Spasms in the intestines bother the patient for various reasons. Colicky pain is associated with gastrointestinal disorders. Causes may include poor nutrition, surgery, medications, and diseases of the gastrointestinal tract. All of the above factors lead to stomach cramps.
Intestinal spasm is a rapid and prolonged muscle contraction, characterized by a delay in the relaxation phase. Spasm of the transverse muscles is called a cramp, while spasm of the smooth muscles is called colic.
Most often, intestinal spasm develops in the small intestine, after which the pathological contraction can spread throughout the digestive tract, when intestinal colic becomes generalized.
Treatment of colic
For patients with sensitive intestines, a set of lifestyle changes with drug and non-drug therapy is indicated. It includes:
- dietary diet, eating by the hour;
- physical therapy classes, walking, yoga, aerobics;
- limiting psycho-emotional stress, breathing exercises for relaxation, meditation;
- general relaxation massage;
- water procedures with a calming effect - baths with pine needles, valerian, herbal extracts;
- psychotherapeutic sessions;
- electrosleep;
- taking sedative medicinal teas or natural-based medications at night (Persen, Sedafiton, Novo-Passit, tinctures of peony, valerian, motherwort);
- antispasmodics – No-shpa, Riabal, Buscopan;
- antidiarrheals – Imodium, Uzara or laxatives – Dufalak, Regulax;
- means for restoring microflora - Bifiform, Linex, Hilak forte.

First aid
If colic is detected in the abdomen, you must contact a medical facility.
At the first attack, you need to take a comfortable position, relieve pressure with clothing on the abdominal area, and you can drink a painkiller. Recommendations include taking a warm bath and drinking warm drinks.
If the attack does not go away or recurs, you must call a doctor. In any case, after an attack of colic, even a single one, it is necessary to consult a specialist to find out the causes of the spasms and determine further actions - what and how to treat.
Doctors do not recommend taking any action before their arrival, since by eliminating the symptoms, you can complicate the process of finding out the causes of their occurrence, just as they warn against the use of painkillers and thermal procedures. In this case, it is better to apply a cold compress.
In order to determine the necessary therapeutic procedures, it is necessary to carry out a minimum diagnosis, which is done in any medical institution.
Diet food
The diet is based on the prevalence of diarrhea or constipation.
What to exclude
All patients need to avoid overeating and eating foods that stimulate the secretion of bile and gastric juice and irritate the intestinal mucosa. These include:
- rough, fibrous foods;
- fried, fatty, difficult to digest dishes consisting of a large number of components;
- alcohol;
- spinach, onions, garlic, especially raw;
- hot seasonings, industrial sauces, horseradish, mustard;
- fatty meats and fish;
- canned, smoked, pickled products, pickles.
Diet rules for constipation
It is important to ensure sufficient fluid intake - at least 1.5 liters of clean drinking water in addition to drinks and first courses. It is recommended to eat five meals a day, strictly according to the clock. This is due to the fact that the entry of food components into the stomach reflexively stimulates bowel movements, so if you have constipation, you should not allow long breaks between meals.
The diet should be dominated by plant foods containing fiber and pectin, especially salads made from fresh vegetables and herbs. They should be included in the diet at least 400 g. Boiled, stewed vegetables, and fruit juices are also useful. There is no need to chop the food, but you should chew it thoroughly, do not move around while eating, and do not be distracted by external irritants.
Products with a laxative effect
Recommended products include:
- the most useful vegetable dishes are carrots, pumpkins, zucchini, beets, broccoli, cauliflower, tomatoes;
- cabbage (not tolerated by everyone) - Beijing and white cabbage, pickled, sea cabbage;
- greens - lettuce, celery, cilantro, dill;
- dried fruits – figs, dried apricots, prunes;
- legumes (if tolerated) – green peas, green beans, soy cheese;
- bread – rye, grain, crispbread;
- low-fat meat and fish for soup, boiled, baked;
- cereals for first courses, side dishes, casseroles;
- butter and vegetable oil;
- cottage cheese, yogurt, curdled milk, kefir, cheese, sour cream;
- weak tea, coffee with milk, juices from sweet fruits and berries, preferably cool or cold;
- melon, apricots, plums.
For the first course they prepare borscht, beetroot soup, okroshka, with pearl barley and vegetables. It is not advisable to add rice, semolina, or vermicelli. Constipation is aggravated by jelly, ground porridge, quince, and blueberries.
Menu for constipation
If there is a violation of regular bowel movements, nutrition is based on the following approximate menu:
- pumpkin porridge, cereal flakes with prunes, rosehip infusion;
- cottage cheese casserole with figs and apricots;
- borscht, boiled chicken, beetroot and seaweed salad with olive oil and herbs;
- fish stew with vegetables, buckwheat porridge;
- yogurt, cookies.
Diet and menu for diarrhea
All dishes are boiled, baked in the oven. No chopping is required, but it is necessary to boil cereals, vegetables, and meat well. In food you can use:
- soup in a weak broth of meat, fish, with meatballs, quenelles;
- dried white flour bread;
- cutlets and meatballs made from steamed minced meat and fish; fish can also be baked or boiled in pieces;
- porridge (except millet, pearl barley) in water, broth;
- pasta for soup, side dish, casseroles;
- fermented baked milk, kefir, cottage cheese, curdled milk, yogurt;
- butter;
- eggs – 1-2 per day;
- boiled potatoes, carrots and cauliflower, greens;
- sweet berries and fruits, citrus fruits, their juices.
To create a dietary diet, the following indicative menu is proposed:
- steam omelette, tea;
- cottage cheese casserole with pasta, blueberry jelly;
- rice soup with pollock meatballs, croutons, rosehip broth;
- mashed potatoes with boiled meat, stewed carrots with zucchini;
- kefir with biscuit.
Causes of cramps in the intestines
Intestinal cramps can be caused by a number of factors:
- Bacterial gastroenteritis.
This disease is characterized by cramping pain in the intestines, bloating and nausea. Occurs due to the entry of bacteria into the microflora of the human body.
- Duodenitis.
The disease is associated with damage to the duodenum. The patient feels colicky pain in the stomach area. Pain syndromes increase during coughing. Duodenitis is an inflammatory disease of the duodenum. The diagnosis is most common in male patients.
Duodenitis can be caused by excessive consumption of alcoholic beverages, fried and floury, salty foods. Poisoning with toxic substances and medications also leads to the development of duodenitis.
- Dysbacteriosis.
Dysbiosis is an excess, deficiency or imbalance in the number of beneficial and harmful microorganisms in the intestines. The disease can develop due to increased acidity in the human body. Dysbacteriosis appears in a weak body after using antibiotics.
A special factor in the development of dysbiosis is that the intestines cannot independently promote its contents. Dysbacteriosis actively develops if pathogenic microbes or parasites actively multiply in the intestines (dysentery, viral diseases, salmonellosis, helminthiases, lamblia).
- Pathogenesis.
A complex inflammatory process develops in the body. The patient feels colicky pain, severe cramps, bloating and nausea. During the development of pathogenesis, the patient experiences sharp cutting pain in the lower abdomen. Pathogenesis in advanced cases is removed by surgery.
- Increased sensitivity.
People with weakened bodies have increased sensitivity. The body is very susceptible, affected by infections, allergies and inflammatory processes. With increased sensitivity, the patient is often tormented by colicky cutting pain, flatulence, diarrhea or constipation, bloating, nausea and vomiting.
- Impaired intestinal motility.
If intestinal motility is impaired, the patient experiences frequent gastrointestinal disorders. The patient suffers from constipation and disorders, he feels discomfort in the intestinal area.
Dish recipes
To prepare dishes for intestinal colic, you can use the following recipes.
Porridge made from pumpkin, cereal flakes and prunes

For porridge that simulates intestinal function, you need to take:
- pumpkin – 400 g,
- cereal flakes - 2 tablespoons,
- prunes – 50 g,
- walnut kernels – 20 g,
- cinnamon – 2 g.
The pumpkin is peeled and cut into cubes. Prunes are doused with boiling water. Pour 2 cm of water into the bottom of the pan and add pumpkin with prunes, add cinnamon and sugar if the pumpkin is not sweet. Simmer over low heat until soft, add flakes and cook for another 7 minutes. When serving, sprinkle with nut slices.
Cottage cheese casserole with pasta

To prepare the dish you will need:
- cottage cheese – 500 g,
- pasta – 100 g,
- yogurt (kefir) – 150 g,
- egg - 1 piece,
- sugar – 3 tablespoons,
- vanilla sugar – 3 g.
Boil the pasta in salted water until almost done. Beat cottage cheese, yogurt, egg, regular sugar and vanilla with a mixer, mix with pasta. Place in a greased form, bake in a multicooker in the “baking” mode or in the oven at 180 degrees for 40 minutes.
Fish stew with vegetables

For a light and juicy dish you will need:
- fillet – 200 g,
- zucchini - half medium,
- yellow bell pepper – 1 piece,
- tomato – 1 piece,
- lemon juice - tablespoon,
- salt to taste.
Add salt to the fish fillet and brush with lemon juice. Peel the vegetables, pour boiling water over the tomatoes, remove the skins and cut into cubes. Place vegetable cubes in a baking dish or sleeve, and fillet on top of them. Simmer for 20 minutes at 180 degrees.
What symptoms differentiate between appendiceal colic and other types of acute appendicitis?
Regularly checked by doctors when acute appendicitis is suspected, the Shchetkin-Blumberg symptom gives a negative result. To identify this symptom, you need to slowly press with your hand on the abdominal wall of the lying patient, and then sharply remove your hand. Increasing pain indicates a positive symptom, absence of changes in the nature of pain indicates a negative one.
A “dubious symptom” is also possible - painful, but not sharp sensations that the patient experiences when removing his hand. In this case, a correct check is usually hampered by very tense abdominal muscles, bloating, ascites or a well-defined subcutaneous fat layer.
In case of appendicular colic, Karavaeva’s symptom will also be negative - the nature of the pain does not change when coughing. Sitkovsky's symptom is also not detected - if the patient lies on his left side, the pain will not appear and will not intensify if it is felt constantly. Retracting the abdomen or pressing the right femoral artery also does not change the picture.
Folk remedies

To prevent the occurrence of colic, medicinal herbal preparations are used. They include herbs with antispasmodic, calming effects that improve food digestion. For example, you can use the following formulas:
- St. John's wort, motherwort and chamomile flowers - 30 g each, calendula flowers - 10 g;
- fennel fruits, oregano herb and mint leaves in equal parts;
- cudweed grass, blueberry fruits - two parts each, lemon balm leaves, dill fruits - one part each (recommended if you are prone to diarrhea);
- flax seeds, senna leaves and chamomile flowers 20 g each, mint and lemon balm leaves 10 g each, rose hips 20 g (prescribed for constipation).
To prepare the infusion, pour a tablespoon of the mixture into 250 ml of boiling water overnight. In the morning, filter and take 50 ml before meals. The course of treatment lasts at least a month.
Symptoms of cramps in the intestines
Intestinal spasms are accompanied by a number of other symptoms:
- Heaviness in the stomach. In addition to spasms in the intestines, the patient feels heaviness in the stomach for no apparent reason. The appearance of this symptom occurs on an empty stomach and immediately after eating.
- Lack of appetite. The patient notices a lack of appetite. The body refuses to take food. Sometimes these symptoms are accompanied by nausea and vomiting.
- Gastrointestinal tract disorders. Stomach cramps often lead to gastrointestinal disorders. The patient begins to have problems with stool, frustration and constipation.
- Temperature increase. During the inflammatory process in the human body, the temperature rises. The patient's condition is characterized by weakness, lack of appetite and constant drowsiness.
- Headache. The patient suffers from headache, chills, and loss of strength. Migraines often begin.
- Flatulence. Flatulence is one of the main symptoms accompanying intestinal cramps. Flatulence continues for several days. Increases after eating.
Diagnostics
Taking an anamnesis for this condition is a very important point in diagnosis. The doctor will clarify the presence of chronic diseases of the digestive and genitourinary systems, find out the nature of nutrition, working conditions (important when in contact with chemicals). When examining, pay attention to the color of the skin, mucous membranes, and the patient’s posture.
On palpation of the abdomen, pain is usually not expressed, bloating is noted. During auscultation, increased intestinal sounds and rumbling are heard; their absence is an ominous sign and indicates intestinal obstruction.
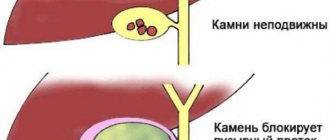
General and biochemical blood tests are prescribed to detect inflammation (increased levels of leukocytes and ESR), helminthic infestation (increased number of eosinophils), dysfunction of the liver and pancreas.
Instrumental methods include ultrasound and radiography with a contrast agent. In more complex cases - computed tomography and magnetic resonance imaging. Endoscopic research methods are also informative - gastroduodenoscopy, colonoscopy. To study the state of the biliary system and pancreas, cholangiopancreatography and excretory urography are indicated.