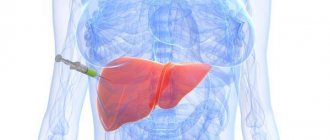
What a focal formation in the liver looks like on ultrasound
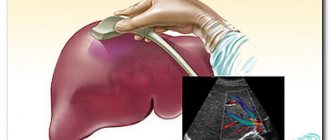
Focal liver damage is detected by ultrasound diagnostics. In a healthy person, the organ tissue is moderately hyperechoic, which is what the ultrasound diagnostician writes in the conclusion. If the structure is changed, the specialist sees hypoechoic formations in the liver on the monitor. Ultrasound allows you to analyze their density, size, and determine the presence of a capsule.
Hypervascular and hypovascular formation is an indicator of the number of blood vessels (there are many or few of them, respectively).
It can be benign in nature or formed from cancer cells - a biopsy followed by cytological examination helps differentiate them.
Non-parasitic cysts
A true cyst is a congenital disease, which is a cavity filled with fluid, occurs in 5-7% of people, more often in women, and is detected by chance during ultrasound. When a liver cyst is found, we must remember that it is combined with damage to the kidneys and pancreas. Accordingly, it is necessary to examine these organs. If a single congenital cyst is detected by chance and does not have clinical symptoms, then it should be monitored. In case of an increase in size during dynamic examinations, surgical treatment is indicated.
As a rule, true cysts accompany the following serious diseases:
- cholelithiasis;
- cirrhosis;
- tumors of the pancreas, gall bladder and ducts, colon, ovaries, uterus, retroperitoneum;
- stomach and duodenal ulcers;
- aneurysms of large vessels in the abdominal cavity.
A false cyst is called if it was a consequence of a previous injury, for example, a subcapsular rupture during an accident. These cysts fester and require surgical intervention.
What are the types of formations on the liver?
If a focal formation was detected during ultrasound diagnostics, you should not diagnose yourself and guess what it could be. It is better to listen to your doctor's advice.
Benign cysts include cysts of non-parasitic origin (single, multiple), as well as:
- nodular hyperplasia, hemangioma, adenoma, lipoma;
- hematomas of traumatic and postoperative origin.
Infectious foci are detected with abscess, echinococcosis, alveococcosis. Malignant formations are hepatocellular carcinoma, angioblastoma, hepatoblastoma.
Benign
Small lesions often do not make themselves felt. The altered areas are formed from epithelial tissue (adenoma), stromal tissue (nodular hyperplasia), blood vessels (hemangioma), and fat cells (lipoma).
Structural changes in the liver are detected by chance. It is possible to suspect their presence without instrumental examination. If the formation increases, pain occurs in the right lobe of the liver.
Hemangioma is characterized by a high level of vascularization (proliferation of the vascular network), that is, hypervascular. Cyst, adenoma, abscess are hypovascular formations of the liver. The approach to treating a benign structure is determined by its size, rate of increase and the danger of degeneration into a malignant form.
Adenoma and cystadenoma
Adenomas are formed from cells similar to normal liver cells. The lesions are single or multiple, located in groups, and have a capsule. Adenomas can progress rapidly, reaching a diameter of up to 20 cm. If intensive growth is observed, removal of the abnormal area is required.
Cystadenoma often occurs in women over 40 years of age. This is a single multi-chamber formation, the cavity of which is lined with cuboidal epithelial cells. Mucus accumulates inside the chambers, and papillomas may occur. Cystadenoma is prone to degeneration from a benign to a malignant form, so it must be removed immediately.
Hemangioma
The structure of the hemangioma is formed from venous elements. It grows slowly, does not metastasize, and does not spread to other organs. Regular monitoring of hemangioma is necessary due to the high risk of compression of the bile ducts and disruption of bile outflow, deterioration of blood supply to the liver when the vascular bed is blocked. Possible bleeding due to rupture of blood vessels. Transformation into cancer is rare.
Lipoma
Formed from fat cells. The diameter of a lipoma in the liver is rarely more than 5 cm. The risk of cancerous degeneration is low.
Liver hyperplasia
Hyperplasia is associated with a change in the lobulation of the organ. Pathology is often diagnosed in the right lobe of the liver. With the nodular form of hyperplasia, multiple nodules are found, the size of which is no more than 4 cm. The volume of the liver remains normal. Pathological areas grow slowly, do not spread to nearby organs, and respond well to treatment.
Cysts
The formations are congenital or occur against the background of inflammatory processes. Cysts have a capsule containing fluid inside. The color varies from transparent to brown-green (blood and bile are present). Multiple or single cysts are found both inside and on the surface of the liver. The size of the formations sometimes reaches 25 cm in diameter. Large ones are removed, small ones (up to 5 cm) are observed.
Hematoma
Occurs after injury or surgery for vascular damage. Ultrasound shows the accumulation of fluid and clots (during the formation of a cyst), a thick mass with a dense capsule, septa (a progressive cyst). Often the hematoma resolves on its own.
Infectious
Liver masses are often of infectious origin. An abscess occurs when pathogens invade the liver. Transmission of infection through blood, lymph or bile is possible when:
- cholecystitis, cholangitis;
- diverticulitis;
- duodenal ulcer;
- damage to the integrity of the intestine.

A person complains of pain on the right under the ribs and increasing weakness. Against the background of an abscess, fever and profuse sweating occur. With parasitic infestation (infection with echinococcus, alveococcus), cysts form. Echinococcosis formations do not appear for a long time. When the patient seeks help, the cyst may fill with a large volume of fluid (from 1.5 to 5 liters).
Multiple formations are formed during alveococcosis. The cysts are filled with thick white contents; when cut, they resemble cheese with holes. The diameter of the formation ranges from 1 to 30 cm. The cyst can grow beyond the liver and spread to nearby organs. Because of this, the pathology is called alveococcal cancer.
Malignant
A tumor in the liver may be malignant. It occurs directly in the tissues of the organ or is the result of the germination of metastases from other foci.
- Hepatocellular carcinoma develops very quickly and often causes death. Occurs mainly in men over 50 years of age.
- Angiosarcoma is also very aggressive in nature, occurring with equal frequency in women and men.
- Hepatoblastoma is diagnosed in children under one year of age. The formations look like nodes without a capsule.
Symptoms of a malignant tumor in the liver are yellowing of the skin and eyes, dark urine. A person quickly loses weight, feels weak, and has pain on the right side under the ribs.
Metastases
Metastases are usually called those malignant tumors that arise in various organs and tissues of the body under the influence of an existing primary tumor, both before and after the patient is cured.
Oncologists associate the occurrence of metastases with the spread of malignant cells detached from the tumor through the lymphatic and blood vessels.
In general terms, they imagine the causes and mechanism of metastases as follows.
When a tumor develops, a large number of dead and living malignant cells are rejected from it, which, with the flow of lymph, enter the first regional lymph node located nearby.
Along this path, in the tumor focus and in the regional lymph node, malignant cells come under the influence of antitumor immunity agents (cellular and humoral antibodies, etc.). As the tumor develops, at first this “primary” immunity is activated, and then gradually weakens.
As a result, the regional lymph node becomes “clogged” with cells and their “corpses”; the movement of lymph through the node is greatly reduced until it completely stops and even before metastasis occurs in it. In this case, the outflow of lymph occurs through collectors, newly formed pathways, or retrogradely, i.e. in the opposite direction. At the same time, antitumor immunity appeared in more distant lymph nodes and in peripheral blood lymphocytes.
Next, the malignant cells, passing through the lymphatic vessels and nodes, enter the blood vessels through the thoracic duct and are transported by the bloodstream to various organs and tissues. By settling in them, constantly dividing malignant cells can become the embryos of a new tumor.
This is how G.N. writes about it. Lobko and G.M. Porubova: “When tumor cells enter the circulatory or lymphatic system, they are exposed to a variety of factors: the mechanical action of flow and other numerical influences from the body’s antitumor defense system (cellular and humoral antibodies, complement, natural killer cells, free and fixed phagocytes, etc. ).
Tumor cells that have undergone this strict complex of selective influences and survive settle in distant organs, attach to endothelial cells, penetrate into the organ parenchyma and proliferate, giving rise to secondary neoplasms.
It should be noted that most scientists studying metastases respond to the relationship." the formation of metastases in certain organs or tissues with the intensity of the entry of malignant cells into the blood.” However ". the presence of malignant cells in the thoracic duct lymph and in the blood does not necessarily mean the development of metastases. When the body’s defense systems function effectively, tumor cells are fixed and destroyed outside the lymphatic system.”
And other researchers point out that “. at a high concentration of tumor cells in the blood, only a few of them give metastases. It has been shown that 24 hours after cells enter the blood, only 1% of them remain viable and only 0.1% exhibit the ability to metastasize (Fidler, 1970). Most of the tumor cells that enter the bloodstream or lymphatic channel die, so their presence in the blood of a tumor carrier does not mean that metastasis has begun.”
This leads to the conclusion that a cancer cell that has entered some organ or tissue cannot itself metastasize. Apparently, some other conditions are necessary for the occurrence of metastasis and even, perhaps, sufficient conditions without the introduction of malignant cells into the parenchyma of the organ. This largely confirms the fact that metastases have a latent period, i.e., as academician I.V. Davydovsky: “. the time of onset of metastasis varies enormously even for cancers of the same location.
For example, after removal of breast cancer, metastases can be detected clinically 10-20 years later.” It turns out that a cancer cell “settled” in an organ waits 10-20 years, and then can only begin its malignant work. This, of course, is incredible!
Indeed, the onset of metastases depends not on the malignant cell that has invaded the organ, but on injuries during surgical interventions: “Sometimes the latent period for the development of metastases after surgery is sharply shortened. It seems that the injury itself either causes abundant metastasis or accelerates the growth of previously occurring metastases. Apparently, mechanical factors in the form of, for example, diagnostic biopsies, can accelerate metastasis. The same is noted with complete excision of the primary node, which is confirmed experimentally (Roussi et al.).”
The problem of localization of metastases is of great interest to oncologists. Knowledge of the sites of possible metastasis for a given primary tumor would make it possible to timely detect metastasis and take measures for its treatment. However, many attempts to solve this problem have failed. And this is no coincidence. Another academician I.V. Davydovsky wrote: “There is a lot of mystery in the question of the localization of metastases and the selectivity of metastasis.”
Further diagnostics
Ultrasound scanning does not always allow one to accurately differentiate the type of tumor in the liver. Malignant lesions may not differ in echogenicity from healthy tissue. To clarify the diagnosis, other diagnostic procedures are required:
- computer, magnetic resonance imaging (shows the number, localization of formations, their size, shape, density and structure);
- biopsy followed by cytological examination (to determine the type of pathological cells).
You need to take tests - for tumor markers, blood biochemistry (liver tests). Consultation with a hepatologist or surgeon is required.
How are such problems diagnosed?
Unfortunately, benign tumor processes are diagnosed much less frequently than malignant ones, since such pathologies are most often asymptomatic, and patients do not consider it necessary to undergo preventive examinations.

Malignant formations can make themselves felt and therefore are detected more often.
The following diagnostic methods are most suitable for detecting any tumor-like lesions of the liver structures:
Mentioned ultrasound, CT or MRI; more accurate and specific methods of hepatoscintigraphy, hepatoangiography, laparoscopy with mandatory targeted liver tissue biopsy.
In addition, to detect malignant tumors, doctors may recommend liver tests and coagulation tests.
For such diseases, the occurrence of shifts in biochemical parameters is considered typical - a decrease in albumin, an increase in fibrinogen, an increase in transaminase activity, etc.
If metastatic lesions of the hepatic structures are suspected, patients may be prescribed studies of other organs - stomach radiography, mammography, colonoscopy, irrigoscopy, pulmonary radiography, endoscopy, and others.
Treatment of focal changes in the liver
The method of therapy is determined by the nature and size of liver changes and the patient’s condition. Specialists observe small benign formations during monthly ultrasound scans.

Large hyperechoic neoplasms that are not amenable to medication are removed. In the later stages of the pathological process, an organ transplant is required.
For liver cancer, radiation and chemotherapy are used. These methods are combined with surgical operations. Their volume depends on the degree of damage. At the 4th (terminal) stage, treatment is aimed at maintaining the function of the diseased organ and reducing the intensity of pain.
For formations in the liver, diet No. 5 is prescribed. Plant foods should predominate in the diet. Meat and sea fish - only low fat. Food is prepared by steaming, baking or boiling. Canned, smoked and fried foods are prohibited.
Benign tumors
A hyperechoic formation found during examination may be due to a benign tumor. These include:
- adenoma;
- hemangioma;
- nodes of non-cirrhotic nature.
Treatment tactics for benign tumors depend on the cause of their occurrence. For example, liver adenomas are more often formed in young women during long-term use of contraceptives; discontinuation of these drugs will lead to the resorption of adenomas. However, they can become malignant.
Hemangioma is a vascular tumor up to 4 cm in size, most often located in the posterior segments of the right lobe. Combined with the formation of hemangiomas in other organs and the spine. These diseases require dynamic monitoring. The danger of hemangiomas lies in the possibility of their rupture and bleeding. In addition, they mask malignant tumors and metastases.
Malignant neoplasms
Hepatocellular cancer in 100% of cases occurs as a result of cirrhosis due to hepatitis B.
Recently, the disease has become quite common due to the increased consumption of toxic substances in food, inhalation, and through the blood. It is characterized by diffuse nodular growth, an unfavorable course that ends in death.
Inflammatory diseases of the biliary tract, parasitic infestations, disruption of the production and outflow of bile lead to cholangiocarcinoma, another malignant disease with a poor prognosis.
It is not possible to clearly distinguish the primary tumor from metastases during primary diagnostics - ultrasound, SCT, MRI. The final diagnosis can be made by histological examination, which is performed after puncture or surgery. Tumors from almost all organs can metastasize to the liver:
- lungs;
- kidneys;
- transverse colon;
- stomach, ovaries;
- pancreas;
- breast;
- esophagus;
- ovaries;
- uterus;
- prostate;
- bladder.
The presence of metastases is a prognostically unfavorable symptom of cancer and indicates that the process is advanced.