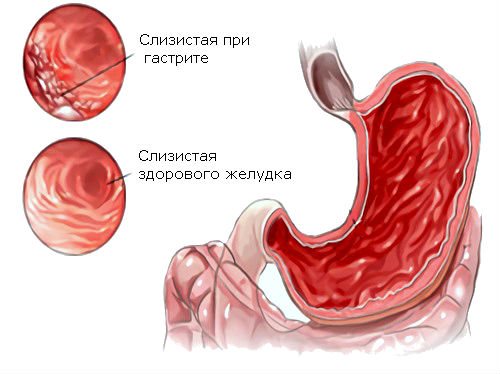
Gastritis is a common stomach disease, affecting 95% of people. The main reason is poor nutrition, spicy, fatty, hot foods, snacks. Pathology, as a rule. begins in adolescence. Gastritis is a disorder of the gastric mucosa; obvious symptoms are heartburn, nausea, unpleasant taste in the mouth, and dull pain. There are two types of disease: acute and chronic. Doctors say that it is easier to protect yourself from the disease in time; it will take years of treatment to cope with the disease.
Pancreatitis is a consequence of disturbances in the functioning of the pancreas. The first sign of the disease is vomiting and the formation of an aversion to fatty, spicy foods. Then such products stop being absorbed and come out. Nausea is common, but it is vomiting that indicates the severity of the disease. The second sign is an intestinal disorder that is unable to digest foods, resulting in diarrhea. The third sign is pain in the abdomen, localized in the left hypochondrium.
Features of treatment
The bacterium Helicobacter causes gastritis; a person becomes infected already in childhood. Treatment of gastritis involves gastroscopy, which is done under anesthesia; the procedure takes 5-10 minutes to check for Helicobacter. Normalization of nutrition is an important process in the treatment of gastritis. Medications are indicated; the medications will be prescribed by the attending physician, based on the examinations and tests performed.
Pancreatitis cannot be neglected; severe consequences are likely, including death. Treatment of pancreatitis primarily involves eliminating alcohol. At the diagnostic stage, a blood test and stool test will be required. Enzyme preparations are prescribed. When medications enter the body with food, the pancreas rests. Secretolytic drugs that reduce the acidity of gastric juice are important. The main factor that causes the pancreas to produce juice is acid. Antispasmodics help relax the walls of the duct and mouth. Mineral waters for treatment must have an alkaline composition.
Cholecystitis is inflammation of the gallbladder. A symptom of cholecystitis is pain under the right rib. Treatment is mainly done with antispasmodics and antibiotics. Proper nutrition will help get rid of the disease.
Inflammation of the gallbladder
Before treating the mentioned diseases, it is necessary to determine the causes that contributed to the appearance and development of the diseases.
Special procedures will help recognize the disease:
- Carrying out computer diagnostics.
- Fibrogastroscopy is necessary to exclude pathology from the stomach and duodenum.
- An endoscopic examination will help identify cancer.
- Ultrasonography.
Diagnostic methods
In order to determine which pathological process is developing in the patient’s body, qualified specialists can prescribe the following additional diagnostic methods:
- taking blood tests for clinical and biochemical studies,
- Ultrasound, MRI, or CT,
- carrying out endoscopy in combination with a biopsy, which will help to obtain information about the condition of the mucous membranes of the gastrointestinal tract,
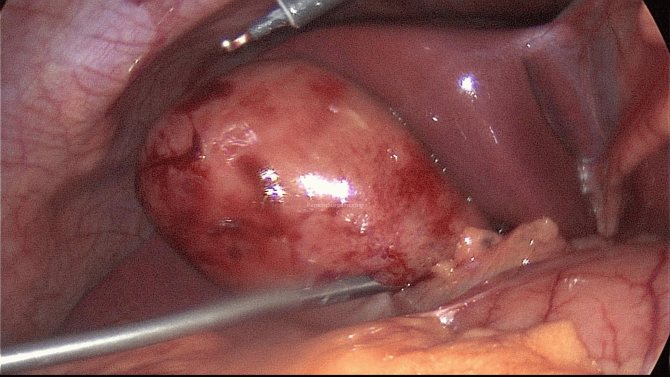
- in some cases, laparoscopic diagnosis may be necessary to determine the acute form of pancreatic disease.
It is important to remember that the course of acute pancreatitis is often a surgical emergency that can dramatically worsen the patient’s condition, and surgical intervention will be simply necessary. Therefore, if during the development of this pathology it suddenly becomes worse, it is highly not recommended to delay a visit to the doctor.
Bibliography
- Vinogradov A.V. Differential diagnosis of internal diseases, manual, 2001.
- Grigoriev P.Ya., Yakovenko A.V., Clinical gastroenterology, 1998
- Gubergrits N.B., Ostroukhova I.N. The severity of Helicobacter pylori infection in patients with chronic pancreatitis. Russian Journal of Gastroenterology, Hepatology and Coloproctology. 2002 No. 5 p. 70.
- Zhukova EH Comparative assessment of various diagnostic criteria for exacerbation of chronic pancreatitis. Russian gastroenterological journal 1998 No. 1.
How to distinguish gastritis from pancreatitis
The symptoms of the two diseases are similar due to the close location of the organs. It is quite possible to recognize gastritis - pain in the stomach, nausea, pain after eating. With pancreatitis, pain in the hypochondrium, stool disturbances, and diarrhea with a foul odor occur. Symptoms noticeable to the patient are given. The attending physician is required to carry out a number of procedures to determine the cause, localize the pain, collect tests, conduct an examination - to understand the cause and prescribe treatment.
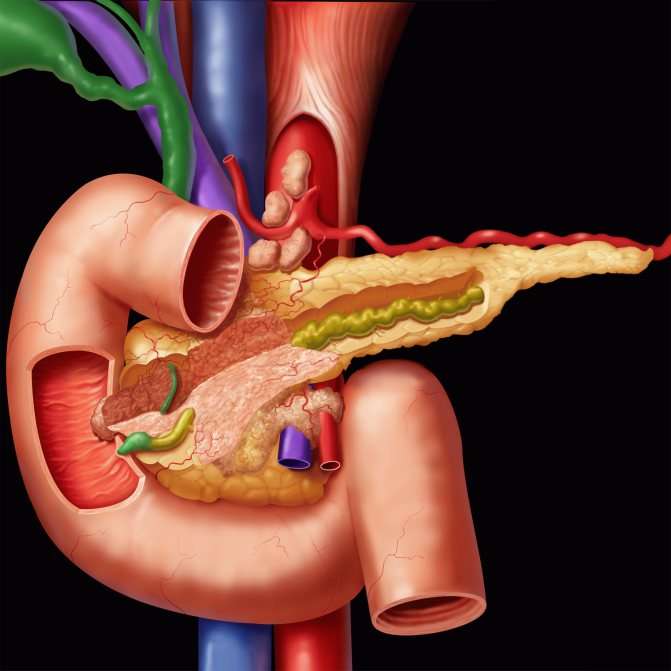
The organs of the gastrointestinal tract are interconnected, have a similar origin, similar symptoms, but can differ.

Organs of the gastrointestinal tract
There is a difference in the treatment of diseases, different examination methods are used, different drugs are prescribed.
It is important to start treatment of the gastrointestinal tract on time. Every person needs strength and energy to work, study, and simply live. We take energy from food, including vitamins and minerals - elements of normal functioning. When difficulties arise in the gastrointestinal tract, human life is poisoned and other organs cease to function normally. Disturbances appear in the immune system.
Etiology of parallel development of diseases
As you can see, there are signs of gastritis and pancreatitis at the same time. But why do both diseases affect a person at once? Chronic gastritis and pancreatitis develop due to the same provoking factors:
- poor nutrition;
- alcohol abuse;
- stress.
Since food enters the stomach first, this organ is the first to suffer. The mucous membrane becomes inflamed. Due to the lack of treatment, chronic gastritis develops, which can only occasionally bother the owner, so serious measures are not taken.
Constant inflammation disrupts the acid balance. Excess acid does not allow food to be fully digested. As a result, the pancreas takes over the issue of undigested food, increasing the amount of enzymes. This, depending on the intensity of the disease, gives rise to an acute or chronic form of pancreatitis.
After this, excess pancreatic enzymes and hormones, supplemented by the contents of the bile duct, enter the stomach, the mucosa of which is further damaged by pancreatic enzymes.
Causes of diseases of the gastrointestinal tract
The main cause of gastrointestinal diseases is poor nutrition. The frantic rhythm does not allow you to eat often and healthily. Preparing the right food takes a lot of time, snacks and quick meals are the way out of the situation for every third person.
Nervous tension, constant stress, overwork, fears can cause disturbances in normal digestion.
Pancreatitis and gastritis are common diseases that can take even children by surprise, so nutritional culture should be instilled in early childhood.
Distinctive features in symptomatic manifestation
Gastritis is a pathological disorder of the inflammatory nature of the course, localized in the area of the mucous membrane covering the stomach. It has two forms of flow - acute and chronic gastritis. During complications of this disease, atrophic processes in this membrane may begin to develop. If the inflammatory process begins to cover the stomach itself and the duodenum, then chronic gastroduodenitis begins to develop. Gastroduodenitis and pancreatitis have the same distinctive features of the course that distinguish gastritis from pancreatitis.
Pancreatitis is a pathological dysfunction of an inflammatory nature, but already localized in the pancreas. Complications of this pathology can lead to the development of necrosis, which occurs during the digestion of areas of glandular tissue by enzymes that the gland itself produces. Necrotic lesions of tissue structures, that is, necrosis, in most cases spreads to nearby organs and tissues. Both chronic pancreatitis and its acute form, characterized by a significant deterioration in general health, can develop.
The first difference between gastritis and pancreatitis is in the area of their localization; gastritis affects the lining of the stomach, and pancreatitis affects the pancreas.
But, due to the fact that these organs of the digestive system are located at a minimum distance from each other, the symptomatic manifestation of pancreatitis and gastritis is very similar in the overall clinical picture. With the development of both diseases, the following is observed:
- constant feeling of weakness;
- increased level of fatigue and excessive sleepiness;
- the skin becomes pale;
- the level of sweating increases;
- body temperature becomes spasmodic and quite often rises to subfebrile levels.

And yet it is possible to distinguish gastritis from the development of pancreatitis. The distinctive symptoms of gastritis are as follows:
- decrease in general appetite, up to its complete loss;
- the occurrence of dull painful sensations in the epigastric region of the abdomen, a burning sensation, heaviness and discomfort, which may become more or less intense after eating food;
- the formation of an unpleasant taste in the mouth, the appearance of belching;
- the occurrence of a feeling of nausea, which often ends with the discharge of vomit, followed by a feeling of relief in the general condition;
- development of diarrhea and constipation;
- feelings of fullness in the abdomen that occur after eating food;
- the appearance of rumbling in the abdominal cavity, as well as bloating.
The degree of manifestation of symptoms in gastritis depends on its nature of the course, the severity and state of concomitant pathological disorders.
The distinctive symptoms of pancreatitis have a slightly different clinical picture:
- Severe pain occurs in the navel area, which, with further development, spreads throughout the entire abdominal area and radiates to the back.
- Complete loss of appetite and bloating.
- Regular discharge of vomit, which is a distinctive symptom of the development of acute pancreatitis. It can appear along with the onset of painful sensations, or immediately after them and last from a couple of minutes to a couple of hours.
- Formation of loose stools with the characteristic appearance of foam, mushy structure.
- With the exacerbation and further development of the pathology, the level of general well-being of the patient begins to deteriorate.

Among other things, acute pancreatitis can be accompanied not only by unbearable pain, but also by an increased level of salivation.
Based on the symptomatic manifestations described above, a qualified specialist will be able to approximately recognize the type of pathological disorder in the digestive system, but additional diagnostic procedures and instrumental research methods will still be required to make an accurate diagnosis.
Consequences of gastritis and pancreatitis
Gastritis will not go away without a trace if you do not approach treatment wisely and carefully. Possible consequences: peptic ulcer of the duodenum, stomach and, worst of all, stomach cancer. A common mistake people make is self-treatment of gastritis with drugs that reduce the concentration of hydrochloric acid in the stomach. Such treatment allows you to relieve pain syndromes, but retains the risk of the disease progressing or developing into a severe stage. When acidity decreases, bacteria spread throughout the stomach and cause inflammation of the walls.
If you have stomach pain, do not suppress it with anti-inflammatory drugs. Many people with mild ailments do not always have the opportunity to immediately consult a doctor, then antacids are recommended to quickly relieve pain. Treatment is aimed at completely destroying the Helicobacter pylori bacterium. Approximately three to four acid-reducing, antibacterial drugs are prescribed. The course of treatment is usually ten to fourteen days. Only modes with many components allow you to achieve the full result.
If a person suspects acute gastritis and pancreatitis, they must immediately call an ambulance, the disease is dangerous! First aid for suspected pancreatitis: application of cold to the abdomen, use of antispasmodics - papaverine, no-spa, do not eat food until doctors arrive. The ambulance provides emergency assistance in the form of a dropper with a physical solution, antiemetic, and pain reliever.
The period of onset of the disease can last ten years, and the person is only bothered by pain some time after eating. With a long course of chronic pancreatitis, the death of organ cells occurs, digestion is disrupted, and diabetes mellitus can develop.
Chronic pancreatitis
Difference between diseases
Gastritis and pancreatitis are completely different diseases. Gastritis is caused by inflammation of the stomach lining. This leads to incomplete breakdown of the products entering the stomach, and disorders of the chemical or mechanical process are recorded.
Thanks to the protective gel produced by the mucous membrane in the required volume, it helps protect the stomach walls from gastric acid enzymes. But when dangerous nutrients and toxins penetrate the organ, the helium barrier is broken, which leads to damage and pathologies.
Pancreatitis is the result of changes in the functioning of the organ. Pathology appears in the acute phase. A painful disorder of the pancreas can develop as a result of poor nutrition, namely the intake of fatty, fried foods, the penetration of toxic elements during smoking, and drinking alcohol. The progression of pancreatitis is also accompanied by:
- gallstone pathology;
- renal failure;
- gastrointestinal diseases.

gastrointestinal diseases
In addition to the fact that diseases affect different organs, the differences between gastritis and pancreatitis lie in the symptoms and consequences of the disease.
In symptoms
How does pancreatitis differ from gastritis, if you look at the symptoms of the diseases? The difference is not only in the place of pain formation and consequences, but also in the features of treatment of gastritis and pancreatitis. The correctness of a certain conclusion is important in choosing a treatment strategy.
It is important to understand that the difference between pancreatitis and gastritis is determined not by the manifestations, but by the genesis of the course. It is quite difficult to distinguish between diseases; even a doctor is not always able to determine the exact disease just by signs. Therefore, an examination is carried out.
Gastritis is a change in the lining of the stomach mucosa, obvious symptoms:
- heartburn;
- nausea;
- vomit;
- unpleasant taste in the mouth;
- dizziness;
- weight in the stomach area;
- diarrhea;
- dull painful discomfort.

heartburn
An external sign of gastritis is determined by a pale face. With exacerbation of gastritis and pancreatitis, the patient feels obvious manifestations of painful discomfort in the stomach area.
Pancreatitis is the result of changes in the activity of the pancreas. Manifestations of the disease are more distinct. An exacerbation is observed after drinking alcohol-containing drinks in a significant amount. Often such signs appear in the peritoneum, the syndrome is sharp and strong. After some time, the syndrome spreads throughout the peritoneum and sometimes spreads to the back.
The first signs of pancreatitis are vomiting, the formation of an aversion to fatty, fried foods. Afterwards, these products are not absorbed, leaving the outside. Unlike vomiting attacks in the presence of gastritis, pancreatic vomiting does not bring relief to the patient and has a continuous or recurring manifestation. The vomiting reflex does not go away, even with an empty stomach. Vomit contents have an admixture of bile, a green or transparent tint.
Afterwards, stool disorder is observed, the intestines are not able to cope with the digestion of food, and diarrhea occurs. Stools with pancreatitis are mushy, foamy, and have a strong, foul odor.
In diagnostics
Pancreatitis with gastritis are considered diseases of the gastrointestinal tract. The signs are similar, which makes it difficult to draw a correct conclusion. It’s bad when diseases develop together. This leads to difficulties in diagnosing the disease and therapy. The painful phenomenon of gastritis and developing pancreatitis are distinguished by symptoms.

diagnosis of the disease
Causes of disease of the gastric mucosa.
- The presence of the bacterium Helicobacter pylori.
- Duodenogastric spasm.
- Alcohol, long-term use of drugs.
- Autoimmune lesion.
Reasons that provoke the development of pancreatitis.
- Mechanical, occurring when enzymes pass through the pancreatic ducts.
- Neurohumoral disorders characterized by difficulties in the production of enzymes and hormones.
- Poisoning of the pancreas.
Although the symptoms of gastritis and pancreatitis are similar, there is a difference in the appearance of pain.
- Discomfort with gastritis appears at the top of the peritoneum, in the solar plexus area. It is dull, aching, has spasms, and leads to colic.
- With pancreatic pathology, the pain is prolonged, severe, often girdling in nature, and occurs under the scapula on the left.
- The painful area when touched is slightly above the umbilical zone.
- The pain begins after eating with gastritis, due to a change in the dietary table. When changes appear in the dietary pattern for pancreatitis, the pain appears after a certain period of time, and after drinking alcohol, generally for a day.

gastritis pain
Only a doctor determines gastritis or pancreatitis based on common symptoms, which often accompany each other. To determine the diagnosis, laboratory and instrumental studies are prescribed.
The doctor collects anamnesis, examines complaints and prescribes the following studies:
- clinical blood test - general symptoms of the body’s inflammatory response;
- biochemical analysis - increase in the activity of amylase, lipase, maybe liver enzymes;
- Ultrasound of the peritoneum;
- endoscopic examination together with biopsy;
- laparoscopy.
Consequences of cholecystitis
Dangerous consequences of cholecystitis occur when bile ceases to be produced, and the risk of gallstones develops. To prevent the formation of stones, it is recommended to eat five times a day at set times. Remember the obligatory condition is not to overeat.
In adults, if cholecystitis occurs, angina pectoris and inflammation in the digestive tract develop. Acute cholecystitis can develop into pancreatitis and hepatitis. Each meal allows a certain amount of bile to be released.
Differences in Pathogenesis
The clinical picture is determined by how exactly the pathological process occurs in both diseases.
Inflammation of the gastric mucosa occurs when:
- infection with the bacterium Helicobacter pylori and the associated direct contact damage to epithelial cells, as well as the influence of the bacterium on the balance of protective and aggressive factors in the stomach,
- duodenogastric reflux ─ reflux of the contents of the duodenum back into the stomach due to poor functioning of the pyloric sphincter. In this case, the mucous membrane is damaged by pancreatic enzymes and other aggressive agents that normally do not come into contact with the stomach. They also change the pH in the stomach, and the stomach performs its functions worse under new conditions,
- prolonged use of medications or other substances (for example, alcohol) that damage the epithelium of the stomach. Many medications have a negative effect on the stomach, but some especially. The latter include, for example, non-steroidal anti-inflammatory drugs,
- the autoimmune nature of the lesion, when the immune system begins to produce antibodies against the lining walls of the fundus of the stomach, gradually reducing the production of acid and digestive enzymes and ultimately leading to atrophy of epithelial cells.
Pancreatitis is based on:
- mechanical damaging factors, most often a violation of the passage of pancreatic enzymes through the ducts into the duodenum. Due to the fact that the main pancreatic duct, together with the common bile duct, opens into the duodenum with one formation - the papilla of Vater (major duodenal papilla), an obstruction may occur at this level as a result of cholelithiasis,
- neurohumoral disorders, namely pathology of innervation, impaired secretion of digestive enzymes and hormones by the pancreas,
- toxic damage as a result of exposure of pancreatic tissue to toxic substances, both those received from outside (alcohol, drugs, poisons) and those formed in the body (pancreatic enzymes themselves, toxins in renal failure).

Lifestyle with gastritis and pancreatitis
The diet is indicated for each of two diseases: pancreatitis and gastritis.
Nutrition
You will have to forget about strong meat broths, exclude mushroom and fish soups. You should avoid fried, salty, spicy, and smoked foods. Prohibited vegetables: radishes, horseradish, sorrel, turnips. Avoiding alcohol is important.
The priority is millet porridge with the addition of pumpkin and berries. It is acceptable to eat white fish, turkey, chicken breast, and anything steamed. Sausages, chocolate, flour, coffee are prohibited. An active lifestyle is important - sports, movement, physical education, exercise - whatever. Move as much and often as possible.
Other aspects of life
A set of exercises for the prevention and treatment of cholecystitis: strengthening the abs, bending over, pulling up, turning left and right. A massage, relaxation, and breathing practice will come in handy. You can go to a sanatorium and receive treatment with mineral waters. Once or twice a year it is necessary to check with a doctor, do an ultrasound examination, take tests, and consult.
Nowadays, it is important to take care of your health: the environment is alarming, products are often stuffed with chemicals and GMOs. More and more people are leaning toward a healthy lifestyle, healthy eating, and quit smoking and drinking alcohol. This is no accident. Many diseases begin to bother people at a young age. They say that diseases are getting younger. To live a happy, bright life longer, you need to have your body examined on time.
If you are experiencing pain, there is a problem in the body, and you need help. At the first signs of imbalance and disharmony in the digestive tract, be it an ulcer, gastritis, pancreatitis, cholecystitis, visit a doctor, do not make a diagnosis yourself.
Popular analogues and substitutes of Pancreatin: the right choice
The lack of effectiveness of the drug, the occurrence of side effects and the presence of contraindications force people with gastritis to look for analogues - inexpensive but effective drugs that will help replace Pancreatin. However, the use of expensive analogues is not always appropriate.
Pancreatin or Creon: which is better?
What is better to take - Pancreatin or Creon - is determined by the doctor based on the diagnosis and symptoms. Minor eating disorders and flatulence from fatty foods and overeating are well removed by cheap Pancreatin. In case of severe diseases - acute pancreatitis, Shwachman-Diamond syndrome, chronic inflammation of the pancreas - the doctor is likely to prescribe Creon due to its specific differences from Pancreatin:
- Pancreatin is activated in the stomach. Active enzymes with high acidity do not always reach the intestines unchanged, which is why their activity decreases. With gastritis, this moment can become critical. Creon is available in gelatin tablets, the activation period of which is somewhat delayed in the stomach. They enter the intestines unchanged and begin to dissolve there, fully exerting an enzymatic effect on proteins, fats and carbohydrates.
- There is more active ingredient in Creon. This may also become a factor in choosing a more expensive drug.
- In the instructions for Pancreatin, the number of accompanying active enzymes is not always indicated precisely, but in Creon this is clearly indicated.
- Price. Pancreatin wins here, since its analogue will cost at least 5 times more.
Creon gelatin capsules have an extended spectrum of action. But its cost is not always justified when treating gastritis. However, when using additional medications, Creon looks like a more advantageous option, since it clearly states the amount of all active ingredients.
Pancreatin or Festal: which is better?

Among the additional features of Festal are:
- Activation of bile production,
- Improvement of all processes in the gastrointestinal tract,
- Can be used before wearing dentures,
- Helps produce gastrointestinal enzymes.
Key contraindications include pregnancy, cholelithiasis and a predisposition to diarrhea.
Doctors recommend alternating the drugs Festal and Pancreatin, since they are almost identical and can replace each other. A comparative analysis of drugs can show that the activity of the components in Festal is much higher. This leads to frequent side effects with regular use. For Pancreatin this figure is significantly lower.
The price of Pancreatin is almost 3-4 times lower than the cost of Festal, which also encourages its use. However, when undergoing treatment with other drugs, Festal is most often prescribed due to its increased enzyme activity.
Pancreatin or Mezim: which is better?
Mezim contains pancreatin and has a similar effect to the drug of the same name. The indications include the same as in the instructions for Pancreatin, including insufficient enzyme activity of the pancreas and gastrocardiac syndrome. The drug is often used for overeating and the treatment of non-infectious diarrhea. Mezim's contraindications are similar to its analogue. Key difference between Mezim and Pancreatin:
- Mezim tablets are 2-3 times more expensive,
- Mezim is produced by a German corporation,
- The exact amount of enzymes stated in Mezim is 4200 IU of amylase, 3500 IU of lipase and 250 IU of protease. The composition of the drug Mezim Forte contains 10,000 enzymes, significantly more,
- Compared to Pancreatin, Mezim has fewer predispositions to contraindications.
Pancreatin and Mezim do not require a prescription, but the enhanced drug requires a prescription from a doctor.
There is no exact answer to the question of what is best for gastritis. It all depends on the individual characteristics of the person. Reviews from patients confirm that both drugs effectively cope with their tasks in certain situations. Doctors say that Mezim has a higher concentration of active substances, so it works faster. But for eliminating mild eating disorders, this parameter is not so significant.










