Good afternoon, many will be interested in understanding their health and that of their loved ones, and I will tell you my experience, and we will talk about increased bilirubin in a newborn. Most likely, some details may differ, as was the case with you. Please note that you should always consult with highly specialized specialists and not self-medicate. Naturally, you can quickly find the answer to the simplest questions and diagnose yourself. Write your questions/suggestions in the comments, and together we will improve and supplement the quality of the material provided.
Symptoms
We are talking about physiological jaundice if the high level of this pigment does not affect the well-being of the baby, but at the same time its integument is yellow-orange. Also, in this condition, the liver and spleen are not enlarged, and the color of urine and feces is not changed.
But jaundice does not always occur due to the development of a natural physiological process. In some cases, this indicates problems. The appearance of yellow skin already on the first day indicates possible bilirubin encephalopathy.
In this case, the liver and spleen are enlarged, the child will have a very weak sucking reflex and poor appetite. In addition, there is increased drowsiness, hypotension, and convulsions may begin.
Why does physiological jaundice appear?

During the breakdown process, a yellow-brown bile pigment is formed - bilirubin. It is produced in an indirect (unconjugated) form. It is toxic to the body. Increased bilirubin in a newborn has a negative effect on the digestive system, including the intestines, as well as on the heart and central nervous system.
The indirect form must bind in the liver. There, conjugated bilirubin is formed from it. This is already a non-toxic water-soluble form. It enters the bile and is excreted into the intestines. It is this pigment that gives stool its dark color.
But the liver of newborn babies continues to mature, so it often cannot cope with the increased load. This is why bilirubin accumulates.
Many newborns are diagnosed with so-called physiological jaundice. It is not dangerous if the amount of bilirubin does not go off scale. But in cases where doctors recommend treatment, you should not refuse it.
Provoking factors
These include various complications during pregnancy and diseases of the expectant mother. With a certain degree of probability, it can be assumed that the child may begin to develop jaundice after birth if the pregnant woman is diagnosed with diabetes. The pathology is also provoked by intrauterine fetal hypoxia or problematic childbirth. Neonatologists are especially attentive to those babies who had asphyxia during birth.
Also, taking a number of drugs during pregnancy can lead to bilirubinemia.
In this case, the liver and spleen are enlarged, the child will have a very weak sucking reflex and poor appetite. In addition, there is increased drowsiness, hypotension, and convulsions may begin.
One of the important indicators of a child’s health immediately after birth is the level of bilirubin in the blood, which is not stable in the first days of life and causes anxiety in young mothers, turning the baby’s body a jaundiced color. What should be the level of bilirubin in newborns, how to distinguish normal from pathology, and also choose the right treatment tactics? Only a pediatrician can answer these questions in detail after closely monitoring the baby’s condition, but in our article you will read basic information on this topic.

Increased bilirubin in a newborn due to jaundice
It can be of different types:
1. Physiological.
2. Pathological.
Physiological jaundice occurs quite often, can appear on the 4th day and disappears over time, without harming the baby. How elevated the level of bilirubin in a newborn is depends on how mature the fetus is, how the mother’s pregnancy proceeded, and whether she suffered from any diseases or other problems during pregnancy. Often jaundice can occur due to intrauterine hypoxia of the fetus, asphyxia and diabetes mellitus in the mother.
Treatment of elevated bilirubin in the maternity hospital and with home remedies

Doctors in the maternity hospital are required to monitor bilirubin levels in the blood of newborns. To get a complete systemic picture of pigment concentration, they prescribe biochemical blood tests throughout the baby’s stay in the hospital (2-3 times) and monitor the tendency for bilirubin levels to increase or decrease.
Mothers can keep this topic under control and ask the doctor whether such a test was taken from the child and what the results of the laboratory test are.
It is this approach that makes it possible to timely identify jaundice and prescribe measures appropriate to the child’s condition to treat this disease.
Important! If the baby has mild symptoms of jaundice, is active and breastfeeds well, no treatment is required! With continued breastfeeding, after a week the skin, mucous membranes and sclera are completely normalized.
Experienced specialists, as a rule, accurately determine the severity of the disease and all kinds of risks, in contrast to the advice of friends and general information on the Internet
In this case, young mothers should be patient, and if the child needs to remain under the supervision of a doctor for some more time, do not refuse this, do not take responsibility, and do not put the life and health of your child at risk.
After all the necessary studies - visual and laboratory - the specialist makes an appointment and gives recommendations.
Treatment of elevated bilirubin
Previously, the following methods were used to treat this condition:
- Intravenous administration of glucose solution (5%) - this agent allows the binding of bilirubin in the liver.
- Taking adsorbents that bind this substance in the intestines.
- The use of ascorbic acid and phenobarbital - these substances help increase the activity of liver enzymes.
- The use of choleretic drugs that promote the excretion of bilirubin with bile.
Currently, scientists have been able to prove that all these complex and sometimes painful treatment methods can be replaced with a simpler and more effective method - the use of phototherapy.
During this procedure, the baby's skin is irradiated using a special lamp. Under the influence of light, bilirubin is transformed into lumirubin. This substance is a photoisomer that is highly soluble in water and has no toxic effect. Subsequently, lumirubin leaves the child’s body naturally - it is excreted through urine and bile.
This method of therapy is completely painless for the child and allows you to cure jaundice in a fairly short time - as a rule, it literally takes 3-5 days. However, it must be taken into account that only new LED lamps are highly efficient, since the old equipment has exhausted its service life and cannot generate the required wavelength.
An excellent method for preventing and eliminating physiological jaundice is to put the baby to the breast early, since colostrum helps remove meconium and bilirubin from the baby’s body. Frequent feedings are also important.
It is very important to carry out treatment taking into account the cause of the development of the pathology and monitor the dynamics of this process. This therapy is carried out by neonatologists and requires a stay in a children's hospital.
An increase in bilirubin in the blood of newborns is considered a fairly serious condition that requires careful attention from doctors. In some cases, it indicates the development of physiological jaundice, which goes away on its own in a short time. However, sometimes an increase in this substance signals a pathological condition that can only be eliminated with the help of individually selected therapy.
Causes and consequences of high bilirubin in newborns

More than half of full-term babies and ¾ of premature babies suffer from jaundice in the first days. The risk group also includes:
- twins;
- children whose mothers have diabetes.
In order to recognize the pathology in a timely manner, blood from the umbilical cord is immediately taken from the newborn for analysis at the time of birth and again on the third day of life. This allows doctors to keep the situation under control and, if necessary, take emergency measures to preserve the health and life of the baby.
If after 2-3 weeks signs of jaundice continue to actively appear, doctors may suspect pathological jaundice, as a result of an increased concentration of bilirubin in the blood. The reasons for this condition may be:
- Hemolytic disease of newborns. This serious disease occurs against the background of rhesus - conflict between mother and child. It manifests itself as congenital internal edema of the subcutaneous tissue, an enlarged spleen and liver, and damage to the central nervous system.
- Genetic failure. In this case, the newborn may experience one of the following conditions: a defect in the formation of liver enzymes (Gilbert syndrome), decreased enzyme activity (Crigler-Najjar syndrome) and a deficiency of essential enzymes (Lucey-Driscol syndrome). With timely treatment, full compensation is possible, provided there is no severe damage to the brain nuclei.
- Damage to the liver by dangerous infections while the child is in the womb. Toxic agents and viruses reduce the ability to bind bilirubin and provoke parenchymal jaundice. This condition is characterized by prolonged jaundice, enlarged lymph nodes, darkening of urine and lightening of stool, and changes in biochemical blood tests.
- Blockage (obstruction) of the bile ducts, which occurs due to intrauterine cholelithiasis, the presence of a tumor in the body that compresses the bile ducts, bile thickening syndrome. This type of jaundice is called obstructive. The problem is solved by surgical intervention.

By observing the baby and knowing the signs of jaundice, mothers will be able to recognize the pathological or safe course of the disease and seek help from a doctor in time. Only in this case will it be possible to avoid such severe complications as:
- acute intoxication of the body;
- albuminemia, when albumin levels decrease and do not allow plasma to fully transport vitamins and nutrients;
- deafness, mental retardation, convulsions due to the penetration of bilirubin into the brain;
- involuntary motor reflexes that cannot be controlled;
- limb spasms.
We recommend reading: Radiculitis lumbosacral: symptoms and treatment with medication, folk remedies
Very rarely, but still there are cases when the most undesirable and very dangerous complication occurs - kernicterus, which symptomatically passes from one phase to another:
- Braking. The baby becomes lethargic, practically unable to suckle, all his reflexes are depressed.
- Irritation. The child is in hypertonicity, bends his back, twists, and screams heart-rendingly.
- Imaginary recovery. A safe stage at first glance, when it seems to everyone that everything is over and the child has completely passed the illness. However, this is only a temporary lull, during which you need to show special attention to the child and try not to miss a single symptom.
- Complication. Bilirubin attacks the brain, affecting the nuclei, affecting the nervous system, causing serious disorders in the body, which can result in cerebral palsy.
To diagnose complicated jaundice, biochemical, radiological methods, as well as biopsy are used.
Important! Timely diagnosis and correctly chosen medical tactics determine how severe the health consequences of jaundice will be.
Reasons for increased bilirubin
To answer the question of what high bilirubin means in a newborn, it is important to know that the reasons for its overestimation are completely different. And not always dangerous.
Natural
- Increased formation of the substance.
- Immaturity of the excretory organs.
- Reduced excretion.
- Incorrectly organized breastfeeding ( observed in 3% of newborns and does not require intervention other than establishing feeding ).
Every second baby is characterized by such conditions, which is not a cause for concern. Natural jaundice can be quickly treated without the intervention of drug therapy.
8 cases when pathological jaundice may develop
Bilirubin is a breakdown product of red blood cells
- Inconsistency between the Rh factor and the blood type of mother and baby.
- Infections acquired during pregnancy and childbirth.
- Hereditary diseases (hypothyroidism and other rare diseases).
- The previous child had a history of jaundice.
- Low weight and extreme prematurity.
- Insufficient feeding and/or vomiting.
- Neonatal resuscitation after birth.
- Diseases of the biliary and digestive organs, liver.
In these cases, pathological jaundice often develops at the level of increased bilirubin in the blood of the newborn.
What is the normal level of bilirubin in a newborn?
Bilirubin in the blood is presented in two fractions:
- Indirect (free), which is formed as a result of the fact that the rate of breakdown of red blood cells is higher than the ability of the liver to bind bilirubin. Free bilirubin is a substance that tends to dissolve only in lipids (fats). Due to its inability to dissolve in water, the pigment is very toxic, accumulates in the bloodstream, causing characteristic staining, and can disrupt the normal functioning of cells, easily penetrating into them.
- Direct (bound) bilirubin is formed directly in the liver. After biochemical interaction with the organic acid of the uronic acid group and liver enzymes, which reduce the toxicity of the pigment, it becomes soluble in water and is easily excreted from the body along with bile and urine.
The indicators of the two fractions add up to the total concentration of bilirubin in the blood, with direct bilirubin accounting for no more than 25% of the total volume.
In order for free bilirubin to become bound and soluble, it must be transported to the liver by certain proteins that newborns lack. As a result, the level of bilirubin in the blood increases, and physiological jaundice occurs.
The table shows the norms of bilirubin levels in infants (table of bilirubin in newborns by day)

Jaundice develops in newborns if bilirubin levels are above 50 µmol/l and is expressed, in addition to the concentration of pigment in the blood, by changes in the condition of the infant’s skin: initial color, capillary tone, the extent of the pigment distribution area.
To assess the intensity of changes in indicators, the Cramer scale is used, which can be used to assess the severity of the child’s condition:
- The head area turns yellow (eye sclera, face, palate, tongue below) - 100 µmol/l.
- Yellowness descends to the upper area of the body above the navel - 150 µmol/l.
- The area below the navel is added, including the buttocks and thighs - 200 µmol/l.
- The upper and lower extremities are painted with pigment - 250 µmol/l.
- Skin changes color throughout the body, including fingers, toes, palms and feet - over 250 µmol/l.

The higher the indicator, the more serious the reason to assume that the child has jaundice of various types and degrees of severity and such complications as gallbladder dyskinesia.
For full-term infants, the critical indicator will be the concentration of bilirubin in the bloodstream above normal and up to a limit of 250 µmol/l, for those born prematurely - 200. Infants born prematurely have a greater risk of being in the group diagnosed with “jaundice” due to underdevelopment of body systems and increased sensitivity to adverse conditions.
Indirect bilirubin toxins can cause damage to the deep structures of the anterior part of the brain, which are responsible for motor activity and coordination, and cause bilirubin encephalopathy (kernicterus). This condition provokes:
- increased drowsiness or extreme agitation;
- decreased sucking reflex;
- increased muscle tone in the back of the head.
Important! Parents should know that excessive readings negatively affect the functioning of the brain and biliary organs. If the skin of a newborn suddenly turns yellow-brown, you should seek medical help without delay. Only a decrease in bilirubin levels will help avoid toxic poisoning with bile pigment.
In the absence of pathology, within 2-3 weeks from the moment of birth, the level of direct bilirubin gradually decreases and returns to normal; it is during this period that the physiological jaundice of the baby disappears completely and does not return.
Important! There is no need to rush to interrupt breastfeeding, which can later become a panacea for the child. However, in order to dispel doubts and make sure that the cause of yellowing of the skin is not liver pathology, you can transfer the baby to artificial feeding for several days. If during this time the color of the skin returns to normal, it is recommended to resume breastfeeding without delay.
Bilirubin in children
The level of this substance is one of the most important indicators in the biochemical analysis of blood not only in adults, but also in children. By its level one can judge the performance of the liver, biliary tract, hematopoietic and immune systems.
The most significant indicator for health is indirect bilirubin. As mentioned above, it is predominantly synthesized from hemoglobin and is toxic to the body. If indirect bilirubin exceeds the norm for a long time, then this phenomenon leads to severe intoxication. Poisoning the body with bilirubin leads to disruption of the nervous system. This condition requires immediate medical correction.
One of the very first symptoms of an increase in the level of bile pigments is yellowing of the skin. After eliminating the cause of the disease in children, unlike adults, jaundice goes away very quickly and there is no need to use additional medications.
The level of bilirubin in children of different age groups and adults can differ significantly. Therefore, we suggest that you familiarize yourself with these indicators in the table:
| Patient groups | Norm of bilirubin in blood (μ/mol/l) | |||
| General | Indirect | Straight | ||
| Children | From birth to 4 days | 24 | 14,5 | 8,7 |
| Children of the first 4 days of life | 54,5-90 | 45,5-82,5 | 7,8 | |
| From 5 to 10 days of life | 53-70 | 45,5-64 | 7,75-8,7 | |
| From 10 and 30 days of life | 9,5-14,5 | 6,5-10,5 | 1,1-4,5 | |
| Over 1 month | Like an adult | |||
| Women | 3,2-17 | 6,5-17 | 1-4 | |
| Pregnant women | I trimester | 5-21 | 4-20 | 1-9 |
| II trimester | 5-21 | 4,5-23 | 1-10 | |
| III trimester | 5-21 | 5-24 | 1-11 | |
| Men | 3,4-17 | 16,5 | 0,7-8 | |
Consequences of increased bilirubin
The lower threshold for an extreme value is considered to be bilirubin 300 in a newborn. The consequences of such an increase can be fatal. Measures to reduce it must be taken immediately.
Fat-soluble bilirubin takes a long time to be eliminated on its own. With small indicators there is nothing terrible about this. But at high levels, bilirubin is deposited in the cerebral cortex and leads to kernicterus. Intoxication of the entire body occurs and there is a risk of developmental abnormalities. In severe cases, death is possible.
- long continuous crying;
- yellowness of the skin and sclera;
- drowsiness, lethargy;
- the baby sucks poorly;
- the child tenses and stretches his neck muscles.
We recommend reading: How to treat urticaria in adults and children at home using folk remedies and medications
Signs indicating that a child has physiological jaundice:
- the child is active;
- sucks well;
- the pigment appears from day 2 and intensifies on days 3-4;
- the yellowness gradually subsides and disappears within a month;
- no changes in stool or urine.
The degree of yellowness can be determined by the skin:
- face and neck painted;
- yellowness is visible up to the navel;
- the color of the upper limbs changes;
- the skin is all yellow.
When bilirubin is 300 in a newborn, how long this indicator will decrease depends on the child’s body and the therapy performed. It may take several days, in some cases 3-6 weeks.

The child is placed under a lamp and the boy’s eyes and genitals are covered with special glasses. The child is only taken out to eat. With severe jaundice, the child is kept under a lamp around the clock; it is possible to place the lamp above the mother’s bed and carry out treatment even during feeding. Periodically, the child should be turned onto his back and stomach so that bilirubin breaks down on all sides.
Breastfeeding has a positive effect on the removal of toxic substances from the body. It should be noted that with phototherapy, the baby's need for fluid increases by 10-20% and the number of breastfeeding may increase. Treatment is completed when the total level of bilirubin in the blood decreases.
Is bilirubin 300 dangerous in a newborn? Reviews from mothers say that it is dangerous, but only in the absence of treatment. When phototherapy is started on time, the prognosis is favorable.
Treatment of jaundice
If hyperbilirubinemia is detected in an infant, it is necessary to treat:
- Treatment of the disease that led to jaundice. Depending on the causes of the disease, both therapeutic (antiviral) and surgical (restoration of intestinal patency) methods are used.
- Drug therapy for hyperbilirubinemia. The treatment complex includes the introduction of glucose, adsorbents, antioxidants (ascorbic acid), and choleretic agents. Currently, it is rarely used due to insufficient evidence base of effectiveness.
- Phototherapy. During treatment, the child is placed under a special lamp. Light therapy causes toxic bilirubin to undergo changes to form lumirubin. The characteristics of this photoisomer are low toxicity and high solubility in water. This allows you to quickly remove bilirubin from the child’s body and reduce the damaging effect of bilirubin that has not yet been removed from the bloodstream on the child’s nervous system. Lumirubin is extracted from the bloodstream into the intestinal lumen or urine. This simple and effective method has proven itself well. It is non-traumatic for the child.
Treatment is carried out until bilirubin levels normalize. A child who has suffered pathological jaundice of newborns should be under additional supervision. If the bilirubin concentration has reached 300 - 330 µmol/l, the child receives care in a hospital setting. In this case, blood counts are monitored at least once a day. The quantitative result of studies of the level of bilirubin in the blood is the main criterion by which the result of therapy is assessed. Neither skin color nor clinical signs are such criteria.
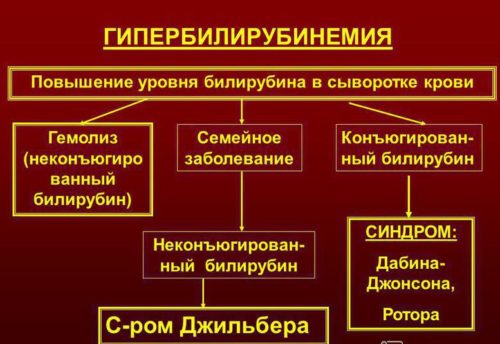
Why does bilirubin increase?
A condition in children and adults in which there is an increase in the amount of bilirubin is called hyperbilirubinemia. The breakdown of hemoglobin in the blood occurs with the appearance of bile pigment, direct and indirect. The latter must be removed from the body so that it does not accumulate in the tissues. There is a protein in the blood called albumin, which captures toxic substances and delivers them to the liver for further disposal. After processing by the liver and glucoronic acid, indirect bilirubin becomes direct and is easily excreted in bile and urine.
Liver enzymes work differently in a newborn than in an adult. It takes time for ripening to occur and for the body to cope with bilirubin itself. But until this happens, the indicators are rising, the jaundice is increasing. The higher the toxic levels, the yellower the child will be. Sometimes the palms and soles become yellow.
If a newborn has a bilirubin level of 300 on the 5th day, then medical attention is required to exclude brain intoxication. The yellowing of the child after the maternity hospital or increased jaundice should alert the mother and become a reason to contact a pediatrician. Unusual behavior of the newborn, drowsiness and lethargy require urgent hospitalization.
After the birth of a child, the level of bile pigment increases. It reaches its highest value on the third day and subsequently decreases. The best option is to increase the total pigment within 50 µmol/l. A value of 250 µmol/l on day 3 is acceptable, but requires treatment. In premature babies, the increase reaches 170 µmol/l. Bilirubin in a newborn 300 is considered critical and requires urgent hospitalization of the child.
Bilirubin content in the blood of a newborn
The first blood test is performed immediately after the baby is born. Based on the results obtained, the intensity of the increase in bilirubin concentration is subsequently determined. By the third day its quantity becomes maximum. It is believed that in full-term infants at this stage, bilirubin should not exceed 205 µmol/liter of blood , in premature infants - 170 µmol/liter .
If these values are exceeded, it is necessary to help the baby get rid of the dangerous pigment.
Causes of increased bilirubin in a newborn
Sometimes, the long-awaited meeting of a new mother with her baby can be overshadowed by the doctor’s words that the baby has increased bilirubin. What are the reasons for this phenomenon?
After birth, the baby’s body experiences enormous stress and tries to adapt to new living conditions. The manifestation of jaundice during this period indicates a massive death of the fetal red blood cells, the composition of which is not at all similar to the hemoglobin of the newborn. The epidermis and mucous crumbs acquire a light olive tint. This condition is more common in premature babies; the percentage of those born on time is much lower.
Usually starting 3-4 days after birth, this phenomenon subsides on its own at 3-5 weeks of life and is not capable of harming the baby. When breastfeeding, physiological jaundice disappears in a shorter period of time. This is due to the fact that breast milk has a laxative effect, and bilirubin is released naturally along with feces.
Children who are in a hurry to appear prematurely need phototherapy in this condition. Under the influence of light from a special lamp, bilirubin penetrates more actively into bile and urine and leaves the body faster. The procedure time is calculated separately for each child, taking into account his weight. Several sessions are allowed in one day; the tanning time is determined by the doctor.
Signs of physiological jaundice:
- Cannot appear earlier than 36 hours after birth.
- Only part of the body, up to the waist, acquires a jaundiced tint.
- Bilirubin does not cross the limit of 205 µmol/l.
- The baby is active and feeling well.
For children born at term, there is the concept of “immature”. Those. The baby may be born between 37 and 39 weeks, but his liver is not yet fully formed, “ripe,” and therefore cannot process hemoglobin into bilirubin and remove excess so that jaundice does not appear.
Consequences of high bilirubin in newborns
But it also happens that physiological jaundice turns into pathological. The reasons that can lead to complications are explained by the following factors.
- Different blood groups and incompatible Rh factors in mother and baby.
- Genetic abnormalities of the child.
- The baby's liver was exposed to the virus before birth.
- The outflow of bile is impaired in the infant.
- Intrauterine growth retardation, immaturity, premature birth.
- Formula feeding.
- Uncontrolled use of various medications by the mother during pregnancy.
All these factors provoke the development of pathological jaundice. The baby's skin color becomes greenish-yellow, the feces become lighter, and the urine, on the contrary, darkens, and the spleen and liver may increase in size.

The baby is getting worse every day, and it is no longer possible to cope without the help of doctors. Inaction of parents can lead to the next stage of pathology and possible complications:
- Poisoning of the nervous system and brain with toxins.
- Real possibility of developing albuminemia. (a drop in albumin, the main blood protein).
If bilirubin enters the brain, there is a risk of kernicterus. And it, in turn, provokes frequent convulsions, complete deafness and mental retardation. In advanced cases, the baby may experience impaired motor function.
The development of the disease depends on the causes that caused it, early contact with a doctor and timely treatment prescribed. By following these rules, it is possible to avoid complications and dire consequences.
Signs of pathological jaundice:
- Appears in the first days after birth.
- The increase in bilirubin over 24 hours is more than 85 µmol/l.
- Yellowing below the waist, palms and entire foot of the baby.
- Poor condition, lethargy or, on the contrary, overexcitability.
To correctly assess the severity of the disease, it is recommended to examine the child in natural light; electric light gives the skin a brighter color. A baby born to a mother with negative Rh is at risk and should be under the constant supervision of doctors.
There is also such a thing as milk jaundice. The baby's bilirubin increases due to breastfeeding. It is believed that the reason for its appearance is the fatty acids contained in mother's milk and a high level of hormones. These elements can disrupt liver function and inhibit the conversion of bilirubin.
We recommend reading: Bifidumbacterin: indications for taking the medicine, dosage and contraindications, instructions for use
To identify the connection between jaundice and milk, you need to switch the baby to formula for a short time and monitor the bilirubin. If his performance began to fall, then the assumption is correct.

But to conduct such a test, it is not necessary to deprive the baby of mother’s milk. You can feed expressed milk by preheating it to 50 degrees and then allowing it to cool to body temperature. This treatment helps reduce the activity of substances in milk that prevent the baby’s enzymes from working at full capacity.
Such jaundice cannot cause complications. Breastfeeding can be continued; it is even recommended to apply it to the breast as often as possible so that bilirubin passes out faster with meconium.
Treatment of pathological jaundice
Pathological jaundice of newborns is detected already in the first days after birth.
It can occur due to incompatibility of the blood type or Rh factor of the mother and the child, infectious liver diseases or intestinal obstruction in the newborn, or premature birth. This type of jaundice is more dangerous than physiological jaundice. Bilirubin, the concentration of which increases every hour, is practically not excreted from the newborn’s body. Accumulating in the blood, the pigment can reach the brain after some time. For cells of the nervous system, bilirubin is a poison.
Pathological jaundice is treated in a hospital setting . In severe cases, the neonatologist may prescribe blood transfusions and hormonal drugs. Basically, therapy uses droppers and medications that improve liver function and promote the excretion of bilirubin.
Indirect, direct and total bilirubin
Bilirubin has three varieties (fractions).
Indirect bilirubin (unbound) is quite toxic, practically water-insoluble, but tends to combine well with fats. If the liver’s mechanism for processing indirect bilirubin suddenly goes wrong, it, having the property of penetrating into cells, begins to accumulate in fatty deposits. It can only be removed from the body by converting it directly using gastric enzymes.
Direct bilirubin (bound) is its indirect fraction that has been processed by the liver. It is absolutely non-toxic and perfectly soluble, due to which it has no problems with excretion.
Total bilirubin as such does not exist in nature; it is the sum of two types, direct and indirect.
What is bilirubin
At birth, the baby's hemoglobin level is quite high. Being in the mother’s stomach, this level of red blood cells was necessary for the baby to function normally. But after his birth, his body began to work a little differently and the baby no longer needed such high hemoglobin, so it began to break down.
The rapid destruction of hemoglobin is accompanied by the release of bilirubin into the blood; this process is so fast and rapid that the baby’s body does not have time to remove the breakdown products and bilirubin accumulates in the blood.
The development of the disease depends on the causes that caused it, early contact with a doctor and timely treatment prescribed. By following these rules, it is possible to avoid complications and dire consequences.
Bilirubin
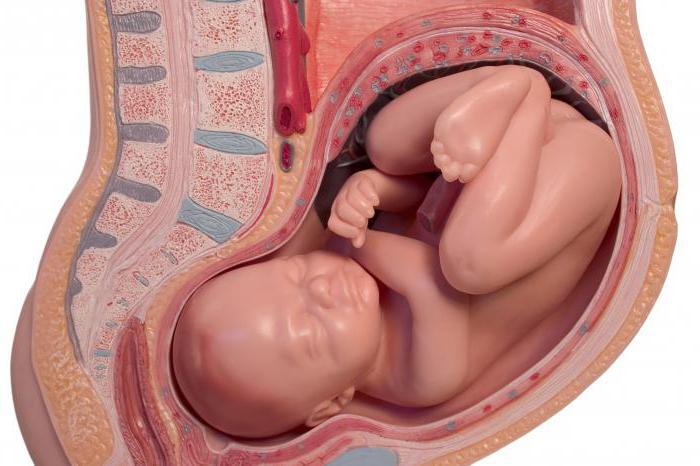
Even in the perinatal period, when the child’s internal organs are developing, bilirubin is already released in the baby’s body. Its formation is associated with the destruction of red blood cells - erythrocytes.
While in the mother's womb, the baby does not yet breathe on its own. The supply of oxygen received through the placenta occurs through a separate group of red blood cells. They cease to exist with the birth of a child. Bilirubin, which is obtained as a result of the decomposition of these red blood cells, has a special structure. It does not dissolve and cannot be excreted in urine. The accumulation of this substance causes intoxication of the newborn’s body, which is accompanied by a change in the color of the skin and whites of the eyes.
Liver cells convert bilirubin into a soluble form. But she is not always ready to fulfill her functions. In premature babies, the liver is not yet fully formed, so it cannot withstand additional stress. The concentration of bilirubin increases every day, and the child’s body is not yet ready to transform and remove pigment in such quantities. Sometimes newborn jaundice can also occur in full-term babies. It may go away on its own within 1-2 weeks after birth.
What tests need to be taken to determine the level of pigment?
A blood test is the very first and most important examination that needs to be done in a child’s life. After birth and umbilical cord cutting, blood is taken for general examination. The test reveals the group, the Rh factor, and how many different substances are contained. The pigment in the source material is determined in three forms and their ratio:
- general (both states in total);
- straight (free) – no more than a quarter;
- indirect (related) - from 75%.
Jaundice in a newborn is diagnosed when the maximum permissible value of the indicator is 256 µmol/l in full-term babies and 171 µmol/l in those born prematurely. Detection of the amount of a substance in the plasma is extremely important in children under one year of age with hemolytic disease, jaundice regardless of etiology, cirrhosis, hepatitis, toxin poisoning, suspected oncology, taking large doses of medication, pathologies of the gallbladder to identify stones, patency of the ducts.
Before taking a biochemical blood test for bilirubin, certain conditions must be met, otherwise the result, and therefore the diagnosis, will be unreliable. Blood is collected on an empty stomach. The result is known within a few hours.
How to test for bilirubin in newborns?
A blood sample is used to assess the amount of bilirubin in a child's body. To obtain reliable results, blood is taken exclusively on an empty stomach to determine this substance. You should not eat for eight hours before the test. Due to the nature of the study, results can be obtained literally on the same day.
To more fully assess the child’s condition, you should undergo an analysis that takes into account the percentage of fractions. This technique is especially important when identifying the causes of jaundice in newborns. The baby’s bilirubin level is an excellent indicator of the functioning of his body, so such an analysis will help to establish pathology at an early stage of its development.
You can learn how to treat stomatitis in a child from our article. You can find out what time a baby starts crawling here.
You can find out about atopic dermatitis in a child by following the link
Why does my baby have high bilirubin levels?
The appearance and development of pathological processes in the liver is the main cause of physiological jaundice in newborns. The first priority, if the bilirubin level has increased or decreased from acceptable values and does not decrease by the third week, is to diagnose the original disease.
Without identifying the root cause - the illness that caused the deterioration of the newborn's condition - it is impossible to prescribe the correct treatment.
Can total, indirect bilirubin rise again after falling? Pathological reasons causing an increase in pigment in the blood plasma:
- liver problems due to damage to the parenchyma;
- hepatitis, cholecystitis;
- long-term disruption of the normal flow of bile into the intestines;
- hereditary factors;
- diabetes mellitus of one parent;
- too intense breakdown of red blood cells;
- digestive system infections;
- congenital disorders of the cardiovascular system;
- deficiency of vitamins, microelements, in particular vitamin B12;
- hormonal imbalance;
- taking medications (analgesics and antibiotics affect the removal of pigment);
- hemolytic anemia;
- malaria.
If a baby over 1 month old has yellowing of the skin, this is a reason to immediately contact a pediatrician. The provoking factor may be any of the above reasons. A timely examination will allow you to identify the root cause of the pathology and prescribe treatment.
Exchange blood transfusion
If the amount of pigment in a newborn increases due to hemolytic disease, exchange transfusion is used for treatment (when a little blood is first taken from the child and then the same volume of donor material is infused). Hemolytic disease is a conflict between the blood of the mother and the child, in which the baby’s red blood cells die. An overestimated indicator in this case is one of the symptoms of the disease. The indicators will constantly increase, so action must be taken immediately. Thanks to this procedure, the newborn's blood is cleared of maternal antibodies and excess bilirubin.
Exchange transfusion is considered necessary if the amount of the substance exceeds 428 µmol/l.








