Rectal adenocarcinoma is a malignant tumor that is dangerous because in the early stages it does not cause discomfort and does not show obvious symptoms of the disease. Adenocarcinoma consists of glandular epithelial cells that line the walls of the rectum. The disease is also called glandular cancer, this pathology is a type of colorectal cancer. In terms of frequency of diagnosis, this disease ranks third among gastrointestinal cancers.
Adenocarcinoma - what is it?
Adenocarcinoma of the rectum (ICD code 10 - C20) is considered the most common type of malignant tumors of the rectum. This pathology is more common among the male population than among women. More often appears after 45 years. Atypical cells divide quite quickly and cause destruction of the tissues that make up the tumor.
Adenocarcinoma begins to metastasize early to nearby and distant organs, which causes early death - after the onset of pathology development within a year.
Why does the disease appear?
Rectal adenocarcinoma is a fairly common malignant tumor among other cancers. The main reason lies in the hereditary factor. If close relatives have been diagnosed with such a disease, there is a high probability of developing a malignant tumor in any representative of this genus.
The influence of external factors cannot be excluded. The reasons may be as follows:
- chronic diseases of the colon, the presence of ailments such as hemorrhoids, fistula, colitis, polyposis;
- a favorable environment for the development of cancer cells is created by diffuse polyposis and Gardner and Turcot syndrome;
- people over 50 years old;
- frequent constipation;
- long-term use of certain medications;
- papillomavirus;
- improper diet, which is high in fat and low in fiber;
- exposure to stress and depression;
- overweight;
- bad habits.
The exact causes of the disease have not yet been established by medical science. Only factors that contribute to the development of the disease have been identified.
Leading clinics in Israel

Assuta
Israel, Tel Aviv

Ikhilov
Israel, Tel Aviv

Hadassah
Israel, Jerusalem
Complications
Adenocarcinoma of the sigmoid colon is characterized by a slow progression. However, the pathology is asymptomatic for a long time, which is why treatment begins in a difficult situation. Glandular cancer can cause serious complications, including death.
Large formations block the intestinal lumen, causing intestinal obstruction. This condition requires urgent surgical intervention. In addition, with colorectal cancer, frequent diarrhea is replaced by persistent constipation, as a result of which the walls of the large intestine are injured by solid feces.
As the tumor grows, it can rupture the wall of the affected intestine. This is dangerous due to the development of peritonitis, when intestinal contents enter the abdominal cavity.
The disease also leads to anorexia due to loss of appetite, heavy bleeding causes anemia. If left untreated, death occurs several months after the appearance of metastases.
Causes of the disease
The exact causes of the pathology are not clear; more often the disease is diagnosed in patients who have relatives with oncological pathologies of the gastrointestinal tract.
Another risk factor is frequent consumption of foods with high levels of animal fat and fiber. Other factors that can cause the development of pathology in the rectum are:
- hereditary diseases (diffuse polyposis, Turcot and Gardner syndromes);
- chronic intestinal diseases (rectal fissures, fistulas, hemorrhoids, polyps, colitis). Precancerous conditions include ulcerative colitis and Crohn's disease;
- anal sex;
- prolonged constipation;
- frequent stress;
- prolonged use of certain types of medications;
- presence of HPV (human papillomavirus);
- long-term contact with harmful substances (amides, asbestos, tyrosine) in production;
- diabetes;
- age after 50 years;
- sedentary lifestyle, obesity;
- drinking alcohol and smoking.
Symptoms and diagnostic signs
In addition to the general symptoms given above, you can add signs of an advanced stage of the disease:
- the tumor is palpable through the abdomen;
- there is a suspicion of peritonitis;
- when obstruction develops, the patient experiences vomiting of feces, cessation of gas discharge, and intense pain;
- accompanied by weakness, weight loss;
- Intestinal bleeding is often observed.
The most significant and informative diagnostic methods are:
- tumor markers;
- biopsy;
- histological studies;
- different options for endoscopy.
Identification of tumor markers are substances that naturally increase in concentration with a certain type of cancer; they are determined in venous blood. For intestinal cancer, it is determined:
- presence of tumor cells marker CA 19-9 and CEA for suspected rectal cancer;
- carcinoembryonic antigen.
Carrying out endoscopic examinations with the introduction of a sigmoidoscope, a fibrocolonoscope into the rectum, a laparoscope into the abdominal cavity, as well as the ability to examine tissue urgently during surgery gives clinicians a way to establish moderately differentiated growth of glandular cells. Suitable for cytology:
- fragments of fabric;
- imprints of the removed mucous membrane;
- purulent and mucous discharge.
The conclusion indicates the type of tumor as well- or low-differentiated adenocarcinoma of the colon or small intestine.

During a colorectal examination, the cancerous tumor is examined and a piece of tissue is removed for cytology.
Adenocarcinoma of the large intestine also differs in its histological structure; they are distinguished:
- dark cell tumor;
- mucinous;
- cancer without classification.
Types of adenocarcinoma
Colorectal cancer is divided depending on the homogeneity of the formation. Each type has its own characteristics:
- highly differentiated adenocarcinoma of the rectum has a slightly changed cellular composition of the neoplasm. An increase in the size of the nuclei is observed, the cells can continue to perform their functions. Elderly patients do not have metastases or tumor growth into other organs. Young patients are at greater risk with this disease - they may experience a relapse after a year. Diagnosis is difficult due to its high similarity to normal cells. This subgroup of pathology responds well to treatment - after therapy, 97% of patients experience remission. The tumor has a low degree of malignancy;
- moderately differentiated rectal adenocarcinoma does not have such a positive prognosis. The pathology is accompanied by complications in the form of the appearance of fistula tracts and the development of peritonitis. Large neoplasms often break through the intestinal walls, causing severe bleeding. With this pathology, the prognosis after surgery or other treatment is often positive;
- poorly differentiated adenocarcinoma of the rectum . Dark cell tumor has an aggressive course. The spread of metastases to nearby organs occurs several times faster. There is a pronounced polymorphism of cells. If this type of adenocarcinoma is present, the survival prognosis is poor. Poorly differentiated adenocarcinomas are represented by the following types of cancer; mucous (colloidal). The main symptom is strong mucus production;
- squamous;
- mucocellular (ring cell), which affects young people;
- glandular-squamous. This type of malignant tumor is the least diagnosed;
Tubular adenocarcinoma. This pathology consists of tubular connections, is of medium size and has unclear boundaries. Almost 50% of patients with colorectal cancer suffer from this type of pathology.
Degrees of differentiation
The level of differentiation of intestinal adenocarcinoma provides information about the degree of transformation of glandular epithelial cells and indicates the ratio of malignant and benign cells present in the tissues. The classification of differentiation includes four points:
- Highly differentiated option.
- Moderately differentiated form.
- Poorly differentiated type.
- Undifferentiated cancerous tumor.
The highly differentiated variant is characterized by a more favorable outcome than other types. With this form of the disease, there is no change in cell structure. The increase occurs only in the nuclei. Oncological cells are still similar to healthy ones and perform their functions. This form of the disease is characterized by a favorable outcome. In 98% of cases the patient can be saved.
The moderately differentiated form worsens the prognosis. In this case, rectal adenocarcinoma is cured in 75%. The indicators are encouraging, and yet the percentage of those recovered is declining. This form can be cured mainly surgically or under the influence of radio waves.
The poorly differentiated type is a severe illness, the favorable outcome is sharply reduced. This type of disease is called mucous cancer, since the development of the disease increases the production of secretions. The tumor in this disease grows very quickly. Malignant tumors quickly metastasize. Often this form of the disease leads to death. Therapeutic intervention rarely brings relief.
The undifferentiated type of the disease is accompanied by the formation of pathological malignant cells, which metastasize to the lymph nodes. The outcome of the disease is rarely favorable.
Stages of disease development
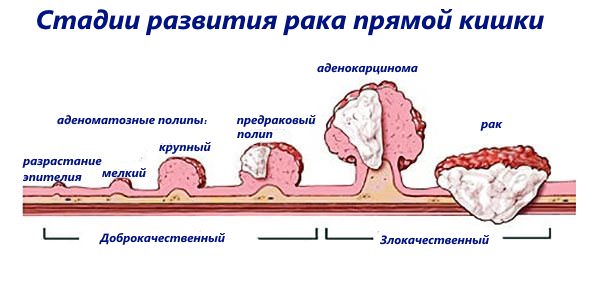
The development of rectal adenocarcinoma is divided into the following stages:
- Stage 1 - characterized by a small tumor size, mobility and distinct boundaries. The mucous and submucosal layers of the organ are more susceptible to damage;
- Stage 2 of the disease is divided into two substages: substage 2A. At this substage, there are no metastases, tumor cells do not spread beyond the walls and lumen of the intestine. The size of the tumor can be up to half of the mucosa.
- 2B substage. The tumor is usually small in size, but there are metastases.
- 3A substage. Deep germination of cancer cells is observed; not only the intestinal walls, but also the peri-rectal tissue are involved in the process. Rare foci of metastases in the lymph nodes can be diagnosed. The size of the tumor itself occupies more than half the diameter of the intestine.
Don't waste your time searching for inaccurate cancer treatment prices
*Only upon receipt of information about the patient’s disease, a representative of the clinic will be able to calculate the exact price for treatment.
Stages
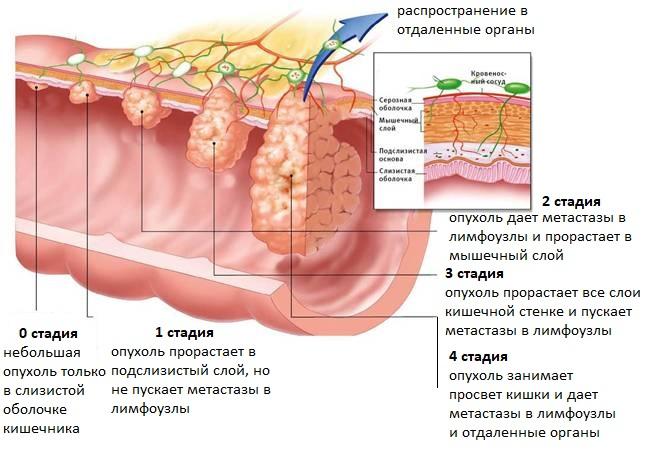
Rectal adenocarcinoma is divided into four degrees of severity, called stages. Each stage has characteristic features:
- In the first stage, the mucous and submucosal layer of the intestinal walls is affected. At this stage of development, pathology is detected very rarely, since it almost always passes without any symptoms. Only if a person consults a doctor because of some other illness, the doctor may suspect the presence of a tumor and refer the patient for a more detailed examination.
- The second stage is divided into two substages. At stage 2A, the tumor infiltrates into the muscle tissue and blocks the intestinal lumen by one centimeter, but does not yet affect the lymph nodes and nearby structures. In stage 2B, the intestinal lumen is blocked by more than one centimeter. At this stage, most patients develop chronic constipation, and streaks of blood, mucus and pus can be found in the stool.
- Doctors also divide the third stage into two. Stage 3A is characterized by tumor growth through the entire thickness of the intestine and blocking the lumen by more than one centimeter. At the same time, the lymph nodes remain healthy. If a person is diagnosed with stage 3B, this means that the neoplasm has metastasized to regional lymph nodes and has grown into the tissue of the outer serous membrane, which contains a lot of nerve endings. That is why only at stage 3B do patients begin to complain of severe pain and go to the doctor for the first time.
- The fourth stage is the last and is fatal. The tumor grows to enormous sizes, infiltrates into any nearby structures and metastasizes to distant organs.
The earlier the oncological process is detected, the greater the chance of curing the patient.
Symptoms of the disease
In the early stages of the disease, adenocarcinoma is not accompanied by an obvious clinical picture.
When a tumor grows into surrounding tissues and when the intestinal lumen is blocked, the following signs may appear:
- aching or sharp abdominal pain;
- severe weight loss;
- disorders of the defecation process - constipation, which is replaced by diarrhea, pain when going to the toilet;
- aversion to food (usually meat dishes);
- anemia (dizziness, pale skin);
- increasing aches and weakness;
- the presence of mucus and blood clots in the stool;
- sustained hyperthermia;
- flatulence and bloating.
When the cancer process spreads to other organs, other signs appear, for example, disruption of the urination process.
The growth of a cancerous tumor can cause increased production of mucus; its accumulation causes painful tenesmus - an increased urge to defecate (up to 20 times per day).
When a malignant tumor begins to disintegrate, blood and pus enter the stool, which emit a foul odor.
What's happened
Adenocarcinoma, or glandular cancer, occurs mostly without symptoms at an early stage of development. For this reason, it can be detected already at later stages of formation, which significantly complicates the treatment process and reduces the likelihood of a complete recovery.
The tumor is localized in areas of accumulation of glandular tissue lining the inner surface of the intestinal walls.
In most cases, adenocarcinoma is detected in elderly people over the age of 60, especially in those who live in areas of unfavorable environmental conditions.
Adenocarcinoma is one of the types of carcinoma, since it begins to develop from the glandular epithelial layer.
Establishing diagnosis
Diagnosis begins with an initial rectal examination and medical history. The following examination methods are:
- blood test - general, biochemical, for tumor markers;
- stool test for the presence of occult blood;
- PET, CT, MRI, scintigraphy. They help clarify the location and features of the histological structure of the tumor, identify signs of the development of metastases;
- transabdominal or endorectal ultrasound;
- irrigoscopy. It is carried out using a contrast agent, which is introduced into the body orally or using an enema;
- colonoscopy;
- sigmoidoscopy. It allows you to conduct a visual examination of the organ mucosa and perform a biopsy of the tumor.
Video on the topic:
Forecast
It is necessary to make further predictions taking into account a number of certain factors - the stage of the disease, the age category of the patient, the state of the immune system and other characteristics of the human body.
When a pathological process is diagnosed at the beginning of its development after surgery, life expectancy for 5 years is observed in 90 percent of cases. If the disease is detected at stage 2, the survival rate is about 70%.
When lymph nodes and distant anatomical structures are affected, 5-year survival is observed in 50 and 10 percent of patients, respectively.
Treatment of pathology
Due to the early appearance of metastases, the prognosis of the disease will depend on timely and correct treatment.
The treatment regimen is selected taking into account the location of the tumor and the general health of the patient. The degree of differentiation of cancer cells plays a significant role. The best treatment effect comes from combination therapy. The complex of therapy includes: radiation and chemotherapy, surgery.
When treating moderately differentiated adenocarcinoma and low-grade adenocarcinoma, strong radioactive irradiation and a high dosage of toxic drugs are required. Surgery is considered an effective method of treatment. The doctor performs excision of neoplasia, as well as tissues that have been affected by metastases.
When adenocarcinoma is located very close to the anus, radical measures are used to excise the affected area along with the sphincter apparatus. After excision, an artificial opening is formed for the removal of feces - a colostomy, which involves attaching a colostomy bag; it should be changed periodically.
A malignant tumor cannot always be removed through surgery. For some patients, surgery is contraindicated for health reasons and advanced age. In this case, one of the methods of palliative medicine therapy is used.
The use of chemotherapy is generally considered an adjuvant treatment to achieve a greater therapeutic effect. A number of combinations using cytostatics are used to treat rectal tumors. The following drugs are commonly used:
- "Capecitabine";
- "Ftorafur";
- "Leucovorin";
- "Fluorouracil";
- "Raltitrexid";
- "Irinotecan".
Radiation therapy is used before or after surgery. Before surgery, the use of this method helps to reduce the size of the node and slow down the process of metastases.
When a patient is diagnosed with glandular cancer, the use of this technique is contraindicated.

Would you like to receive an estimate for treatment?
*Only upon receipt of data on the patient’s disease, a representative of the clinic will be able to calculate an accurate estimate for treatment.
Treatment options
After all tests and studies, the disease is treated. The main method is surgery and is determined by the size of the tumor, the classification of adenocarcinoma and the type of structure of atypical cells. Small tumors are removed by resection. Laparoscopy is a gentle method of removal, in which several punctures are made in the peritoneum. If the carcinoma is large enough to metastasize to the large intestine, part of the digestive tract is removed—a colectomy is performed. To remove feces, a colostomy is created, an outlet for a colostomy bag.

The preparatory stage before surgery is chemotherapy, which reduces metastases.
Chemotherapy and radiation are used in the preparatory stage before surgery to reduce metastases. Drug treatment, as a rule, is not used, except for the prescription of painkillers. Before surgery, a number of procedures are required:
- cleansing the intestines with the drug "Fortrans";
- special slag-free diet based on mixtures “Resurs”, “AF”, “Optium”, “Peptamen”;
- hydrocolonotherapy;
- enemas.
Consequences of the disease
Rectal adenocarcinoma metastasizes more often to nearby lymph nodes. This is followed by the involvement of bone tissue, uterus, liver, bladder, and kidneys in the tumor process. Lastly, they are observed in the lungs and brain.
Glandular cancer can provoke a number of severe complications, the following may occur:
- bleeding;
- anemia;
- intestinal obstruction (ranging from relative to complete obstructive);
- inflammation of the peritoneum and subsequent development of peritonitis;
- perforation (rupture) of the rectal wall due to tumor growth.
What does colon cancer look like?
Doctors at the Yusupov Hospital collect material from a rectal tumor during an endoscopic examination or surgery and send it to the histology laboratory. Laboratory assistants determine the histological type of the tumor based on what colorectal cancer looks like.
Rectal adenocarcinoma consists of atypical cells that originate from glandular epithelial tissue and are formed into tubular, papillary and other structures. The cellular structure can have varying degrees of differentiation: highly differentiated neoplasms have cytological signs of maternal epithelial tissue, and poorly differentiated adenocarcinomas only vaguely resemble the original material. They are highly aggressive, grow and spread faster.
Mucous adenocarcinoma is a group of cells that are surrounded by mucus. Tumors of the mucous type can be poorly differentiated and highly differentiated. Mucus accumulates in tumor structures in the form of “lakes” of varying sizes
Signet ring cell carcinoma gets its name due to the shape of the cells, which, due to an excess of mucus in them and the displacement of nuclei towards the membranes, take on the appearance of a ring. The mucous substance that occupies the space of cells is a specific protein mucin. Signet ring cell tumors of the rectum are quite aggressive.
Squamous cell carcinoma of the rectum consists of atypical cells. They belong to the squamous intestinal epithelium. Pathological lesions contain intercellular bridges and keratin. Rectal squamous cell tumors can be keratinizing or non-keratinizing.
Glandular squamous adenocarcinoma is a rare type of rectal cancer. Such neoplasms are represented by adenocarcinoma, in combination with squamous cell carcinoma. Under a microscope, histologists see small fragments of squamous cell transformation.
Undifferentiated rectal tumors consist of atypical cells of epithelial tissue that do not form glandular structures and do not produce mucus. These cells represent different cytological structures. They form sheets or cords that are separated by a scant stroma of connective tissue.
Scirrhus is a cancerous tumor in which the connective tissue predominates over the stroma. Cytological structures in scirra are cubic cells collected in strands or small cells. Sometimes there are neoplasms in the rectum that do not fit into any histological type. In this case, oncologists talk about unclassified rectal cancer.
Neuroendocrine tumors of the rectum originate from cells of the diffuse neuroendocrine system. They have a well-developed fibrous stroma and are histologically different from adenocarcinomas.
Diet for adenocarcinoma
Before surgery, the patient is advised to eat well to maintain a weakened body. You should also strengthen your immune system with foods that are rich in vitamins.
The diet should be varied; salty, fried, fatty, spicy foods, as well as foods that cause fermentation and increased gas formation, should be excluded from the diet. You should eat small portions a day up to 6 times.
After excision of the tumor, do not eat anything on the first day. Next, all food is offered to the patient in liquid form; the volume of water per day should not be less than one and a half liters.
Treatment
Treatment of rectal adenocarcinoma is selected individually and depends on the degree of tumor differentiation, the stage of development of the oncological process and the general condition of the patient. In therapy, various techniques are used to get rid of the tumor. Treatment can be carried out through surgery, chemicals, and radiation. The combination of these methods is most effective in the fight against glandular colon cancer.
The most effective treatment for adenocarcinoma is surgery, during which doctors remove the tumor and the affected area of the intestine itself, as well as the sphincter apparatus. A colostomy (an artificial opening for stool waste) is immediately removed through the abdominal wall, to which a colostomy bag is attached. Before and after the operation, the patient undergoes several courses of chemical and radiation therapy.
If the patient’s advanced age or weakened condition prevents the operation, then palliative treatment is necessary, aimed at reducing pain, improving the quality and length of life. In this case, doctors perform electrocoagulation of the tumor (cauterization with electric current), as well as:
- Chemotherapy is the introduction of a cytostatic drug into the patient’s body, for example, Irinotecan or Fluorouracil. In some cases, it is necessary to use a complex of chemical drugs.
- Radiation therapy - since the rectum, unlike other parts of the intestine, is rigidly fixed in its place, a strictly specified area is subject to irradiation.
We recommend reading: What is osteoma of the frontal sinus, its treatment and symptoms
After such therapy, a large, inoperable tumor may become smaller in size, allowing doctors to perform surgery to remove it.

Meals for rectal cancer should be fractional (five or six times a day in small portions) and contain a sufficient amount of vitamins and useful elements.
With this disease, it is unacceptable to consume alcohol, spicy, fatty, fried and too salty foods, as well as foods that cause fermentation and increased gas formation.
When installing a colostomy, the patient should not eat anything at all on the first day after the operation; further nutrition should be in semi-liquid form and no more than two kilograms per day. The amount of liquid you drink per day should not exceed one and a half liters.
Disease prevention
For early diagnosis of the disease and prevention of its development, it is recommended to follow these rules:
- upon reaching 50 years of age, you should undergo a mandatory examination by a coloproctologist at least once a year;
- treat inflammation and polyps in the intestines in a timely manner;
- if you have relatives suffering from adenomatous polyposis, screening should be done after 20 years of age;
- exclude spicy foods and foods high in fat from the diet. Eat more fruits and vegetables to normalize intestinal function and relieve constipation;
- follow a healthy lifestyle.
Video on the topic:
Diagnostics
At an early stage, computer or magnetic resonance imaging allows an accurate diagnosis to be made. Metastases are also detected using these methods. Instrumental methods include colonoscopy, laparoscopy, rectomanoscopy, and fibrocolonoscopy.
In addition, an ultrasound examination and biopsy of the tumor formation are performed. Fluoroscopy with a contrast agent detects polyps, ulcerative lesions, and neoplasms on the walls of the large intestine.
The patient must also undergo a general blood test. A reduced hemoglobin level indicates anemia, which can occur with glandular cancer. Elevated haptoglobin can also signal the disease. A high level of urea indicates a high probability of intestinal obstruction and colorectal cancer.
Treatment and metastasis
The choice of treatment method depends on the size of the tumor, the presence of metastases and the extent of tissue damage. The following methods exist:
- Radiation therapy. Slows down the development of tumors, destroys primary and secondary tumor foci.
- Neutron therapy. A new type of irradiation based on the use of neutrons penetrating deep layers of tissue. Before irradiation, a substance that absorbs neutrons is introduced. Healthy tissues are not injured during this treatment.
- Chemotherapy. Drugs that suppress the growth and metastasis of tumors (Vinblastine, Cisplatin) are administered intravenously or orally.
- Surgery. The operation is performed to eliminate small tumors that do not penetrate into surrounding tissues and do not have metastases. In advanced forms of the disease, surgical interventions are used to restore intestinal patency.
Good results are observed with the simultaneous use of several treatment methods.
Causes
To consider the causes of adenocarcinoma, we will highlight the general part that is characteristic of any localization of neoplasms. We will consider the most typical risk factors in specific cases.
It was found that tumor degeneration of glandular cells can be caused by poor nutrition with increased consumption of:
- animal fats from meat, butter;
- excesses of sweets;
- fried, smoked, spicy dishes;
- alcoholic drinks.
At the same time, the diet does not have enough:
Risk factors include:
- tendency to constipation;
- intestinal polyps;
- chronic inflammation (colitis, enterocolitis);
- hereditary predisposition;
- low quality of drinking water;
- long experience of working with occupational hazards;
- presence of papillomavirus;
- passion for anal sex.
Symptoms of adenocarcinoma
In most cases, this type of cancer develops quite slowly. For a long time the patient does not notice any changes in his condition.
Important: adenocarcinoma is often a consequence of a chronic inflammatory process in the intestinal wall, and the first manifestations are often mistaken for an exacerbation of a long-existing pathology.
Unfortunately, the neoplasm is usually diagnosed at late stages, when single or multiple secondary lesions have already formed. This circumstance significantly complicates treatment and reduces the patient’s chances of a full recovery.
Early clinical signs:
- pathological impurities in feces (blood and mucus are found in 90% of cases);
- Irregular bowel movements (constipation).
Later symptoms:
- pain in the abdominal area (dull, aching character);
- increased fatigue;
- general weakness;
- weight loss due to normal nutrition;
- loss of appetite;
- low-grade fever for no apparent reason;
- alternating diarrhea and constipation;
- changes in the nature of stool and the appearance of a putrid odor during bowel movements;
- frequent tenesmus (false urge to have a bowel movement);
- jaundice (with metastases in the liver and gall bladder).
The intensity and duration of painful attacks increases as adenocarcinoma grows. Anemia appears against the background of intoxication and chronic bleeding.
Important: if the lower sections are affected, the blood on the surface of the feces has a bright scarlet color. With a higher localization of the tumor, the blood is dark. If the tumor is located on the right side of the intestine, the bleeding may be hidden.
Weight loss is caused by a disruption in the flow of digestive enzymes into the intestinal lumen and a decrease in the absorption of nutrients.
The cause of hyperthermia (within subfebrile values) is the reaction of the immune system to a pathological neoplasm. The process of adenocarcinoma disintegration can be accompanied by a rise in temperature to 38°C and above.
If the tumor closes the intestinal lumen, fecal retention occurs, which is accompanied by the appearance of nausea and vomiting (against the background of general poisoning of the body). At the same time, there is also an increase in the intensity of the pain syndrome.
The waste products react with the tumor, causing it to ulcerate and become infected. A sign of such a complication is the presence of pus and dark blood in the stool.
When the tissue of the retroperitoneal region is involved in the inflammatory process, a symptom such as tension and intense pain in the muscles of the lumbar region appears.
Causes and predisposing factors of progress
One of the main reasons, according to the results of a study by oncologists, is the hereditary (genetic) predisposition of the sick person himself. But there are a number of factors that can trigger a surge in this disease or increase the risk of accelerated development of a cancerous tumor:
- Elderly age.
- Chronic diseases of the rectum.
- Already existing benign tumors.
- Constant contact with substances containing toxic reagents (including medications).
- Infectious papilloma virus.
- Physical injuries.
- Constant stress.
It is these factors that can contribute to faster growth of a cancerous tumor.
Typology
Adenocarcinomas differ in the morphological, cytochemical and functional characteristics of cancer cells, which are determined by the results of histological examination.
Classification of intestinal adenocarcinoma:
- Highly differentiated. Pathologically altered cells show a slight increase in nuclei. Appropriate therapy has a positive effect, and complete recovery is possible. Young people are at risk of relapse within a year. In elderly patients, the risk of tumor recurrence after removal of well-differentiated colon adenocarcinoma is 50%. The prognosis for life is favorable.
- Moderately differentiated. Cancer cells are prone to growth, which is dangerous due to obstruction and rupture of the intestinal lining. High probability of developing inflammation of the peritoneum. With timely treatment and tumor resection, the 5-year survival prognosis is positive.
- Poorly differentiated. Rapid proliferation of cancer cells and early metastasis occur. The tumor boundaries are not visualized during diagnostic procedures. Difficult to treat.
- Undifferentiated. As a result of histological examination, pathological cells atypical for cancer are detected. It grows into the peritoneum and early metastasizes into the lymphatic system. If undifferentiated intestinal adenocarcinoma is detected, the prognosis for life is negative.
Types of glandular cancer by cell type:
- mucinous adenocarcinoma - rare, consists of nodes interspersed with mucus (mucin), which makes up the majority of the tumor;
- signet ring cell adenocarcinoma - cancer cells are prone to rapid division, the accumulation of intracellular mucus leads to their deformation;
- squamous cell adenocarcinoma - often recurs, grows into neighboring organs;
- tubular adenocarcinoma is the most common form, characterized by structural proliferation and atypical cell structure.
Reference! Adenocarcinomas form inside and outside the intestine (endophytic and exophytic). An endophytic tumor is sometimes detected by palpating the peritoneum. Internal neoplasm leads to intestinal obstruction.
A little about the intestines and the cells that cause the disease
The human intestine is divided into 2 sections: thin and thick. The connection with the stomach begins with the subtle. There are:
Here the maximum number of enzymes is located, the breakdown and absorption of nutrients is carried out. Everything needed is absorbed into the blood. The large intestine ensures the accumulation and reabsorption of water, the formation of a mass of toxins, and their removal from the body. He shares:
- to the cecum with a vermiform appendix (appendix);
- colon with four parts (ascending, transverse colon, descending, sigmoid and rectus).
The final segment is the rectal ampulla, anal canal and anus. Glandular cells are located on the mucous membrane of all parts. They are wedged between the epithelium and are absent at the tips of the villi. In total, they constitute up to 9.5% of the cellular composition of the small intestinal mucosa, the concentration increases as it approaches the thick section. They differ from their neighbors in their ability to produce mucus, which is necessary to protect the wall from passing feces.
After secretion is released into the intestines, they again become prismatic. Malignant degeneration is characterized at first by slow growth into the intestine (endophytic growth) or outward (exophytic), then by a rapid transition to metastasis through the vessels to the nearest lymph nodes, lungs, liver and other organs.
The most severe course is observed at a young age. This is explained by anatomical changes in blood vessels in people over 40 years of age: the lumen decreases, the activity of transferring metastases is less pronounced. And up to 30 years of age, the intestine has a pronounced vascular and lymphatic network, which provides a high risk of metastasis.










