Home Miscellaneous
6 Mar 2020, 20:00 Anna 2 451 No
The pancreas is located very close to the stomach; it does not have a definite shape, as it constantly twists in different directions. Such changes are considered normal, but in some cases, bending of the pancreas can be dangerous. Sometimes the pancreas can bend around the duodenum and squeeze it, this is very bad.
Pancreas shape
Normally, the shape of the gland varies. It happens:
- elongated (in some children all its sections - head, body, tail, are almost on the same line),
- bent at a certain angle,
- in the form of the letter L,
- dumbbell-shaped
- rolled into a ring.
Sometimes, after an examination, parents are informed that the child has a bend in the pancreas. This causes anxiety and wariness. But such an arrangement does not pose a danger to digestion or general health, with the exception of the last one. All these forms are a variant of the norm.
Thanks to its connections with the duodenum and peritoneum, it is firmly fixed and does not change its location in relation to neighboring organs depending on the location of the child’s body.
4Is it dangerous
Changing the shape of the gland is not dangerous for a person if it does not cause him discomfort and does not disrupt the digestion process.
The only critical situation is when the deformed organ is wrapped around the duodenum in the form of a tight ring. The resulting acute intestinal obstruction is life-threatening.
Doctors have found that the shape of the pancreas does not affect the quality of the organ’s functioning and does not in any way affect the patient’s well-being. Its deformation does not necessarily indicate that a person has any disease, but only serves as a reason for regular visits to the doctor and an in-depth examination of the abdominal organs. For this, the patient is referred to diagnostic procedures that are more informative than ultrasound: computed tomography or magnetic resonance imaging.
Deformation
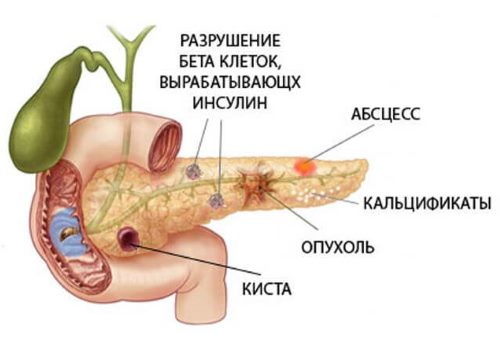
If the bend of the gland is non-pathological (except in rare cases), then the deformation should be monitored over time. Main causes of deformation:
- acute pancreatitis,
- cyst,
- tumor,
- developmental anomalies,
- injuries,
- poor nutrition.
Deformation does not always entail the development of severe pathology or is its manifestation. But it must be identified when the child is still small. This is necessary for further correction in the event of the development of other pathological changes.
Why is the pancreas deformed in children?
Since the pancreas is a rather vulnerable organ, the numerous pathologies that develop in it can lead to changes in the size and shape of the organ - deformation, which can occur with or without displacement of the gland.
Acute pancreatitis
In acute pancreatitis, as a result of swelling of the gland, it may move slightly upward. As a result, its shape changes: this can be expressed in an angular bend or multiple bends. Such deformation is more common when the process is chronic.
Cysts
Deformation develops in the presence of cysts - liquid formations limited in the organ tissue by a capsule. The cyst can reach different sizes, does not cause any subjective sensations - the baby feels normal, so it cannot be detected without additional diagnostic methods. The cyst is an incidental finding during ultrasound. Congenital cysts are found in children.
Polycystic disease is a large number of cysts of different sizes. Reminds me of a honeycomb. It is found during a generalized process in the parenchyma of the liver, spleen, kidneys, and ovaries.
Neoplasm
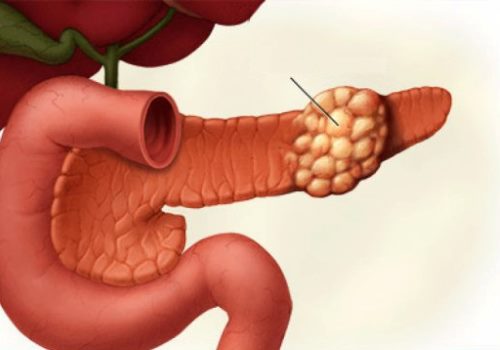
Another cause of deformation is tumor. It can develop in any part of the gland. In this case, the contours of the organ can be greatly disrupted, the boundaries become lumpy and unclear. It is rarely diagnosed in children.
Developmental anomalies
Developmental anomalies play a role in the bending of the pancreas in a child from birth. They do not depend on how the pregnancy proceeded. With all congenital pancreatic defects, the newborn feels normal. This doesn't bother him.
The ring-shaped pancreas surrounds the duodenum at any level, leading to obstruction. It is difficult to differentiate from pancreatic head cancer that grows into the intestinal wall.
Aberrant gland - a rounded formation up to 2.5 cm is found in the wall of the duodenum or gallbladder, similar in echogenicity to pancreatic tissue. But it is rare in children.
Duplicate pancreas - cases of a body and tail with one head of the pancreas, as well as two complete glands located in parallel, have been described.
Injury
In case of injury, the gland increases in size on the second day. It enlarges and loses its contours on ultrasound. A round formation without clear contours is determined - hematoma or necrosis, disrupting the correct shape of the gland. This picture is observed with a mild closed injury.
In case of severe injury accompanied by a rupture, in the first hours only the head or part of the body is identified. Subsequently, due to bleeding and leakage of pancreatic juice, the contours become blurred, and the organ increases significantly and unevenly in size.
Bend or bend of an organ?
In medical terminology, there is no concept of bend, bend, or inflection of the pancreas. Elastic tissues allow the organ to bend, straighten and even curl into a ring. The diagnosis of bending of the pancreas does not exist due to the absence of a threat to the health and life of the patient. A bend is dangerous only if the pancreas encircles the duodenal bulb in a ring - this is accompanied by clinical manifestations.
Diffuse changes in the liver and pancreas (Hepatomegaly) - what is it?
Let's like and subscribe to the channel. New materials are published daily!
If you want to support the project, there is a donation form at the end of the page. Thank you for your attention!
With the development
of hepatomegaly, diffuse changes in the liver and pancreas are observed.
Symptoms can be pronounced or blurred. Only a doctor can diagnose the disease and prescribe the necessary comprehensive treatment.
Hepatomegaly: ICD code
Hepatomegaly is included in the ICD 10 standard document by the World Health Organization. The disease is assigned to group R 16.
Symptoms of hepatomegaly
Symptoms of hepatomegaly are associated with the causes that caused this disease.
The main sign is the ability to easily feel its increase during palpation.
During the examination, the patient complains of pain.
Hepatomegaly also has the following symptoms:
- swelling;
- enlarged kidneys;
- nausea or vomiting;
- distortion of taste;
- aversion to certain foods;
- heartburn;
- yellowness of the skin;
- increased fatigue;
- odor from the mouth;
- itching;
- abdominal discomfort;
- diarrhea or constipation;
- the appearance of age spots on the face.
Kinds
The disease is divided into types with characteristic features for each:
- Unexpressed hepatomegaly
is expressed in a slight increase in the size of the liver. The disease is diagnosed in young children. If the child does not have negative symptoms and his health does not cause him discomfort, the doctor does not prescribe treatment. Most often, this type of hepatomegaly goes away on its own over time. If, over time, an increase in the organ is observed, the doctor selects complex therapy. - Severe hepatomegaly
is diagnosed if the organ has increased to 5 cm or more. Because of this, there is an increase in the volume of the abdominal cavity, which can be observed upon visual examination. As the disease progresses, a person develops leukemia or hemoblastosis. - A moderately pronounced form
is characterized by a slight increase in size, which exceeds the norm by up to 2-5 cm. In this case, the patient rarely experiences negative symptoms. If you follow a diet and do not drink alcohol, the organ can recover on its own and eventually return to its normal size. If the liver is moderately enlarged, drug therapy is prescribed only when negative symptoms begin to appear over time.
Hepatomegaly of the left lobe
Hepatomegaly due to the left lobe is rare. An enlarged organ can be caused by infections or problems with the heart, spleen, or kidneys. Due to the location of the left lobe close to the pancreas, the development of the disease can begin due to pancreatitis or due to diffuse changes.
Hepatomegaly of the right lobe
This form of the disease is diagnosed frequently. The increase occurs due to genetic characteristics. Inflammatory diseases, toxins, and abuse of certain types of foods can provoke hepatomegaly. Hepatomegaly of the right lobe negatively affects the entire body, since it performs 60% of all the necessary functions of the liver.
Diffuse
With this form, the organ increases in size from 12 cm and above. Diffuse changes affect any part. This damages nerve endings and negatively affects blood circulation and bile excretion. Changes occur due to infectious processes. This form is characterized by the following negative symptoms:
- increased heart rate;
- aching pain is felt;
- pain radiates to the arm or shoulder blade;
- if the disease is provoked by alcoholism, there is an increase in the size of the spleen;
- severe chills appear.
Drug treatment does not help with this form. Patients are prescribed surgery.
Partial
The organ enlarges unevenly. One of the shares may be larger and the other smaller. Irregularities may be observed along the lower edge of the liver. During palpation, lumpiness and unevenness of the surface are felt.
Hepatomegaly and splenomegaly
Diseases can occur simultaneously. And if hepatomegaly is characterized by an increase in the size of the liver, then splenomegaly is characterized by an increase in the size of the spleen. This form of the disease is caused by:
- Gaucher disease;
- impaired blood circulation in the veins of these organs;
- parasites and infections;
- gallbladder disease;
- heart disease;
- pericarditis;
- tuberculosis;
- malaria.
Due to fatty liver disease
A disease that develops against the background of fatty hepatosis appears when the degeneration of healthy cells into fatty cells begins. The disease is provoked by alcoholism, frequent use of medications, a regular diet or frequent fasting, abuse of probiotics and fatty foods. Fats are not processed, but accumulate in cells, which provokes the development of hepatomegaly due to fatty hepatosis.
Hepatomegaly in the fetus
In the fetus, the disease is associated with severe enlargement of the organ. The doctor’s task during diagnosis is to identify the factor that provoked the disease. Most often this is due to:
- with intrauterine infection;
- due to metabolic failure;
- if a woman has had syphilis.
In newborns
Hepatomegaly in newborns is mild.
The increase is a maximum of 2 cm. The disease can be caused by many factors:
- poor nutrition;
- vaccination;
- autoimmune diseases;
- infections;
- malignant formations;
- blockage or ducts;
- Debre's syndrome;
- Gierke's disease;
- Mauriac syndrome;
- echinococcosis;
- Waringer's syndrome.
Hepatomegaly can be identified by the following symptoms:
- vomiting or nausea;
- yellowness of the skin;
- the appearance of pigment spots;
- swelling of the navel;
- diarrhea;
- anemia;
- lethargy.
All symptoms are also typical for older children.
Methods for diagnosing pathology in children
The retroperitoneal location of the pancreas does not make it possible to palpate it and determine changes in size, shape, and additional formations. Pathological changes in it do not always manifest themselves as complaints and clinical symptoms.

In cases of deformity associated with acute or chronic pancreatitis, a diagnosis can be made based on:
- complaints,
- a detailed history,
- laboratory data.
The disease has clinical manifestations that are not specific, but on their basis an inflammatory process can be suspected:
- acute onset
- febrile temperature (38–39 degrees),
- pain in the navel area, in the left hypochondrium or surrounding pain,
- nausea and vomiting that does not bring relief,
- diarrhea.
Laboratory tests will help confirm the diagnosis:
- general blood analysis,
- biochemical tests of blood and urine for elevated levels of amylase and other enzymes - a sign of pancreatitis,
- coprogram
- fecal elastase analysis.
If even after this the picture does not clear up, they do sonography (ultrasound), and, if necessary, CT. Ultrasound reveals a swollen organ, a change in its echogenicity and a slight curvature with an upward displacement of the organ.
In other cases of deformity, the main diagnostic method is ultrasound or CT, since clinical manifestations are most often absent and laboratory data are uninformative. If a tumor is suspected, an MRI is performed and a biopsy with histological examination is performed.
Bend of the gallbladder: symptoms and treatment, causes of the disorder
Patients often turn to a gastroenterologist with complaints of constant nausea, a feeling of heaviness in the side and other symptoms of digestive disorders; during the examination, it turns out that the cause of this is a kink in the gallbladder.
Gallbladder bend - What is it?
Normally, the gallbladder has the shape of an oblong sac and is a reservoir for storing bile.
A kink in the gallbladder is an abnormal condition during which constrictions occur in the organ, causing the bladder to take the shape of an hourglass, a hook, or the letter “G.”
When a bend occurs simultaneously in several places, the gallbladder resembles the shape of the Latin letter “c”; this pathology is most often found in pediatric practice.
Causes of gallbladder bending
General view of the gallbladder, structure, photo
There are congenital and acquired inflection of the bladder. Congenital occurs at the stage of embryogenesis, at approximately 5-6 weeks of gestation, when the liver and gall bladder of the embryo are formed. The development of this pathology can be provoked by various factors of the internal and external environment:
- Pregnant women taking medications up to 12 weeks
- Drinking alcoholic beverages and smoking tobacco,
- Past viral and infectious diseases,
- Chronic diseases in the mother,
- Unfavorable environmental conditions in which the pregnant woman lives.
A congenital inflection is also called a persistent or fixed disease of the gallbladder, however, since the cavity of the organ is lined with muscle fibers that tend to contract, the pathological process can periodically change its location. In this case, the patient is diagnosed with a labile inflection of the gallbladder.
Acquired bending of the gallbladder is a consequence of the following reasons:
- Violation of diet, predominance of fatty, spicy, smoked foods in the diet,
- Exhaustive diets
- Obesity,
- Metabolic disease,
- Past foodborne illnesses,
- Weight lifting,
- Sedentary lifestyle,
- Cholecystitis,
- Cholelithiasis,
- Previous operations on the gallbladder or liver,
- Pregnancy,
- Long-term and uncontrolled use of certain medications,
- Concomitant diseases of the duodenum, liver, pancreas.
The gallbladder has a body, a fundus and a neck. Depending on the location of the pathological process, kinks of the upper or lower third of the organ, neck or body are distinguished. A bend in the body of the gallbladder is the most dangerous condition and entails serious complications.
Signs and symptoms of a kinked gallbladder
Characteristic clinical symptoms of gallbladder inflection are:
- Constant bitterness in the mouth
- Nausea,
- The appearance of bad breath,
- Gray or yellowish coating on the tongue,
- Belching,
- Bloating and increased gas formation,
- Heartburn,
- Feeling of heaviness in the stomach, especially after eating,
- Vomiting when eating fatty, fried, smoked,
- Stool disorders (diarrhea followed by prolonged constipation).
When stones form in the ducts of the bladder against the background of constant stagnation of bile, the patient sometimes experiences yellowness of the skin and visible mucous membranes.
Periodically, the organ itself and the bile ducts become inflamed, as a result of which the patient develops cholangitis or cholecystitis, the symptoms of which are:
- Pain in the right hypochondrium,
- Nausea and vomiting,
- Diarrhea,
- Increase in body temperature to 38-39 degrees,
- Refusal to eat
- Yellowness of the skin and mucous membranes,
- Attacks of biliary colic.
A bend in the gallbladder in an infant before the introduction of complementary foods may not manifest itself clinically, however, after the inclusion of adult food in the diet, constant regurgitation and stool disturbances are possible. The S-shaped bend of this organ in a young child is in most cases the main cause of a common pathology - biliary dyskinesia.
Diagnostics
The main method for diagnosing gallbladder pathologies is ultrasound. This method has no contraindications or age restrictions, so it is prescribed even to the youngest patients if a bend is suspected.
Using ultrasound, you can accurately determine the functionality of the organ, the presence of a bend, as well as the location of the pathological process.
In order to find out whether the bend is congenital or acquired, adult patients undergo stimulation of the secretory abilities of the organ by taking raw egg yolks or butter.
With congenital bending, the deformation of the bladder after increased bile production remains unchanged. To determine the probable cause of the anomaly, the gastroenterologist collects a thorough history of the patient’s life. Depending on the cause of the gallbladder bend, the doctor will prescribe appropriate treatment.
Treatment of gallbladder inflection
For the congenital form of the pathology, treatment consists of reducing the symptoms of gallbladder bending by following a special diet and performing simple physical exercises that stimulate the normal flow of bile.
Herbal teas and decoctions of medicinal herbs - corn silk, mint, yarrow, immortelle flowers - help improve organ function and prevent congestion.
Drug therapy
In order to prevent stagnant processes and stone formation when the gallbladder is bent, choleretic drugs are prescribed, for example, Allochol, Gepabene.
These drugs can only be taken with the permission of a doctor and if there are no stones in the bladder or ducts. Otherwise, therapy with choleretic agents leads to blockage of the ducts with stones and the development of an acute inflammatory process or dangerous conditions requiring surgical intervention.
When diagnosing congestion and stones in a bladder with a diameter of no more than 5 mm, Ursohol or Ursofalk are prescribed - drugs that change the viscosity and composition of bile, normalize its outflow, and destroy small stones. For pain and spasms in the area of the right hypochondrium, No-shpu, Papaverine or analgesics are prescribed.
For inflammation of the ducts or gallbladder, a course of anti-inflammatory drugs or antibiotics is indicated.
Diet for gallbladder bending
In order to improve the patient’s general condition and reduce the severity of clinical symptoms of bladder inflection, adherence to therapeutic nutrition is indicated (table No. 5a). The following are completely excluded from the diet:
- Baking,
- Confectionery – pastries, chocolate, candies, cakes, straws, puff pastry,
- Fatty meats and fish - pork, lamb, mackerel, salmon,
- Salo,
- By-products,
- Spices, vinegar, herbs, spicy dishes,
- Mushrooms,
- Sausages,
- Pasta,
- Legumes,
- Sour cream, hard cheese,
- Strong broths
- Red caviar.
Limit butter and chicken egg yolks.
The basis of the diet is boiled porridge (cooked in water with the addition of milk if desired), low-fat cottage cheese, lean meat, kefir, yogurt, day-old bread, vegetables, fruits, herbs, low-fat fish (pike perch, hake, pollock). Dishes are prepared by steaming or boiling; meals should be frequent and in small portions.
Treatment of kinks at home
If there are no stones in the gall bladder or ducts, the patient can undergo tubage or so-called blind probing at home once a month.
The essence of the procedure is that the patient first takes a solution of magnesia or sorbitol, after which a warm heating pad is placed on the right hypochondrium for 30 minutes.
Under the influence of heat and a concentrated solution of sorbitol or magnesia, the sphincter of Oddi (located in the gallbladder) opens, the contractility of the gallbladder increases and the accumulated bile is released into the intestinal lumen.
Bile has an irritating effect on the intestinal mucous membranes, as a result of which the patient experiences several times liquefied green or yellow stool - this is normal.
After this procedure, patients note a significant improvement in their well-being, the disappearance of the feeling of heaviness, nausea and bloating.
A strict contraindication to tubage is the presence of stones of any diameter in the gallbladder or ducts, obstruction of the ducts, or the presence of any neoplasms in the organ that impede the outflow of bile.
Complications
When the bladder is bent, bile accumulates in the organ and changes its viscosity, resulting in the gradual formation of stones. A dangerous complication of this condition is the displacement of the stone into the lumen of the bile ducts, which blocks the path of bile outflow (duct blockage).
Such a complication poses a threat to the health and life of the patient, so in such situations immediate surgical intervention is often required.
Loading…
Source: https://afgsm.ru/bolezni/peregib-zhelchnogo-puzyrya-simptomy-i-lechenie-prichiny-narusheniya
Therapy of the disease
Therapeutic treatment is necessary only in case of acute inflammatory process. Tumors are observed from the first days and treated by oncologists. In case of injury, tumor, compression of the duodenal bulb by the parenchyma of the gland and the development of intestinal obstruction in this place, treatment is surgical.
Medicines

Pancreatitis is a common cause of the appearance of an angular bend, which appears with an acute onset. With timely and adequate treatment, the iron returns to its normal position. Therefore, it is necessary to begin therapy as early as possible using:
- antispasmodics,
- painkillers,
- antibacterial,
- anti-enzyme,
- enzymatic agents.
According to the famous pediatrician Evgeniy Komarovsky: treatment of pancreatitis necessarily includes therapeutic nutrition.
Phytotherapy
Herbal medicine is not suitable as a method of treating pathology that has caused bending or deformation of the pancreas. In acute pancreatitis or during exacerbation of a chronic process, it is contraindicated: it can worsen the course by adding an allergic component. The disease is too serious and can cause severe complications, often leading to death, so the use of medicinal plants for its treatment is not recommended. Similarly - when a gland tumor is detected.
In other cases (in case of injuries, congenital anomalies, cysts), the method is ineffective.
Physiotherapy
Physiotherapeutic methods of treatment are used only for pancreatitis: in the acute phase, when the child cannot eat, warm mineral alkaline water without gas is used. The frequency and volume of fluid you drink is determined by your doctor. After 2–3 weeks, in the phase of unstable remission, symptomatic physiotherapy is used to:
- relieving spasms,
- improving the outflow of pancreatic juice,
- anti-inflammatory action,
- restoration of blood circulation in the affected organ,
- improving motility of the stomach and duodenum.

An effective method is:
- electrophoresis with novocaine, antispasmodics (papaverine, platiphylline, No-Shpa), liquid mud preparations (medicinal mud, peloidin, humisol),
- Ultrasound in pulsed mode relieves pain well and normalizes gastric secretion.
Indications for treatment
In 80% of cases of abnormalities, no treatment is required. The altered gland functions normally and does not lead to a deterioration in the patient’s condition.
Medical intervention is required if the following symptoms are present:
- stomach ache;
- chronic dyspepsia;
- stool disorders;
- signs of intestinal obstruction;
- jaundice;
- chronic pancreatitis;
- insulin deficiency (diabetes mellitus).
The patient is hospitalized in all cases of planned surgical intervention. Conservative therapy is carried out on an outpatient basis.
Prevention methods
It is almost impossible to prevent the development of congenital deformation of the pancreas, since it occurs at the stage of embryonic development in the first months of pregnancy.
The expectant mother should eat right, lead an active lifestyle and forget about smoking, drinking alcohol, and medications that affect the fetus. Chronic infections should be identified and treated before conception.
Considering the fact that pancreatitis is the main cause of structural changes in the gland, it is necessary to prevent this disease in a child. To do this, parents can carry out the following activities:
- Timely identify and treat diseases of the digestive tract, liver and biliary tract.
- Exclude fatty, spicy and fried foods, “stall” food from your diet, and limit your consumption of fast food.
- Organize diet and complementary feeding in accordance with age.
- Vaccinate the child according to the vaccination schedule and according to epidemic indications.
- Prevent infection by viruses, bacteria, parasites.
Functional curves arise due to the anatomical and physiological characteristics of the child’s body; they cannot be prevented and, apart from dynamic observation, no action is required.
You can find out about drugs for the treatment of pancreatitis in children here...
lechigastrit.ru