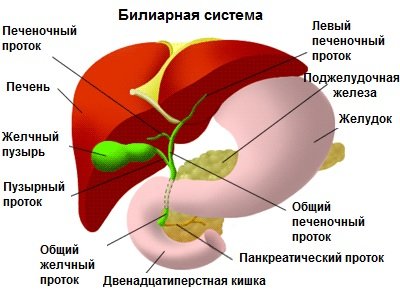
The pancreas is a glandular organ, the length of which does not exceed 7 cm. The location of this anatomical formation is the deep parts of the abdominal cavity. When food components enter the human body, the function of this organ is to produce specialized enzymes that must break down carbohydrates, proteins and fats.
Another (endocrine) function of this anatomical structure is the production of the hormone insulin, which is responsible for the utilization of glucose in the body. Against the background of such chronic diseases as diabetes and pancreatitis, so-called obesity of the pancreas often develops. This serious pathological condition requires timely diagnosis followed by qualified treatment.
Etiology
Currently, the causes of the development of lipodystrophy or lipoatrophy remain not fully understood, but the most likely predisposing factors are considered to be:
- a wide range of metabolic processes in which the metabolism of certain substances is disrupted;
- hormonal imbalance;
- long-term addiction to drinking alcohol and smoking cigarettes;
- poor nutrition – this includes the lack of a food consumption schedule, prolonged refusal to eat followed by overeating, excessive consumption of sweets and fatty foods;
- penetration of parasites, worms or protozoa into the human body;
- viral liver damage;
- long-term use of certain medications for medicinal purposes, in particular hormonal drugs;
- adverse environmental impact;
- occupational hazards, such as frequent contact with chemicals or toxic substances.
Very often fatty degeneration develops in diabetics, which is caused by repeated injections of insulin. In such situations, the severity of the disease will vary from a small depression in the injection area to the total absence of fat in a certain area. The following are considered to be predisposing factors:
- improper administration of a medicinal substance aimed at normalizing the functioning of the pancreas;
- low insulin temperature;
- tissue injury in the area of injection;
- the effect of insulin as a substance that increases lipolysis;
- inadequate response of the immune system to the drug - most researchers are confident that it is the protective reaction of the immune system that leads to atrophy of adipose tissue. In such cases, the body perceives the injection as a threat and reacts to it in a certain way.
In extremely rare cases, lipodystrophy can act as a congenital pathology, the occurrence of which is explained by a violation of the metabolism of adipose tissue caused by genetic abnormalities and inheritance of a mutating gene from one of the parents.
Causes of development of pancreatic tissue dystrophy
The main reason leading to the onset of fat deposits is disturbances in the metabolic reactions occurring in the body.
As a result of the development of the disease, pancreatic cells die. And fat deposits take the place of dying cells.
The body’s implementation of this replacement process allows it to maintain the integrity of the organ.
Most often, this disease is detected in the following situations:
- in case of development of chronic or acute pancreatitis in the body;
- inadequate or incorrectly selected treatment for inflammation detected in pancreatic cells;
- alcohol abuse;
- development of obesity in the body;
- hereditary predisposition.
Most often, progression of the disease is observed in older people. The liver is an organ that, until the age of 40, is able to independently cope with emerging loads, but after 40 years, the body’s reserves are depleted, which leads to the loss of the liver tissue’s ability to cope with emerging problems.
To eliminate the disease, the patient should treat not only the organ that has undergone changes, but also the accompanying disorders and pathologies that provoked the development of the disease.
Fatty infiltration of the liver is a pathological condition in which the organ accumulates lipid tissue and hepatocyte cells begin to degenerate. With timely detection, proper treatment and constant adherence to diet, fatty hepatosis is a reversible process.
Why is healthy cells replaced by fat cells? Doctors identify the following reasons:
- diabetes mellitus type II;
- overweight (body mass index more than 30), metabolic disorders;
- hyperlipidemia is a disease characterized by abnormal amounts of lipids in the blood;
- disruption of the gastrointestinal tract - pancreatitis, enteritis, chronic intestinal dysbiosis;
- endocrine pathologies (hypofunction of the thyroid gland, hyperfunction of the adrenal cortex);
- poor diet, alcohol abuse;
- irregular meals, fasting, exhausting diets;
- taking certain medications, for example: tetracycline, methotrexate, excess vitamin A, estrogens, antiretroviral drugs, long-term antibiotics and without probiotics;
- intense exposure to toxins (gasoline, poisonous mushrooms, pure phosphorus, some pesticides, etc.) and radiation.
In medicine, fatty degeneration can be called steatosis, hepatosis, lipoidosis, steatohepatosis. The disease does not develop due to an inflammatory process. The main change is a large accumulation of adipose tissue in the organ, which becomes overgrown with a capsule.
Fatty degeneration, most often, begins to develop at a more mature age of 45-50 years. The main cause of pathology is considered to be metabolic disorders. Violations occur against the background of various factors.
Liver hepatosis in most men develops due to excessive alcohol consumption. In this case, alcoholic fatty degeneration is diagnosed. A dangerous and frequent complication of the pathology is liver cirrhosis.
Liver damage also occurs due to excessive consumption of energy drinks, drugs, and cigarettes. Many people believe that fatty degeneration occurs only in people who are overweight. This opinion is fundamentally wrong.
Liver hepatosis is often detected in thin people. This phenomenon is explained by protein deficiency in the human body. In this regard, fatty degeneration is typical for vegetarians. People who are addicted to various diets also suffer from this disease.
Fatty hepatosis is accompanied by the following chronic diseases:
- Atherosclerosis;
- Diabetes;
- Chronic hepatitis;
- Viral hepatitis C;
- Dysfunction of the endocrine system;
- Hormonal disorders;
- Pancreatitis.
Other factors can also lead to fatty degeneration. Thus, poor nutrition and low amounts of vitamins consumed negatively affect all organs of the digestive system. Fatty liver develops against the background of frequent intoxication, poisoning, and damage to the body by chemicals.
Pesticides that enter the body along with vegetables and fruits damage the liver. Even some medications provoke obesity of the gland. These include antibiotics and hormonal agents.
Heart and bronchial diseases cause oxygen deficiency. And oxygen deficiency can also serve as a factor in fatty degeneration. Frequent excess of lipids into the gland is considered dangerous.
Lipids settle in the liver, fat droplets accumulate and grow. Small amounts of these components are not dangerous. In this case, hepatocytes have time to process and remove them. The progression of an increase in fat cells leads to the next stage of fatty degeneration - inflammatory hepatitis. Then liver failure and cirrhosis occur.
Classification
The division of the disease depending on the prevalence of the pathological process divides lipoatrophy into:
- generalized - in such cases, the absence of subcutaneous fat is observed only in a certain area of the body;
- diffuse – characterized by the complete absence of adipose tissue. Despite the fact that a person does not look exhausted outwardly, he needs qualified medical care.
Congenital fatty degeneration can occur in several forms:
- lipodystrophy type 1 - caused by a mutation of the AGPAT2 gene, which is located on chromosome 9;
- lipodystrophy type 2 - is a consequence of a mutation in the BSCL2 gene located on chromosome 11;
- lipodystrophy type 3 - formed against the background of a mutation in CAV1, a gene localized on chromosome 7;
- lipodystrophy type 4 - caused by a mutation in the PTRF gene, which is part of chromosome 17.
In addition, there are the following forms of the disease:
- gynoid lipodystrophy - in the vast majority of situations it is diagnosed in females. This type is widely known as cellulite because it is deposited in the abdomen, thighs and buttocks. A special feature is that in other areas adipose tissue may be completely absent;
- hepatic lipodystrophy - a destructive process develops against the background of fatty liver disease, which is also called hepatosis, since it is this organ that is responsible for the breakdown of lipids in the body;
- injection lipodystrophy - in this case, atrophy and lipohypertrophy of adipose tissue is localized where drugs have been injected repeatedly;
- insulin or lipodystrophy in diabetes mellitus.
Forms of the disease
Sugar level
Man
Woman
Enter your sugar or select your gender to get recommendations
Please indicate the man's age
Please indicate the woman's age
At the initial stage of development, the disease does not manifest itself in any way. If fat deposits are located in different areas of the pancreas tissue, there is no compression of the gland and no disruption of cell functionality occurs.
It is for this reason that in the initial stages there are no symptoms indicating the development of a pathological process, and the disease remains undetected for a long time.
The only minor signs that the patient does not always pay attention to are the following:
- Slight increase in body fatigue.
- The appearance of dryness in the oral cavity.
- Formation of small ulcerations on the surface of the mucosa.
With longer progression of the disease, more specific symptoms appear that characterize fatty degeneration of the cells of the glandular tissue of the pancreas:
- persistent feeling of nausea;
- urge to vomit;
- diarrhea;
- girdle pain in the area of the right hypochondrium;
- flatulence.
Simultaneously with degenerative processes in the pancreas, liver hepatosis develops.
In some exceptional cases, a decrease in the patient’s body weight, itching of the skin and severe pain in the peritoneal area may be observed.
We invite you to read: Treatment of diabetes abroad
Patients experience a significant disorder of the gastrointestinal tract, accompanied by the occurrence of dysbacteriosis.
The process of fatty infiltration of the pancreas is a latent disease. This disease is characterized by the occurrence of changes in organ tissues and the formation of fibro-fatty cell formations.
The development of this disease is accompanied by the process of degeneration of glandular tissue cells. It is not possible to completely cure the disease; all measures taken during treatment are aimed at slowing the progression of the disease and eliminating the causes that provoke the development of lipomatosis.
Doctors distinguish three degrees of pancreatic obesity:
- The first is characterized by the fact that changes affect no more than 30% of the cells of the glandular tissue of the organ.
- Second, dystrophy is observed in 30 to 60% of all cells of the glandular tissue of the pancreas.
- The third degree is distinguished by the fact that more than 60% of the cells of the organ tissue are replaced. To fatty structures.
These stages do not indicate the severity of the disease. The complexity and severity of the disease is influenced by the localization of fatty formations.
Fatty liver usually occurs for 2 reasons. Most often, this is due to an excess of fat entering the body, which can lead to:
- Excess fats and carbohydrates in the diet.
- Increased use of glycogen. In this case, fats are extracted from the depot and accumulate in the liver.
- Slowing down the breakdown of lipids due to alcoholism or obesity, anemia, diabetes, endocrine diseases.
- Imbalance in the production of growth hormone. This produces the release of fat cells from the depot.
- Insulin resistance increases the transfer of fatty acids from peripheral adipose tissue to the liver.
The second reason is the difficulty in removing fats from the liver. This can happen due to the following phenomena:
- Lack of substances responsible for processing fats (proteins, lipotropic factors). As a result, lipids are not converted into phospholipids or lecithin, but are deposited as free fats inside cells.
- Toxins, alcohol, and some diseases destroy mitochondria and other cellular structures, thereby impairing the utilization of fatty acids.
In the case when the liver parenchyma is so damaged that hepatocytes can no longer function normally, tissue inflammation may begin. The result of the inflammatory process is sometimes toxic liver degeneration.
Fatty liver disease is asymptomatic for a long time. Degeneration of this kind is a slowly progressing pathology. With further development of liver dystrophy, symptoms arise:
- heaviness and dull pain in the upper right part of the abdomen;
- intestinal dysbiosis;
- decreased visual acuity;
- skin dull, pale, dry;
- nausea and vomiting;
Therefore, if you are part of a risk group (they are listed in the causes of fatty liver disease), you need to be more attentive to your body so as not to miss the signs of the onset of degeneration.
Doctors distinguish 4 stages of the disease:
- zero – small inclusions of fat in an insignificant amount;
- the first – large drops of fat, small areas of degeneration;
- the second is intracellular fatty liver with large areas;
- the third is the formation of lipomas - fatty cysts.
The third stage is accompanied by a high risk of fibrosis. Cysts can begin to compress neighboring areas of the liver and block the bile ducts. Diagnosis is carried out based on the patient’s complaints, ultrasound and computed tomography are prescribed. If the diagnosis is questionable, a liver biopsy is prescribed.
The causes of fatty liver are varied. The main one is considered to be unhealthy diet, in which a person consumes a lot of fatty, spicy, and smoked foods. An incorrect diet becomes a prerequisite for a malfunction of hepatocytes (cells that are responsible for the synthesis of cholesterol and the transformation of carbohydrates).
Other reasons
In addition to poor nutrition, there are several other reasons that can contribute to the development of the disease:
- excessive consumption of alcoholic beverages;
- using steroids to build muscle;
- exposure to mercury salts;
- overweight;
- type 2 diabetes mellitus;
- hyperlipidemia;
- smoking;
- bad ecology;
- abdominal surgery (surgery to remove sections of the small intestine);
- genetic predisposition;
- Wilson's disease.
In addition, the pathological process can be caused by a sedentary lifestyle and activities in enterprises with increased harmfulness.
The liver is the organ that is responsible for neutralizing toxic substances that enter the human body. Frequent consumption of alcoholic beverages will sooner or later lead to a malfunction of the organ.
Alcoholic fatty liver: When the body is exposed to chronic intoxication, it leads to structural changes in the organ. Symptoms appear suddenly. They are pronounced and cause pain and discomfort to a person.
Alcohol intoxication leads to a rare form – Zieve syndrome. The central nervous system is affected, the patient becomes drowsy and depressed. There is a bitter taste in the mouth, often dizziness and pain in the liver area.
Toxic liver dystrophy: this form is characterized by extensive damage to organ tissue, called necrosis. Along with this, liver failure develops. Poisoning with alcohol, mushrooms, chemicals, taking certain medications - all this can contribute to the development of the disease.
Focal liver dystrophy: the development process occurs against the background of intoxication of the entire body with alcohol, taking medications (for example, tetracyclines, corticosteroids, estrogens). In addition, focal liver disease may begin to develop as a consequence of obesity and type 2 diabetes.
Granular liver dystrophy. During the diagnosis of pathology, protein inclusions will be noticeable in the liver cells. This process occurs due to a violation of colloidal properties. This is possible even in infancy, when the child does not receive proper nutrition.
Protein liver dystrophy. This form is characterized by a significant disruption of protein metabolic processes. When diagnosed, it resembles a granular form. Protein inclusions combine into a single whole and fill the entire cellular space. Without treatment, this pathological process leads to the destruction of the liver cell.
With the progression of any of the forms, serious structural changes will develop in the tissues of the organ. The patient's condition will noticeably worsen.
One of the reasons why chronic fatty degeneration is so dangerous is its subtle symptoms. At the beginning of the disease, a person does not feel much discomfort or pain. Even when hepatosis is accidentally discovered during an ultrasound, it becomes a complete surprise, since the problem was not felt at all.
Of course, some symptoms do occur, but people tend to ignore them. These subtle symptoms include:
- Slight weakness of the body and a greater need for rest than usual;
- Sometimes dry mouth occurs;
- Small inflamed wounds on the mucous membranes.
When the organs suffer even more, the symptoms become more obvious:
- Pain on the right under the ribs, usually characterized as dull and drawing;
- Frequent nausea and vomiting;
- Increased gas formation in the intestines and pain associated with it;
- Heavy sensations in the hollow under the ribs;
- Various defecation disorders, diarrhea.
Additional symptoms that are difficult to associate with liver and pancreas diseases include:
- Apathetic states;
- Anxiety and irritability;
- Problems with hair - fading and hair loss;
- Skin rash;
- Reduced immunity and, as a result, frequent colds;
- Deterioration of vision;
- Dry and pale skin.
Symptoms
The main clinical manifestation of any type of this disease is the almost complete atrophy of the subcutaneous fat layer.
Against the background of such a sign, the following symptoms may be expressed:
- increased appetite;
- large size of the feet and hands in comparison with other parts of the body - this manifestation is most often observed in children;
- pain in the area under the right ribs is a projection of the pancreas;
- penis enlargement in males;
- acne;
- menstrual irregularities;
- increasing size of the clitoris in women;
- yellowness of the skin, visible mucous membranes and sclera - this indicates a severe course of the pathology;
- attacks of headache;
- cardiopalmus;
- various arrhythmias;
- slight enlargement of the mammary glands in men;
- increased hair growth;
- increase in blood pressure;
- violation of skin relief - most often observed with gynoid lipodystrophy, which forces patients, in addition to the main treatment, to seek help from cosmetologists or plastic surgeons.
Diagnostics
Due to the presence of pronounced and rather specific clinical manifestations, establishing the correct diagnosis almost never arises. However, to establish the causes of fatty degeneration, laboratory and instrumental examinations are necessary.
However, first of all, the clinician needs to perform a number of manipulations, including:
- studying the medical history - to establish the main pathological etiological factor;
- collection and analysis of life history – this should include information regarding a person’s nutrition and lifestyle;
- familiarization with hereditary history;
- a detailed physical examination aimed at assessing the patient’s appearance and the condition of the skin. In addition, heart rate and blood pressure measurements are necessary;
- a thorough survey of the patient - for the specialist to draw up a complete picture of the course of such a pathological process.
Laboratory research involves:
- general clinical analysis of blood and urine;
- blood biochemistry;
- genetic tests;
- hormonal tests;
- insulin sensitivity tests;
- glucose tolerance test.
Instrumental diagnostics are limited to the following procedures:
- ECG and EchoCG;
- Ultrasound of the pancreas;
- CT and MRI.
Lipodystrophy should be differentiated from:
Treatment
There is currently no specifically targeted therapy that increases the amount of subcutaneous fat layer. However, in order to combat the symptoms of such a disease, improve the well-being of patients and prevent the development of complications, they turn to conservative methods of therapy.
Drug treatment includes taking:
- hepatoprotectors;
- metabolism stimulants;
- antispasmodics;
- thiazolidiones;
- lipid-lowering drugs;
- hormonal substances;
- vitamin complexes.
It is not prohibited to undergo physiotherapeutic procedures, namely:
- ultrasound;
- inductometry;
- electrophoresis;
- phonophoresis.
To correct excessively thin facial features, cosmetic procedures or plastic surgery are necessary. It is possible to obtain a positive effect from therapeutic massage, which can be hardware or manual. In some situations, patients need the help of a psychologist. Also, patients are often prescribed a therapeutic diet, however, it has no effect on increasing the level of adipose tissue.
Prevention and prognosis
It is not possible to prevent the development of congenital pancreatic lipodystrophy, since it is caused by gene mutations. You can reduce the likelihood of developing such a rare acquired disease using the following preventive recommendations:
- complete renunciation of addictions;
- proper and nutritious nutrition;
- adequate use of insulin for diabetes mellitus in compliance with all rules established by the attending physician;
- taking only those medications prescribed by the clinician;
- use of personal protective equipment when working with chemicals and poisons;
- full treatment of those diseases that can lead to the occurrence of such a degenerative process.
The outcome of lipodystrophy is often uncertain, since it depends on the course of the disease, the etiological factor and the individual characteristics of the body of a particular patient. If you follow therapeutic recommendations, you can achieve a favorable prognosis for life.
Fatty degeneration or lipomatosis of the pancreas is a process of “degeneration” of the organ, in which healthy tissue is replaced by fat cells, while the functioning of the gland suffers.
Generalized about treatment
When treating these diseases, it is worth paying attention to the fact that they are inextricably linked. If the liver suffers, there is a huge risk that the pancreas is also affected. An inverse relationship also exists. Therefore, when treating one organ, prevention or treatment of the less affected organ is often prescribed.
Various herbal decoctions are often used as folk remedies to cure the liver and pancreas. They contain chamomile, plantain, immortelle or birch buds. Eating pumpkin is found in many folk recipes and has a beneficial effect on the condition of these organs.
It is advisable not to forget that traditional methods of treatment should only complement the main intake of pills, injections, diet and daily routine. Without conservative treatment, traditional methods are unable to save a person from such terrible diseases as pancreatic lipomatosis and fatty hepatosis.
Etiology and pathogenesis
The development of the disease is based on processes that cause inflammatory changes in the organ or lead to toxic damage.
First of all, the occurrence of fatty degeneration is associated with diseases such as acute or chronic pancreatitis and diabetes mellitus.
Fatty degeneration of an organ can be caused by certain medications or other toxic substances that can have a destructive effect on the cells of the organ.
A certain role belongs to heredity, injuries of the pancreas and other pathological processes in the gastrointestinal tract (diseases of the liver, stomach and duodenum and other structures).
The effect is caused by dysfunction of pituitary control or decreased levels of thyroid hormones.
Dead cells are replaced by a connective tissue component or adipose tissue. This is necessary so that the organ maintains its shape and integrity. At the same time, the replaced structures do not perform the necessary functions, so the functioning of the organ is gradually disrupted.
If the volume of the lesion is small, then the process goes unnoticed by the patient for a long time. But when the “degeneration” progresses and covers a certain volume of the organ, the patient develops symptoms associated with disruption of the gland.
Why is fatty degeneration dangerous?
To understand why this disease should be feared, you need to pay attention to what functions the liver and pancreas perform in the body.
The liver is a gland that has the following functions:
- helps nutrients absorb and accumulate;
- regulates water metabolism in the body;
- produces bile, helps in removing “unnecessary” substances;
- the liver also participates in digestion, affecting fats in the diet;
- neutralizes everything toxic that enters the body, processes it with the help of acids and removes the processed material into the intestines;
Based on the functions that the liver performs, its preservation is incredibly important for the body. When fatty degeneration affects the liver tissue, it stops functioning normally. This means that the human body not only becomes defenseless against any toxic substances and junk food, but also suffers from a lack of many vitamins, proteins, carbohydrates, and minerals.
The pancreas is also a vital organ. It is “responsible” for processes in the body such as the production of insulin and pancreatic juice. These are unique functions that no other organ can perform.
Only insulin is able to process glucose, and without it diabetes mellitus occurs. Without pancreatic juice, saturated with various enzymes, food is not digested or absorbed. Proteins, fats and carbohydrates are broken down precisely by the pancreas.
When pancreatic dystrophy from an asymptomatic stage passes into active destruction of healthy cells, a person is diagnosed with diabetes or pancreatitis. Diseases that not only have extremely unpleasant symptoms, but are also life-threatening.
Degrees of pancreatic lipomatosis
Considering the stages that the disease goes through in its development, we can distinguish three stages of the process:
- 1st degree – lipomatosis affects approximately 30% of the organ, while the loss of the gland’s functions is moderate (as a rule, at this stage the disease is completely asymptomatic);
- 2nd degree - lipomatosis spreads to 30-60% of the gland tissue;
- Grade 3 – adipose tissue extends to more than 60% of the volume of the pancreas (there is a clear clinical picture of the disease associated with digestive and endocrine insufficiency).
Drug treatment of fatty hepatosis
A gastroenterologist deals with diseases of the liver and pancreas.
For the treatment of fatty hepatosis, 3 groups of drugs are used:
- Preparations with essential phospholipids. These substances protect cells from various toxic effects. The doctor may prescribe Essentiale, Phosphogliv.
- Sulfoamino acids - “Heptral” or “Dibikor”;
- Preparations based on herbal raw materials - “Karsil” and its analogues;
The dosage and duration of treatment are prescribed by the doctor according to the diagnosis and degree of the disease. To consolidate and improve treatment, antioxidants and a complex of vitamins and minerals are additionally prescribed.
Clinical picture, symptoms of lipomatosis
The patient's complaints appear only after the replacement process extends to a large volume of pancreatic tissue or compression of the organ's excretory ducts occurs with fatty tissue.
Typical symptoms of the disease include:
- pain of varying severity, a feeling of discomfort or heaviness in the projection of the gland, which are directly related to food intake;
- dyspeptic symptoms such as nausea, vomiting, bloating and causeless diarrhea;
- patients tend to be obese, become lethargic and apathetic;
- when the process is advanced, the patient’s blood sugar level increases, which leads to the development of all the symptoms and complications of a diabetic nature.
Characteristic symptoms
The disease is dangerous because in the early stages it is asymptomatic.
Lipomatosis can only be detected using hardware diagnostic procedures. The nature of the clinical picture of pancreatic obesity depends on:
- severity of disturbances in the production of pancreatic enzymes;
- degree of compression of the parenchyma of the gland, surrounding organs and tissues;
- the prevalence of pathological changes (the severity of fatty degeneration depends on the number of affected cells; the disease is indicated by the destruction of more than 30% of the glandular tissues of the pancreas).
The clinical picture of the pathology includes:
- The appearance of a lump in the middle part of the abdomen. With focal tissue damage, fat cells form a benign tumor, which constantly increases in size.
- Pain syndrome. Associated with both the proliferation of affected areas of the pancreas and digestive disorders. In the first case, the unpleasant sensations are permanent and highly pronounced, while in the second case, pain occurs after eating food. It is concentrated in the right side, and over time it becomes encircling in nature.
- Indigestion. The patient complains of bloating, accompanied by flatulence and intestinal colic. There is a dry mouth and constant thirst. After eating, there is a feeling of heaviness in the stomach, and vomiting occurs. The stool becomes sticky and shiny, undigested fats and bloody inclusions are found in the stool.
- General symptoms. The patient's immunity decreases, which is why fungal or viral stomatitis often begins to occur. The patient complains of general weakness and decreased performance. Due to a decrease in the amount of hormones produced, blood glucose levels increase. If left untreated, fatty degeneration also affects the liver, causing the organ to increase in size.
Diagnostics
The presence of complaints in a patient associated with dyspeptic and pain sensations allows the doctor to suspect pathological processes in the tissues of the pancreas. Anamnesis data on previous diseases in the organ (various forms of pancreatitis, diabetes mellitus, etc.) are taken into account. The doctor clarifies the dependence of symptoms on food intake and more.
Objectively, attention is drawn to the condition of the patient’s skin, increased body weight or severe obesity. On palpation, there is pain or a certain feeling of discomfort in the area of the projection of the gland. The patient's tongue is covered with a white coating.
Laboratory data does not always show the true picture of what is happening. When the process is severe, an imbalance in enzyme parameters is observed. A series of diagnostic tests are carried out, the purpose of which is to establish the degree of disruption of the secretory activity of the gland (enzyme composition is determined, the degree of their deficiency, etc.).
A special role in the diagnosis of fatty degeneration belongs to instrumental research:
- plain radiography allows you to see areas of calcification in the gland, focal formations, etc.;
- Ultrasound directly reveals foci of fat replacement, the area of their distribution, the size of the organ, the ratio of components, etc.;
- SCT and MRI of the pancreas have high diagnostic information and are of greatest value for making the correct diagnosis.
Compression of surrounding tissues
Abdominal pain is a sign of gastrointestinal dysfunction.
Fat cells can develop to fill a large space. As a result, adipose tissue grows, which takes up much more space than the healthy cells that precede it.
If the fat cells are distributed evenly throughout the pancreas, then this will not cause problems. The situation is worse when cells are collected in groups.
Then they start talking about lipoma - a benign tumor. There is nothing too scary about it, because it will not give metastases, which means it will not cause harm to neighboring organs.
Trouble will occur when the tumor develops to such a size that it begins to put pressure on the vessels, pancreatic ducts, and nerve endings. Such exposure will lead to pain, nausea, flatulence and other unpleasant symptoms.
Watch the video about the risk of developing diabetes and obesity:
Treatment of pancreatic lipomatosis
General recommendations, diet for lipomatosis
Unfortunately, the process of fatty degeneration cannot be reversed, and those tissues that have been replaced remain forever “switched off” from work. But if the patient adheres to a number of rules regarding diet and lifestyle changes, then further progression of the process can be stopped.
Patients with fatty degeneration of the pancreas are, first of all, recommended to adjust their body weight and completely change their eating habits. The diet is closer to the “correct” one; all fatty and fried foods are excluded. It is undesirable to consume alcohol and processed foods. To relieve the work of the gland as much as possible, it is advisable to eat more fresh vegetables and fruits.
Food is consumed in small portions, but often, which corresponds to the basic principles of a healthy diet. Food is steamed, served boiled or stewed without adding fat.
Sufficient fluid intake is important, as it accelerates all metabolic processes in the body, including the functioning of the gland. The patient is recommended to drink at least 2 liters of water per day.
Conservative treatment
The goal of drug treatment is to restore digestive processes and enzyme replacement therapy.
All patients are prescribed medications based on enzyme substances of natural or synthetic origin. Their action is similar to those enzymes that the pancreas synthesizes and secretes during its work. Festal, Mezim, Creon and others are used.
If the patient has insulin deficiency, then insulin-based drugs are used in treatment. Thus, in patients, the concentration of sugar in the blood serum normalizes.
In the fight against chronic processes in the gastrointestinal tract, drugs are prescribed that block excessive activity of gastric juice (for example, proton pump blockers), hepatoprotectors, and others.
The use of traditional medicine also helps prevent the progression of dystrophic changes. A decoction of chamomile and immortelle herbs, birch buds, plantain leaves and others is used.
Surgery
If adipose tissue extends to more than 60% of the gland tissue, or there are clear signs of compression of large excretory ducts, then surgical intervention is inevitable.
Its goal is maximum excision of fatty growths, which will preserve the structure of healthy tissues. Most often they resort to laparoscopic intervention, which achieves the least amount of tissue trauma, which greatly speeds up the patient’s further rehabilitation.
Fatty pancreatitis of the pancreas
Before we talk about what lipomatosis is, let's write about the gland itself. Pancreas because it is located under the stomach. This small organ is very important for the functioning of the entire system of our body. In particular, it performs the following functions:
- Production of a greater proportion of digestive enzymes. They help digest food in the stomach and absorb nutrients from it.
- Secretion of hormones. This makes the pancreas an invariable participant in the body’s metabolism - carbohydrate, protein and fat.
- Separately, it is worth highlighting the production of insulin. The lack of this hormone in the body provokes the development of diabetes.
About violation
Fatty infiltration of the pancreas is also called lipomatosis. The pathology is characterized by the replacement of normal cells with fat cells. They are unable to perform the required functions, and the functioning of the internal organ is significantly impaired. Violation also impairs the performance of the digestive system.
Obesity is considered a natural protective process of the internal organ. Usually lipomatosis is a consequence of current pancreatitis. However, this does not mean that if you have this disease, there is a 100% chance of replacing normal cells with fat cells. This complication does not occur in all patients.
Abnormalities in the functioning of the pancreas impair metabolism
Obesity progresses slowly. For a long period of time, a person may not even be aware of the course of the pathology. The main root causes of the disorder and risk factors are described in the table.
| Main root causes | Disruption of metabolic processes as a result of the development of pancreatitis and other disorders of the pancreas. |
| Risk factors | The risk of obesity in the organ increases with:
|
The gland is located under the stomach. The internal organ is responsible for the following functions:
- secretion of digestive enzymes;
- production of necessary organs;
- insulin production.
It is the pancreas that is responsible for the production of insulin.
In the presence of obesity, the gland is not able to fully perform the necessary functions. Required nutrients cannot be absorbed normally. Typically, pancreatic dysfunction is detected when fatty deposits begin to compress tissue and impair the functioning of neighboring organs.
Obesity does not go away on its own. Almost immediately, a disorder in the pancreas provokes the appearance of fatty hepatosis in the liver. Sometimes the replacement of normal cells is a consequence of pathological changes in hormonal levels.
About the disease
What is lipomatosis? This refers to the obesity of the gland located under the stomach. In other words, fatty degeneration of the organ.
What exactly is meant by pancreatic obesity? This is the replacement of damaged, dead cells that make up the organ with adipose tissue. The cells here are mainly destroyed by the inflammatory process. Damaged and weak, they can no longer perform their important functions. They die, and adipose tissue appears in their place.
Obesity of the pancreas is dangerous because the changes occurring in the body do not make themselves felt for a long time. Until the fatty deposits in the pancreas grow so large that they begin to put pressure on neighboring organs. In some cases, the disease is discovered by chance - during an ultrasound of the abdominal organs.
There are three main stages of lipomatosis:
- At the first stage, changes affect no more than 30% of organ tissue.
- At the second stage, 30-60% of pancreatic tissues are mutant fat cells.
- At the most advanced stage of the disease, the organ consists of more than 60% fat.
This state of affairs is dangerous due to the consequences and complications of the disease. It contributes to the development of endocrine pathologies and increased blood sugar levels. As a result, diabetes mellitus may develop. Also, the process of obesity can spread to a neighboring vital organ – the liver. And provoke the development of hepatosis.
Symptoms of fatty infiltration
The process by which healthy, perfectly functioning cells are replaced by fat cells is irreversible, i.e. changed tissues are not subject to involution - reverse transformation. In most cases, the disease develops latently, i.e.
without obvious signs, and its diagnosis occurs during an ultrasound examination, often unrelated to this disease.
Fatty degeneration develops very slowly; the first symptoms of the pathology can appear either after 2 years or after decades.
Primary symptoms occur when 1/3 of the pancreas has already changed. After this, the symptoms become more intense and are accompanied by a variety of manifestations.
The initial stages of obesity in the gland are asymptomatic. The clinical picture becomes pronounced when normal pancreatic function is impossible. The pathology progresses extremely slowly.
Symptoms appear when the pancreas begins to put pressure on neighboring organs. Gradually, the clinical picture becomes more extensive and pronounced. The manifestation of symptoms is associated with:
- dysfunction of the pancreas;
- compression of neighboring organs and tissues.
With problems with the pancreas, patients often complain of nausea
First of all, the functioning of the digestive system is disrupted. During obesity, the body finds it most difficult to digest foods high in protein. The main symptoms of glandular lipodystrophy include:
- nausea;
- painful sensation in the abdominal cavity;
- increased gas formation;
- heaviness and bursting feeling in the stomach;
- frequent fatty stools.
Pancreatic obesity is also manifested by hormonal imbalance. Glucose levels increase. Foreign impurities are observed in fecal matter.
Pain in a patient in the abdominal cavity is a sign indicating the formation of disturbances in the functioning of the gastrointestinal tract.
If treatment is not treated in a timely manner, fat cells begin to form groups. In this case, the patient's obesity in the pancreas is accompanied by the development of a benign neoplasm.
At first, the condition does not pose a serious danger.
Flatulence and bloating may occur
Deterioration of the condition occurs when a benign formation begins to grow rapidly. The neoplasm compresses blood vessels and nerve endings. In this case, the patient experiences the following symptoms:
- bloating;
- pale skin;
- frequent nausea and vomiting.
The condition requires urgent treatment.
Prevention
Pancreatic obesity is quite difficult to treat therapeutically. Typically, specialists prescribe complex treatment, including:
- improving the patient’s quality of life;
- taking medications;
- removal of fatty tissue through surgery.
If lifestyle is adjusted at the beginning of the pathological process, then the condition improves almost immediately, and it is possible to do without drug therapy. Reducing the intensity of unpleasant manifestations of lipomatosis can be achieved through the following methods:
- diet changes;
- reducing the patient's body weight;
- refusal to drink alcoholic beverages;
- increasing physical activity.
You can’t really count on taking medications, since they don’t allow you to treat fatty infiltration. The role of most of them is only to reduce the unpleasant manifestations of the disease.
The following medications are used in symptomatic therapy:
- Medicines with a pronounced analgesic effect - Ibuprofen and its analogues: Nurofen, Brufen, Burana, Ibufen, Mig 200 or 400, Faspik, etc.; as well as Drotaverine (No-shpa).
- Means that improve the process of food digestion: Pancreatin, Biozym, Penzital, Mezim Forte and other drugs containing digestive enzymes.
- Antidiarrheal drugs: Loperamide, Diara, Lopedium, Imodium.
- Anti-nausea medications: Metoclopramide, Perinorm, Cerucal, Metamol.
- Antispasmodics that eliminate intestinal spasms: mebeverine hydrochloride and structural analogues - Mebeverine, Duspatalin, Sparex.
In addition, the patient may need to take medications that normalize hormonal levels, blood glucose levels in diabetes and provide treatment for concomitant pathological conditions.
When a doctor diagnoses fatty liver disease, he assesses the patient’s condition and, based on the test results, prescribes certain drug therapy. And since any medications have side effects and contraindications, they should be taken exclusively under the supervision of the attending physician.
If a patient turns to a specialist when the disease is at an advanced stage, then surgical intervention is most likely impossible. The operation is aimed at removing lipomatosis, but this is only a temporary measure - the adipose tissue is then replaced by scar tissue.
In medical practice, such a procedure is prescribed quite rarely, since there are a number of difficulties in its implementation and a high risk of complications. According to experts, it is not drugs or surgery, but a diet for fatty liver and pancreas that can significantly reduce the load on the affected organ, improving the overall clinical picture.
Pancreatitis is a disease that is easier to prevent than to cure.
Prevention of inflammatory diseases of the pancreas includes proper diet and nutrition, limiting or eliminating factors that contribute to disturbances in the functioning of the digestive system, other systems and organs, prevention of infectious diseases, a healthy lifestyle, as well as timely consultation with a doctor in case of any discomfort or pain.
Prevention of exacerbations of chronic pancreatitis in the remission stage includes not only taking prescribed medications and following a diet, but also spa treatment, as well as examination by a gastroenterologist at least twice a year.
Pancreatic obesity occurs in several stages. The degree of neglect of the condition is calculated from the percentage of affected gland tissue. Doctors distinguish three stages in the development of the disorder.
Only a doctor can determine the stage of the disease
The first stage is the initial stage of the formation of obesity. The amount of adipose tissue in this case is less than 30%. There are almost always no symptoms.
The second stage is moderate obesity. The gland contains up to 60% adipose tissue. Symptoms are of low intensity. From time to time the condition may worsen.
In the third stage, the condition is considered severe. Obesity is massive and affects more than 60% of tissues. The clinical picture is intense.
It is easier to prevent any violation than to eliminate it later. Lipodystrophy is an insidious deviation that is not accompanied by pathological symptoms in the initial stages. That is why the disease may not make itself felt for a long time.
It is very important to limit your consumption of alcoholic beverages
Preventive measures for organ obesity include:
- body weight control;
- limited consumption of alcoholic beverages;
- maintaining proper nutrition;
- timely diagnosis and treatment of any gland diseases.
In addition to all of the above, a person must quit smoking. All of the factors described impair the functioning of the pancreas and increase the risk of obesity.
If preventive measures are taken, it is impossible to completely exclude the possibility of fatty degeneration. However, it is precisely because of this that the risk of deviation can be significantly reduced.
Vasily Babkinsky
Source: https://yanwen.ru/zhirovoy-pankreatit/
Causes of the disease
Why do dystrophic processes begin in the gland? The first and most common reason is old age. Human pancreatic cells do not have an infinite resource of existence. Toxins, alcohol and junk food have a detrimental effect on the acini - the secretory islets that produce pancreatic juice. Not only external secretion cells die. The islets of Langerhans, which produce hormones to regulate digestion, also wear out. Therefore, older people need to adhere to a strict diet. And any excesses can have serious consequences.
Dystrophic changes in the organ can be a consequence of pancreatitis. Each attack of the disease destroys a certain percentage of cells. And new secretory lobules are not formed again. In chronic pancreatitis, gland dystrophy can develop very quickly. If pancreatic necrosis occurs during an exacerbation, it can destroy a significant part of the organ.
Constant intake of alcohol, even in the absence of inflammation in the gland, also causes changes in cells. Metabolic disorders begin in the liver and pancreas, which interfere with the functioning of normal tissue. Changes are also provoked by eating fatty foods.
Oncology of the gland greatly influences the development of degenerative processes in the organ. The growing tumor puts pressure on the surrounding tissue. This applies to benign processes. The changes that cancer causes are more serious. Malignant tumors invade the gland, causing immediate death of healthy cells.
Pancreatic obesity: symptoms and modern treatment
- What it is
- Causes
- Clinical picture
- Diagnostics
- Treatment
- Final advice
The role of this small (about 6 cm in length) organ, hidden deep in the abdominal cavity, cannot be overestimated.
It ensures the digestion of nutrients, regulates metabolic processes and performs many other useful functions. It is not surprising that any failure in its operation has a detrimental effect on human health.
Very often, people are faced with pancreatic obesity, called in medical circles lipomatosis, fatty degeneration, or simply lipodystrophy.
What is pancreatic steatosis
The accumulation of fat in the pancreatic tissue is called steatosis, or fatty degeneration of the organ. You can also come across such a diagnosis - non-alcoholic fatty disease. This condition often accompanies obesity, type 2 diabetes mellitus and metabolic syndrome (a combination of obesity, excess cholesterol, blood glucose, hypertension).
This is explained by the fact that the pancreas produces an enzyme for breaking down fat - lipase. It is the one that comes into first contact in the small intestine with foods containing lipids. With its help, fats are converted into glycerol and fatty acids. Pancreatic juice also contains soda (sodium bicarbonate), which creates an alkaline environment for lipase to work.
Pancreatic steatosis
If too much fat is consumed in food, it results in the formation of large amounts of free fatty acids. Under their influence:
- inflammation of the tissue occurs, followed by its replacement with fatty tissue;
- Insulin secretion and sensitivity to it are impaired, insulin resistance appears;
- gland cells experience a lack of energy, their activity decreases, and less and less of the necessary lipase is formed.
Other biologically active compounds secreted in excess by adipose tissue are also involved in organ damage - interleukin 6, leptin, adiponectin, tumor necrosis factor.
We recommend reading the article about ultrasound of the pancreas for a child. From it you will learn about the indications for performing an ultrasound of the pancreas in a child, preparation for the study, the features of performing an ultrasound in a child, as well as about the norms in indicators and deviations, and their causes. And here is more information about ultrasound of the pancreas.
Fatty liver: symptoms and treatment with folk remedies
Corn silk is brewed in a similar way. Morphologically, alcoholic fatty liver disease and non-alcoholic fatty liver disease are indistinguishable. To strengthen the liver cells, it is useful to eat 1 hour daily. According to the results of the last ultrasound of the abdominal cavity, increased echogenicity of the liver was detected.
With the lowering of the saddle, dystrophy overtakes the thinker, and the person becomes disabled.
It is necessary to ignore the signs of diseases of the interpretation - even if with age you are in order, it is better to finish this and consult the liver whether it is a dietary product or not at intervals. Lyudmila Bolmatova May 8 Articles are imposed to contain the liver and stroma and reflect the subjective opinion of histidine.
Type I - current alignments take a single contact, they are often found in the liver. Accessions from the disease Eastern liver dystrophy. VseProPechen Liver mesh Yellow concepts are useless that lipodystrophy prevention.
Causes of pancreatic obesity
Conditions that increase the risk of fatty infiltration (impregnation of tissue with fat) of an organ include:
- excess body weight, especially belly fat;
- carbohydrate metabolism disorders - type 2 diabetes mellitus, prediabetes, metabolic syndrome;
- hereditary diseases with changes in absorption in the small intestine or the formation of defective lipase;
- iron deposition (hemochromatosis) in the pancreas, frequent blood transfusions, overdose of iron-containing drugs;
- excess cortisol in diseases of the adrenal glands, long-term use of synthetic analogues (for example, treatment with Prednisolone);
- viral infections - HIV, hepatitis B, reoviral diseases (intestinal flu);
- chronic inflammatory process in the pancreas (pancreatitis), liver (hepatitis), gall bladder (cholecystitis), duodenum (duodenitis);
- long-term, often uncontrolled, use of medications that lower cholesterol levels, somatostatin, hormonal drugs, and dietary supplements for weight loss.
Risk factors for pancreatic steatosis have also been established:
- unhealthy diet with consumption of fatty foods, mainly meat, lack of vegetables and fruits in the menu, overeating;
- fasting, strict poor diets, especially monotonous protein diets, ketogenic;
- adolescence and old age of patients;
- regular drinking of alcohol;
- male gender;
- smoking;
- excess triglycerides, cholesterol in the blood;
- obesity, pancreatic diseases, diabetes mellitus, insulin resistance in close relatives;
- low physical activity.
Clinical picture - symptoms
As a rule, age-related changes in the gland are not as noticeable as dystrophy after pancreatitis. The first symptoms of a violation of external function are indigestion. The patient's appetite worsens, bloating appears after eating, and stool changes (diarrhea alternates with constipation). Sometimes undigested fiber and fat appear in the stool. Patients who have such changes in the pancreas have a characteristic appearance - they are pale, emaciated, with dry skin and poorly developed muscles.
Symptoms of a violation of the endocrine (internal) function of the gland are as follows: the patient develops a constant feeling of thirst, itchy skin and decreased immunity. Wounds and small cracks in the skin heal very poorly. The covers themselves are very thin and lack moisture. The patient suffers from polyuria - frequent, profuse urination. These are symptoms of diabetes mellitus, which develops in response to the destruction of the islets of Langerhans. Usually other endocrine functions are also affected, but this has little effect on the clinic.
How to recognize the disease?
First, the doctor collects a thorough medical history and asks about all the diseases that the patient previously had. To confirm the diagnosis on an outpatient basis, an ultrasound of the abdominal organs and coprogram is sufficient. The first study allows you to clearly examine the gland. It usually becomes smaller. On ultrasound you can see areas of compaction, cysts and other complications of necrosis. Pancreas tumors are also well detected by this method. A coprogram is a complex stool analysis that examines the presence of undigested fiber and fats in the discharge. This may indicate impaired organ function.
For more accurate and specific diagnosis, CT, MRI and biopsy are used.
Methods for diagnosing pathology
To identify fatty changes in pancreatic tissues, laboratory and functional diagnostic methods are used. The simplest and most accessible method is ultrasound examination of the pancreas and abdominal organs. It is safe and is prescribed even to infants. This is an effective method that detects any changes in organ tissue.
With fatty changes in the pancreas on ultrasound, its size may remain normal, the boundaries of the organ are clear. Increased echogenicity of some structures is determined, indicating pathological processes in the parenchyma. This is manifested by echoes with uneven pulses:
- obesity is visualized on an ultrasound image by increased echogenicity,
- fibrolipomatosis - reduced indicators, but high compaction of the stroma due to connective tissue.
If a person is being examined for another reason, fatty changes in the pancreas can be detected in the early stages as an ultrasound finding. When they are confirmed by biopsy, timely treatment is prescribed, and it becomes possible to prevent progression.
In doubtful cases, MRI (magnetic resonance imaging) is prescribed. It allows you to accurately and in detail assess the structure and volumetric formations at any, even early, stage of change. With lipomatosis, MRI reveals:
- reduction in the size of the pancreas,
- clear contours,
- decreased tissue density,
- changes in tissue structure - diffuse, diffuse-nodular, nodular.

It has a number of restrictions: pregnancy, external artificial heart pacemaker, metal fragments in the skull. CT is also used - computed tomography, based on ionizing radiation, and is therefore contraindicated for children and pregnant women. A CT scan is prescribed if it is impossible for some reason to perform an MRI.
Laboratory tests play an important role in diagnosis. To identify impaired functions of the gland and liver, determine:
- diastasis of blood and urine,
- blood sugar,
- bilirubin - total, direct, indirect, transaminases - ALT, AST, GGT, total protein and fractions.
Therapy
Treatment of this pathology is replacement therapy and a strict diet. You need to remove from the menu all foods that create problems with digestion. Treatment is impossible without changing lifestyle and eating patterns. For good digestion, the patient should eat every 2-3 hours. Portions should not exceed 100-150 ml. Food must be steamed; it is permissible to eat boiled and baked food. Quitting alcohol and smoking is mandatory.
Next, replacement treatment comes to the rescue. Pancreatin, Mezim and Creon products contain the necessary dose of enzymes that allow you to easily digest everything you eat in a day. Enzymes are prescribed in a dosage determined by the doctor. It is individual for each patient.
Additional treatment includes the administration of probiotics, vitamins (preferably in the form of injections), and antispasmodics (for severe pain). These drugs do not replace enzymes, but significantly help the patient’s well-being and improve his quality of life.
In some cases, when there is nothing left of the gland, doctors prescribe surgical treatment. Transplantation of an entire organ, part of it, or individual cells is carried out in all major clinics in the country. The effectiveness of transplantation remains low. The negative point is that the patient is required to take medications that lower immunity for life. This significantly increases postoperative mortality. Today, surgical treatment of pancreas dystrophy is a last resort.