Acute cholecystitis should be treated immediately. How is treatment carried out for such a diagnosis as acute cholecystitis? Symptoms and diagnosis will help determine therapy. This pathology is the most dangerous form of the inflammatory process. The pathology is accompanied by pronounced symptoms. Can lead to very serious consequences. If not treated in a timely manner, the pathology can cause death.
Acute cholecystitis is very similar in symptoms to inflammation of the pancreas, appendicitis, inflammation of the bladder, and pyelonephritis.
History of the disease (Anamnesis morbis)
He considers himself sick for about 1 week, when suddenly, after an error in diet, dull, aching pain appeared in the right hypochondrium, the intensity of which increased, and over time, nausea, dry mouth, and general weakness appeared. She did not seek medical help. In the evening of 21.10. the pain intensified sharply, became constant, dry mouth and general weakness increased. Due to increased pain, she sought medical help at the OKB named after. Burdenko was hospitalized in the 2nd surgical department.
Treatment of cholecystitis
Treatment includes recommendations on the regimen, conservative therapy and, if indicated, surgical intervention. Self-medication, experiments with medications, medicinal herbs are dangerous!
Cholecystitis, the symptoms and treatment of which require hospitalization, is observed in the surgical department of the hospital. Treatment can be carried out at home, but only after consultation with a medical specialist.
The treatment regimen for acute cholecystitis includes:
- as prescribed by a doctor, hunger or a special diet (the diet of foods, their cooking, frequency of meals is specified);
- physical peace.
Conservative therapy is carried out as prescribed by a doctor in the following areas:
- pain relief (analgesics, antispasmodics);
- antibacterial therapy;
- choleretic drugs (after determining the cause of the disease);
- infusion, detoxification therapy (intravenous administration of solutions by drip method);
- antienzyme drugs (contrical, gordox);
- according to indications, hemostatic drugs;
- vitamins of various groups;
- therapy of concomitant diseases.
First aid for biliary colic
Biliary colic is a sign of acute cholecystitis. For diagnosis, consultation with a medical specialist is necessary. Cramping pain is characteristic of a number of diseases. Some of them, for example, myocardial infarction, require immediate hospitalization. To receive qualified advice, you must call an ambulance.
Taking painkillers and antispasmodics can make diagnosis difficult. Without information about the cause of the disease, you cannot take decoctions of medicinal herbs or wash your stomach. The patient must be placed in a position that causes less pain. Do not give water or food until the ambulance arrives.
Life History (Anamnesis Vitae)
Born in 1939 in the Penza region, Bashmakovsky district, Nikolaevka village. She grew and developed according to her age and gender.
Not working due to retirement.
Marital status: married, two children
Living conditions are satisfactory, food is sufficient and not rational, with a predominance of fatty foods. He does not abuse alcohol and does not smoke.
Denies tuberculosis, syphilis, Botkin's disease, HIV and other viral diseases.
Allergic reactions to medications and foods were not observed.
Drug therapy
Antispasmodics
This is a group of drugs that cause relaxation of smooth muscles, including the muscles of the gallbladder wall and bile ducts. Myotropic antispasmodics are prescribed for biliary dyskinesia of the hyperkinetic type.
An example is drugs based on the active substance drotoverine - “Doverin”, “Droverin”, “No-shpa”. The drug "Halidor" is an antispasmodic with a more pronounced vascular effect. Normally, bile from the bladder enters the bile duct, and from there into the duodenum.
The cause of difficulty in outflow may be a spasm of the sphincter of Oddi (the place where the bile duct enters the duodenum). An antispasmodic that is effective in this case is Duspatalin. The drug "Odeston" has a complex effect - it combines the properties of an antispasmodic and a choleretic drug.
Choleretic drugs
Choleretic agents perform two main functions: they stimulate the formation of bile and increase its outflow into the duodenum. Drugs to improve the flow of bile are divided into two groups.
- Cholekinetics increase the tone of the muscles of the bladder itself and expand the ducts through which bile flows. This group includes magnesium sulfate. Drugs in this group are prescribed for hypotonic dyskinesia (aching pain, feeling of heaviness in the right side).
- Cholespasmolytics (an effect similar to drotoverine) cause relaxation of the biliary tract. This group includes: “Atropine”, “Platifillin”, “Methacin”.
Treatment with antibiotics
In acute cases or exacerbation of a chronic process, broad-spectrum antibiotics are prescribed: semisynthetic penicillins, cephalosporins. Following the principles of rational antibiotic therapy, the doctor selects the drug based on the patient’s condition, his concomitant diseases, and age.
Self-medication with antibiotics leads to complications, immunosuppression, and the development of allergic reactions.
Use of traditional medicine methods
Traditional medicine methods for cholecystitis are based on the use of medicinal herbs. The active substances contained in them are as dangerous as drugs.
The choleretic effect can be indicated when the outflow from the gallbladder is preserved and is contraindicated in case of calculous cholecystitis or flexure of the cystic duct. Uncontrolled use of traditional medicine can lead to deterioration and the development of life-threatening conditions.
Objective examination of the patient
The general condition is of moderate severity, the position is active, consciousness is clear. Body temperature 36.80 C.
Height 170 cm. Weight 68 kg. The physique is normosthenic.
Skin color is normal, turgor is normal. Visible mucous membranes are of normal color, moist, the tongue is dry, covered with a white coating on the sides. The abdomen is enlarged due to subcutaneous fat. Lymph nodes are palpated as elastic formations 0.5 - 1.0 cm in size, not fused to each other and the underlying tissues. Muscle development is satisfactory, tone is normal, symmetrical. The function of the joints is preserved. Active and passive movements in all joints are fully preserved.
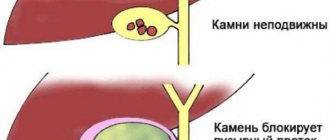
Etiology and pathogenesis
- damage to the walls of the bladder by solid formations (stones), blockage of the bile duct with stones (calculous cholecystitis);
- contamination of bile with bacterial flora, development of infection (bacterial cholecystitis);
- reflux of pancreatic enzymes into the gallbladder (enzymatic cholecystitis).
In all cases, the development of inflammation in the walls of the gallbladder causes a narrowing of the lumen of the bile duct (or its obstruction by a stone) and stagnation of bile, which gradually thickens.
Respiratory system
Breathing through the nose, free, rhythmic, respiratory rate 17 per minute. The voice is loud and clear. The shape of the chest is normosthenic, the intercostal spaces are moderate, the supra- and subclavian fossae are filled, the epigastric angle is straight, the chest is symmetrical. Mixed breathing type.
On palpation, the chest is painless and elastic. Voice tremors are the same in symmetrical areas of the chest.
When percussing over symmetrical areas of the chest, a clear pulmonary sound is heard.
Percussion boundaries of the lungs
| Upper border of the lungs | On right | Left |
| Front height of tops | 4 cm above the middle of the collarbone | 4 cm above the middle of the collarbone |
| Height of the tops at the back | At the level of the spinous process C VIII | At the level of the spinous process C VIII |
Width of Krenig margins 6 cm 6 cm
| Lower border of the lungs | On right | Left |
| Along the parasternal line | Upper edge of 7th rib | Not determined |
| Along the midclavicular line | 7th rib | Not determined |
| Along the anterior axillary line | 8 rib | 8 rib |
| Along the midaxillary line | 9th rib | 9th rib |
| Along the posterior axillary line | 10 rib | 10 rib |
| Along the scapular line | 11th rib | 11th rib |
| Along the paravertebral line | spinous process Th 12 | spinous process Th 12 |
On auscultation, vesicular breathing is heard in symmetrical areas of the chest, but there are no wheezes. Bronchophony is the same on both sides over symmetrical areas of the chest.
Circulatory organs
On examination, no swelling of the jugular veins is observed.
On palpation, the apical impulse is detected in the fifth intercostal space on the left, 1 cm outward of the midclavicular line; it is reinforced, limited, and resistant.
Percussion.
Limits of relative dullness of the heart
| Intercostal space | Relation to topographic line | |
| Right | 5th intercostal space | along the right edge of the sternum |
| Left | 5th intercostal space | 1 cm outward from the left midclavicular line |
| Upper | 3 rib | Midway between the parasternal and left midclavicular line |
The diameter of the relative dullness of the heart is 10 cm.
The width of the vascular bundle is 5 cm.
The heart configuration is normal.
Limits of absolute dullness of the heart
| Intercostal space | Relation to topographic line | |
| Right | 5th intercostal space | Along the left edge of the sternum |
| Left | 4th intercostal space | 1 cm to the right of the left midclavicular line |
| Upper | 3rd intercostal space | Midway between the parasternal and left midclavicular line |
On auscultation, contractions are rhythmic, heart rate is 84 beats per minute.
Heart sounds I and II are muffled and heard at all points of auscultation.
Laboratory and instrumental diagnostics
Purulent cholangitis, complicating the course of acute cholecystitis, can develop as a result of a direct transition of the inflammatory process from the gallbladder to the extrahepatic bile ducts. This is accompanied by thickening of their walls and narrowing of the lumen, which, in turn, leads to disruption of the outflow of bile into the intestines.
However, in most cases, purulent cholangitis occurs in the presence of stones in the bile ducts and stricture .
Obstructive cholangitis is the most severe due to persistent bile stasis and rapid spread of infection into the intrahepatic bile ducts. Purulent obstructive cholangitis can lead to cholangiogenic liver abscesses and biliary sepsis.
Clinical signs of purulent cholangitis do not appear immediately, but 3-4 days after the onset of the attack , and sometimes later. It is characterized by three clinical signs ( Charcot's triad ):
Increasing icteric discoloration of the skin and sclera,
high temperature up to 38-39°C, accompanied by chills and
· pain in the right hypochondrium.
The patient's condition is serious, consciousness may be confused; Tachycardia and a tendency to hypotension are noteworthy.
When palpating the abdomen, along with the symptoms of acute cholecystitis, an increase in the size of the liver and spleen can be detected.
A blood test reveals
high leukocytosis with a shift of the leukocyte formula to the left,
· sharp increase in ESR,
hyperbilirubinemia,
· as well as increased levels of transaminase, alkaline phosphatase, gamma-glutamyltransferase.
With the progressive course of purulent cholangitis, signs of hepatic-renal failure and DIC syndrome appear.
Purulent obstructive cholangitis, complicating the course of acute cholecystitis, is accompanied by high (up to 40%) mortality.
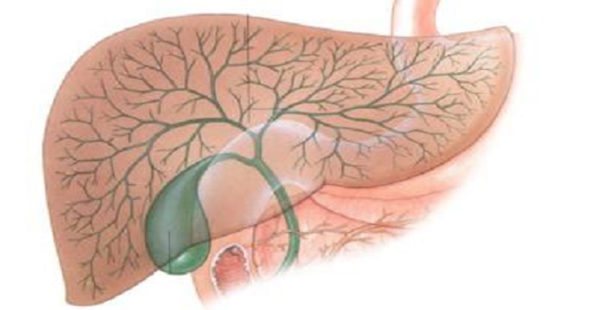
The purpose of diagnostic measures is not only to establish the fact of cholecystolithiasis and signs of inflammation of the gallbladder wall, but also to determine the form of inflammation of the gallbladder, which largely determines the urgency of surgical treatment, the duration of preoperative preparation, the possibility of a full-scale preoperative examination and the choice of an adequate method of surgical treatment.
The most important task of the preoperative examination of a patient with calculous cholecystitis is the diagnosis of changes in the extrahepatic bile ducts (in particular, choledocholithiasis).
Examination upon admission:
-complete blood count, urinalysis, urine amylase, RW, blood glucose, bilirubin, urea, creatinine, AST, ALT, amylase).
— Ultrasound of the abdominal organs (gallbladder, choledoacute cholecystitis, Wirsung duct).
- examination of related specialists : if a concomitant pathology is identified that requires correction, if the diagnosis is unclear, all patients over 45 years old - a therapist (ECG is mandatory).
1. Ultrasound examination of the organs of the hepatopancreatobiliary zone. Dynamic ultrasound.
In elderly and senile patients with a discrepancy between clinical manifestations and the degree of destructive changes in the wall of the gallbladder, ultrasound data allows timely identification of indications for surgery.
Ultrasound signs of acute cholecystitis are:
- thickening of the gallbladder walls more than 4 mm,
- “double contour” of the wall,
- increase in the size of the gallbladder,
- impacted stone at the mouth of the cystic duct,
- presence of perivesical fluid,
— positive ultrasound Murphy sign (local tension of the gallbladder under the ultrasound probe).
- direct and indirect signs of biliary hypertension (dilation of the intrahepatic bile ducts, increase in the diameter of the common hepatic and bile ducts).
Dynamic ultrasound is a repeated ultrasound examination against the background of a changing or stable clinical picture of the disease (thickening of the walls, an increase in the volume of the gallbladder, the appearance of paravesically located fluid in the abdominal cavity - signs of progression of the inflammatory process). Dynamic ultrasound allows you to monitor the course of the inflammatory process of the gallbladder and promptly carry out surgical intervention.
2. Laparoscopy is indicated for patients with an unclear clinical diagnosis. In acute cholecystitis, laparoscopy has a high resolution in the differential diagnosis of inflammatory diseases of the abdominal organs and tumor lesions. The diagnostic accuracy of the method is 94-97%. During laparoscopy, it is possible to puncture the gallbladder and perform direct cholecystocholangiography and apply a cholecystostomy. The use of laparoscopy is contraindicated in cases of extreme severity of the patient's condition, severe cardiac and pulmonary insufficiency, as well as in cases of suspected massive adhesions in the abdominal cavity.
3. ERCP (endoscopic retrograde cholangiopancreatography ) is the most informative method for diagnosing changes in the bile ducts, including choledocholithiasis, stenosis of the large duodenal papilla and extended strictures of the extrahepatic bile ducts.
In connection with the emergency situation, it is assumed that the optimal set of laboratory and instrumental methods will be used (Fig. 10.1), which must be carried out within 24 hours from the moment of hospitalization of the patient.
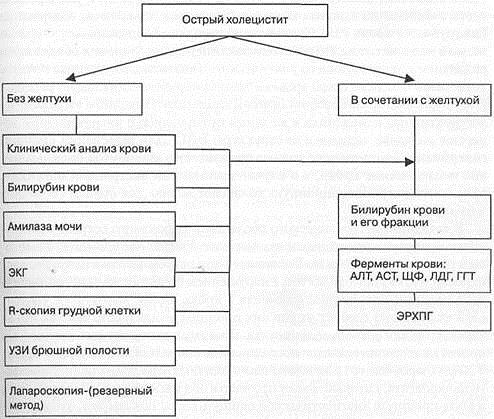
Rice . 10.1. Diagnostic algorithm for acute cholecystitis and its complications .
· When studying the composition of peripheral blood in patients with various forms of acute cholecystitis, significant changes are detected in the white blood .
An increase in the number of leukocytes with a shift in the formula to the left (due to band neutrophils) indicates a destructive process in the wall of the bladder. The more severe the inflammatory process in the gallbladder and abdominal cavity, the more pronounced these changes are.
However, in weakened and elderly , a clear pattern between the severity of changes in the gallbladder and the number of leukocytes in the blood may not be observed.
· Determining the level of bilirubin in the blood in patients with acute cholecystitis is a mandatory study, which makes it possible to identify cholestasis in the early stages of the disease.
A moderate increase in the content of bilirubin in the blood (25-40 µmol/l) is often found in patients with acute cholecystitis. Slight hyperbilirubinemia is explained by the development of concomitant toxic hepatitis with intrahepatic cholestasis. But even this level of hyperbilirubinemia should be considered as an alarming moment, indicating pronounced destructive changes in the gallbladder, or extrahepatic cholestasis due to lithiasis or the structure of the obstructive system. To determine the cause of hyperbilirubinemia, it is necessary to perform a detailed biochemical blood test, and in case of emergency surgery, use intraoperative cholangiography to assess the condition of the bile ducts.
· The standard diagnostic examination of a patient with acute cholecystitis includes the study of amylase in the urine .
· Moderate increase in amylase in urine to 128-256 units . According to Wolgemut, in acute cholecystitis it is often noted, which is probably due to dysfunction of the gastrointestinal tract and evasion of the enzyme into the blood.
· Its higher level ( 512 units and above ) requires clarification of the cause of amylasuria, since this is not typical for acute cholecystitis.
Therefore, in such cases, it is necessary to conduct additional studies (determination of blood amylase, ultrasound, laparoscopy) to exclude or confirm the presence of acute pancreatitis , which can occur under the guise of acute cholecystitis and cause a diagnostic error.
Experience shows that in acute pancreatitis, acute cholecystitis is most often mistakenly diagnosed.
· The list of mandatory studies for a patient with acute cholecystitis must include an ECG and chest x-ray .
The results of these studies are extremely important for a comprehensive assessment of the patient’s physical condition, excluding acute myocardial infarction and right-sided pleuropneumonia, which can imitate the symptoms of an acute abdomen and cause diagnostic errors.
· Ultrasound examination occupies a central place among special instrumental methods for diagnosing acute cholecystitis. The significance of ultrasound is determined by the high informativeness of the method for diseases of the pancreatohepatobiliary system, its non-invasive nature, the possibility of repeating the study many times and performing treatment procedures under its control.
The availability of the ultrasound method for many medical institutions and high diagnostic accuracy (98%) allow us to consider this study standard for acute cholecystitis . To avoid unforgivable diagnostic errors, ultrasound should be performed in all patients suspected of having this disease, without exception, regardless of the severity of clinical symptoms. Based on ultrasound signs, it is necessary to determine the morphological form of acute cholecystitis, since the choice of treatment tactics depends on this.
Vascular examination
Upon examination and palpation of the carotid, temporal, radial, popliteal arteries and arteries of the dorsum of the foot, their pulsation was revealed. When determining the arterial pulse on the radial arteries is the same, moderate filling, tension, normal speed, frequency - 84 beats per minute,
Blood pressure on the brachial arteries:
- on the right 130 and 85 mm. rt. Art.
- on the left 130 and 85 mm. rt. Art.
Urinary system
Urination is free.
No pathology was detected during examination.
The kidneys are not palpable in a horizontal position. There is no pain on palpation of the ureteral, costovertebral and costolumbar points.
The effleurage symptom is negative on both sides. Diuresis is normal.
Possible complications and prognosis of the disease
Acute cholecystitis can be complicated by conditions that are life-threatening for the patient.
Complications of acute cholecystitis:
- empyema of the gallbladder;
- paravesical abscess;
- obstructive jaundice;
- biliary colic;
- perforation of the bladder;
- transition of inflammation to neighboring organs: cholangitis, pancreatitis, ileitis, pleurisy;
- local or diffuse bile peritonitis;
- sepsis.
Chronic cholecystitis can be complicated by cholangitis, hepatitis, and pancreatitis. The course of a chronic disease is usually favorable. Compliance with dietary recommendations and timely treatment for exacerbations give good results.
The condition of the gallbladder, along with other organs of the gastrointestinal tract, determines the health of the entire body. Cholecystitis, the symptoms and treatment of which have been well studied by medical science, can be stopped before complications develop if you consult a doctor in a timely manner.
Author: elmiraritter
Surgical status
When examining the oral cavity, the mucous membranes are not changed, the tongue is dry, with a white coating on the sides. The condition of the teeth is satisfactory, the gums, soft and hard palate are unchanged.
The abdomen is enlarged due to the development of subcutaneous fat and is not involved in the act of breathing.
On palpation, the sensation is painful in the right hypochondrium, peristalsis is weakened, there are no signs of irritation of the peritoneum, a splashing noise is heard.
Symptoms of Shchetkin-Blumberg, Ortner, Mussi are negative.
The spleen cannot be detected on palpation.
Percussion
When percussing the abdominal cavity, a tympanic sound is heard.
Boundaries of the liver according to Kurlov:
Upper border: along the right midclavicular line - 6th rib on the right;
Lower border: along the right midclavicular line - 6 cm from the costal arch, along the anterior midline - 4 cm from the xiphoid process of the sternum, along the left costal arch - 3 cm at the level of the left parasternal line.
Auscultation
Intestinal peristalsis is heard. Peritoneal friction noise and vascular murmurs were not detected during the examination.
Causes of development of acute cholecystitis
The reasons may vary by gender, age, and initial condition of the patients.
Risk group:
- age from 30 to 50 years;
- male gender;
- eating habits, excess weight;
- physical inactivity;
- bacterial, fungal, viral, parasitic infections;
- diabetes mellitus, hypertension, atherosclerotic vascular disease;
- vasculitis (systemic lupus erythematosus);
- extensive injuries, including surgical interventions, organ and tissue transplantation;
- critical conditions (shock, sepsis, immunosuppression);
- long-term stay on artificial nutrition (drugs are administered through a vein).
The causes of acute cholecystitis are associated with the characteristics of neurohumoral regulation. Cholecystitis, the symptoms and treatment of which differ in women, can be caused by the following reasons.
Course of pregnancy:
- increased cholesterol levels, formation of gallstones;
- an increase in the size of the uterus, increased pressure in the abdominal cavity, compression of the gallbladder;
- changes in diet in early toxicosis, taste preferences, development of biliary dyskinesia.
Age-related risks are associated with the development of menopause, a tendency to physical inactivity, and the presence of chronic diseases.