Pain in the esophagus is most often a consequence of diseases of the gastrointestinal tract. Typically, severe and stinging pain occurs with gastroesophageal reflux disease. Pain in the esophagus area can be so severe that it is often confused with signs of a myocardial infarction.
In addition, unbearable pain in this area of the digestive tract can occur due to inflammation of the mucous membrane of the esophagus, as a result of a burn, or due to the formation of a malignant tumor - esophageal cancer. Let's consider the most likely cause-and-effect factors of pain symptoms in the esophagus and establish methods for diagnosing and treating various diseases of the esophagus.
Burning and pain in the esophagus
Possible causes and symptoms of pain in the esophagus
Painful discomfort in this segment of the gastric tract in various clinical pathologies is usually the same. Patients complain of discomfort in the sternum and upper chest. The causes of pain in the esophagus can be very different, ranging from mechanical damage to the digestive organ, damage to the organ by a systemic disease, or as a result of bacterial and fungal infections.
When the esophagus is burned, severe pain occurs in the epigastrium, as well as in the throat area. These symptoms are accompanied by vomiting and increased salivation. Painful symptoms, expressed by pain in the esophagus during or after swallowing, can occur with achalasia cardia. The disease is characterized by increased tension of the lower esophageal sphincter, which prevents the passage of food contents into the stomach. The terminal section of the esophagus becomes narrower, while the remaining segments of the esophageal canal become overstretched.
Narrowing of the esophagus is one of the causes of pain when swallowing
Some patients experience uncoordinated, severe spasms of the esophageal muscles, causing constant pain and discomfort. Another cause of pain in the esophagus can be reflux disease, or gastroesophageal reflux. In addition, one should not discount the side effect after taking medications that cause inflammation of the mucous walls of the esophagus with severe pain. A separate category are AIDS patients. Such patients are predisposed to developing eosinophilic esophagitis. Other symptoms caused by an infection of the esophagus include:
- difficulty swallowing;
- pain in the lower chest, projecting to the spine and back;
- nausea and even vomiting.
You should know that very severe pain and uncontrollable vomiting can provoke a rupture of the esophagus.
What is esophagospasm, classification
Spasm of the esophagus (esophagospasm) is a periodic disturbance of peristalsis of the esophagus, spastic contractions of its walls.
This pathology is divided into the following types:
- Diffuse spasm of the esophagus - “beaded esophagus” - is a motility disorder accompanied by uncoordinated spastic contractions of smooth muscles throughout the organ. The tone of the esophagus increases sharply, the lumen narrows. The spasmodic areas alternate with areas of muscles in normal tone and resemble a rosary.
- Segmental (acute) spasm - “nutcracker esophagus” - disorders that occur in limited areas, with a high amplitude of muscle contractions of the esophageal wall, 2 times higher than normal. Coordination of swallowing movements is not impaired.
Gastroesophageal reflux disease is the most common cause of esophageal pain
A very common cause of esophageal pain is reflux disease. In this condition, the acidic food contents are expelled from the stomach into the esophagus. Irritation of the mucous membrane occurs, which can be damaged and become the basis for the development of a tumor in the esophagus.
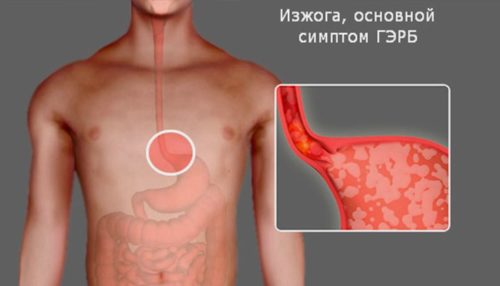
Heartburn is the main symptom of GERD.
Factors predisposing to the onset of the disease include:
- disrupting the work of the lower esophageal sphincter, whose task is to prevent the removal of food from the stomach;
- diseases that impair gastric motility, causing food retention - diabetes, systemic sclerosis, polyneuropathy;
- drugs that reduce the pressure of the lower esophageal sphincter - oral contraceptives, calcium channel blockers, beta2 mimetics);
- pregnancy;
- obesity.
Patients suffering from this disease most often complain of a burning sensation behind the sternum, persistent cough and refraction of the gastrointestinal tract, especially when lying down or bending forward, as well as after drinking alcohol. Alarming symptoms such as dysphagia, weight loss and gastrointestinal bleeding require urgent medical advice.
Symptoms of the disease
The disease is usually accompanied by three main symptoms:
- Pain. The main symptom, most often manifested in the lower third of the sternum. It occurs even in healthy people - during meals (as a result of hasty absorption of food), and at other times, sometimes even at night.
- Dysphagia. The patient perceives it as food retention inside the esophagus, a kind of feeling of a lump behind the sternum. Dysphagia often appears after eating solid foods and cold drinks, and stress or anxiety further intensifies the symptoms.
- Dyspeptic disorders in the form of periodic belching and heartburn, as well as the reverse movement of recently consumed food through the esophagus.
A mild form of the disease leads only to a temporary sensation of a food bolus and food retention - and then, mainly, while eating it. Within a few seconds it disappears, after which the patient can freely continue to eat, without much discomfort and further manifestations of esophagospasm. In severe stages of the disease, symptoms last much longer, as a result of which the patient may lose appetite, which over time leads to weight loss.
Esophageal cancer is the most dangerous cause of esophageal pain
Pain indicates a harmful process in the esophageal segment. Paradoxically, pain symptoms perform a useful function, as they indicate the onset of the disease and allow us to determine its location.

Esophageal cancer may cause pain when swallowing
Unfortunately, in the case of esophageal cancer, pain in the esophagus appears only at a very advanced stage.
Esophageal cancer may primarily be the cause of pain in men after 45 years of age.
Symptoms are not typical:
- There is difficulty swallowing food, first solid and then liquid.
- Hoarseness, dry cough, and frequent shortness of breath may occur.
- Patients often report pain in the heart.
The patient's complaints are associated with significant penetration of the tumor into the respiratory and cardiovascular systems. The prognosis for recovery with late diagnosis is disappointing. The survival time of diagnosed patients is several months. Therefore, it is very important not to ignore even the slightest signs of abnormal changes in the esophagus.
First aid for spasms
To alleviate the condition at home, it is recommended to take a few sips of warm milk. This will push the food through. Breathing exercises also help. Take a deep breath, hold your breath for a few seconds and exhale.
You can take a nitroglycerin tablet. However, you need to monitor your blood pressure.
After eliminating the attack, you need to seek medical help as soon as possible to identify the cause of the illness.
Diagnostic tests for esophageal pain
Numerous additional tests are helpful in diagnosing esophageal pain. Three main research methods are used as a standard:
- X-ray of the esophagus after administration of a contrast agent.
- Endoscopic examination.
- Esophagomanometry of the esophagus.
An X-ray contrast agent allows you to visualize narrowing or stretching of the esophagus, the presence of a tumor in the esophagus or diverticulum, or simply scan the esophageal passage. During an endoscopic examination, changes located inside the wall of the esophagus can be detected, and above all, a developing tumor can be identified.

How is esophageal manometry done?
During endoscopy, biomaterial is collected from the walls of the mucous membrane for histopathological examination. In turn, esophageal manometry measures the muscle tone of the organ of the digestive system. It is useful in diagnosing achalasia and esophageal spasticity. When diagnosing gastroesophageal reflux disease (GERD), a 24-hour pH measurement and the so-called esophageal impedance are prescribed, which provides information about the volume and type of contents, gas or liquid in the cavity environment. In addition, if cancer is suspected and severity is assessed, ultrasound, CT and MRI of the esophagus are prescribed.
Causes of pathology
Physiological causes of the disease may be developmental disorders that arise before the birth of the fetus. Congenital malformations of the esophagus occur during embryonic development and subsequently lead to various changes in the structure of its walls. The physiological causes of achalasia are divided into external and internal.
Internal factors include:
- neoplasms;
- esophageal injuries;
- toxic effects of smoking and alcohol;
- prolonged spasms of the cardia.
The same reasons include stenosis of the esophagus, caused by its damage due to infectious diseases.
External factors mean contributing influence from other organs and systems. These factors include the following diseases:
- sclerosis of the esophagus with adhesions;
- hepato- and splenomegaly;
- gastritis;
- peritonitis;
- aerophagia;
- gastroptosis;
- mediastinitis;
- aortic aneurysm;
- aortitis;
- pleurisy.
Contributing factors that can cause dilation of the esophageal tube are neurotrophic disorders and endocrine dysfunction. In addition, it is possible that allergies cause changes in the functioning of the neuromuscular apparatus of the esophagus.
Diseases that cause similar symptoms
Post-infarction pain is not always associated with esophageal disease, however, the pain symptoms are very similar. The source of pain can also be all anatomical structures located in the abdominal cavity, with the exception of the lung parenchyma. Any inflammation in the abdominal cavity can cause pain that the patient will find in the chest. Naturally, the diagnosis presupposes the presence of symptoms. During exercise or emotional stress, patients suffering from coronary artery disease will also hold their chest in an attempt to relieve symptomatic chest pain. A person may experience similar symptoms with the aforementioned myocardial infarction.

Fatty foods can cause pain in the esophagus
Pain that occurs after eating a rich, fatty meal is likely caused by the presence of gallstones in the gallbladder. In addition, stomach ulcers can cause similar symptoms. We should also not forget about neurotic pain caused by inflammation of tendon joints, as well as injuries to the musculoskeletal system. Take care of yourself and always be healthy!
Why does spasm of the esophagus occur with osteochondrosis?
There are primary and secondary forms of the disease. In the first case, the functioning of nerve endings is disrupted. The second appears with concomitant diseases. Spasm of the esophagus in osteochondrosis is called “vertebrogenic esophagospasm.” It develops reflexively when a nerve root is pinched.
The spinal cord innervates all internal organs. Autonomic nerves control their functioning. The symptoms can be confused with a number of other diseases. Only a specialist can determine the true cause of the appearance.
Varieties
There are several classifications of esophageal spasm. The most common division is the following:
- diffuse esophagospasm . In this case, the cause is uncontrolled contraction of the upper zone of the esophageal tube. If the esophagus is normal, then muscle contractions in all parts of the organ are synchronous. With the diffuse type, spasm occurs at any time (regardless of food intake);
- "Nutcracker esophagus" . Psychogenic esophagospasm of this form is diagnosed if the amplitude of muscle contractions of the organ is doubled;
- non-specific type . In this case, the spasms that are characteristic of the two previous forms are combined.
There are two more types of esophagospasm:
- primary or idiopathic . The reason for its progression is a deficiency of nitric oxide. This is what leads to a malfunction of the intermuscular nerve plexus, which is responsible for the normal functioning of the esophageal tube;
- secondary or reflex . Reflex contractions of the walls occur with hypersensitivity of the mucous membrane, which develops as a result of various pathologies of the digestive tract. This form of esophagitis is most often diagnosed in patients.
Stomach neurosis: psychological causes, signs, treatment
Gastric neurosis (irritable bowel syndrome, intestinal neurosis, esophageal neurosis) is a psychosomatic disease. In a fast-paced life, it is becoming more common, especially among people over 35 years of age. Every fourth person has experienced irritable bowel syndrome.
The essence of the problem
Gastric neurosis is a functional disorder of the gastrointestinal tract. This is the body's complex response to stress. Manifestations of neurosis intensify with a new psychological shock and are combined with mood swings.
Neurosis of the stomach reviews:
- “The psychotherapist prescribed pills, and after two days I noticed an improvement. Before that, I went to doctors for six months. I suffered just as much from pain,” Maria.
- “They prescribed the easiest sedative – valerian. Everything has passed,” Olga.
- “The psychiatrist told me that long-term stress is to blame. Constant tension and contraction of muscles causes digestive disorders over time,” Lyubov.
- “My neurosis is combined with panic attacks and vegetative-vascular dystonia. I was treated by a gastroenterologist for a year. Now they sent me to a psychotherapist,” Anna.
Analysis of reviews shows that the problem is very common. You can go to doctors for years, but without consulting a psychotherapist, neurosis cannot be cured.
Signs
Stomach neurosis symptoms:
- pain under the ribs, in the stomach, of unknown location;
- burning in the epigastric area;
- feeling of heaviness or chronic hunger, emptiness;
- bloating;
- white coating on the tongue;
- inability to taste and smell food, nausea, vomiting;
- changes in heart rhythm, chest pain, increased breathing;
- cephalgia;
- problems falling asleep and waking up, insomnia;
- heartburn independent of food consumed;
- loud belching of empty air;
- irritation, aggression, fears.
Over time, psychological manifestations expand. The patient is afraid that stomach problems will be found in the wrong place. Because of this, a person tries to leave the house as little as possible. The higher the anxiety and fears, the greater the risk of panic attacks.
It's not just the stomach that suffers due to stress. Functional disorders affect the entire gastrointestinal tract. The esophagus and intestines are often affected. These problems have their manifestations.
Violation Signs
| Esophageal neurosis | Heartburn, pain between the shoulder blades, increased sensitivity to hot, cold, spicy foods. In addition, there are problems with swallowing, a feeling of a lump in the throat, involuntary spasms that impede the passage of food or cause a gag reflex. |
| Intestinal neurosis | Diarrhea or constipation, simultaneous manifestation of diarrhea and constipation, cramping pain in the navel area, rumbling, feeling of fullness in the abdomen, night nausea, morning exacerbation of pain. |
Causes
Stomach neurosis occurs for a number of reasons.
- Poor nutrition, snacking on the go, lack of a meal plan, abuse of processed foods and fast food.
- Gastritis, ulcers, pancreatitis, cholecystitis, other inflammatory processes in the stomach.
- Stress, overwork, anxiety. At times of stress, the body's systems work to the limit, metabolic processes accelerate, and muscle tone increases. The stomach and other organs of the digestive system are no exception: muscles contract more often and spasms occur.
- Intoxication as a result of direct or indirect exposure to harmful substances: ingestion of spoiled foods, drinking alcohol, inhaling harmful emissions.
Treatment
Treatment is carried out in two directions: psychological counseling, medical treatment of symptoms. One without the other will be ineffective.
Neurosis of the stomach treated with psychotherapy.
- Identifying the causes of internal tension, identifying stress factors in the patient’s life.
- Increasing stress resistance by correcting self-esteem and self-confidence.
- Formation of the ability to overcome difficult life situations. The psychologist teaches the client to see opportunities for personal growth and life improvement in difficulties.
- Drawing up a rehabilitation plan to change the patient’s life.
There are many psychological causes of stress:
- job dissatisfaction;
- unprocessed psychological trauma;
- non-acceptance of oneself;
- fear of loneliness;
- the passing of a loved one;
- guilt;
- old grudge;
- insecurity;
- physical, intellectual, emotional exhaustion;
- fear of responsibility, etc.
The psychologist and the patient jointly find the true cause and develop a work plan. This situation requires a private approach. As psychological problems are eliminated, somatic signs of irritable bowel go away on their own.
Neurosis of the stomach: drug treatment.
- Complete diagnosis of the gastrointestinal tract to determine or exclude primary diseases such as gastritis, ulcers, polyps.
- When a disease is detected, appropriate treatment is prescribed. It depends on the diagnosis.
- If no organic lesions are found, then only a psychotherapist will deal with the patient.
- To relieve symptoms and alleviate the condition, the patient is prescribed painkillers and antispasmodics.
- The psychotherapist prescribes sedatives. The recipe depends on the severity of neurosis.
Treatment is complemented by diet and physiotherapy. The diet is selected strictly individually, but alcohol, smoking, and fatty foods are necessarily excluded.
Some useful physical treatments include massage, relaxing warm baths with sea salt and aromatic oils. Any activity is useful, even simple walking. When playing sports, endorphins are produced. They stop the production of the stress hormone cortisol.
Bottom line
It is better to prevent any problem. Psychological stress always affects the stomach first.
Try to do what you enjoy. Learn to throw out negative emotions, for example, beat a pear or dance. Increase your stress resistance, believe in yourself, take care of yourself.
: how to treat stomach neurosis
You may also like
Source: https://stressamnet.ru/nevrozy/nevroz-zheludka/
Treatment
Treatment methods depend on the stage of the disease: in the initial period, conservative treatment will be effective; advanced cardiospasm requires surgical intervention.
Conservative methods
Non-operative therapy includes general strengthening measures, organization of a diet, and drug treatment.
Psychotherapy
Patients must be convinced that their illness can be cured, comfortable nutritional conditions must be created, and the consequences of the nervous shock that caused the disease must be removed. Methods of suggestion and hypnosis will help restore emotional and mental health. Excessive physical activity and nervous tension are contraindicated.
Diet therapy
For spastic pathologies of the esophagus, small, frequent meals are necessary (4-5 times a day). It is served pureed and should be consumed slowly, chewing each portion thoroughly before sipping. Diets No. 1, 1a, 1b are recommended. It is necessary to exclude sour, spicy foods, dishes that provoke dysphagia.
There are rules to facilitate the passage of food into the stomach:
- after eating you need to drink a glass of liquid in one gulp;
- After eating, you need to strongly bend your chest and neck back, this helps straighten the esophagus and increase pressure on the cardiac valve. Dinner should be no later than 3-4 hours before bedtime, otherwise food will linger for a long time in the upper gastrointestinal tract and begin to ferment and decompose in it.

Medications
Medications for cardiospasm include drugs with various therapeutic effects:
- antispasmodics (Nitroglycerin, Amylnitrite) are taken before meals, which facilitates the passage of food into the stomach. Relaxation of the cardiac sphincter is facilitated by Papaverine, No-shpa, and belladonna preparations;
Important! Taking antispasmodics is justified in the initial period of the disease; in the later stages they inhibit esophageal peristalsis and can completely stop the movement of food.
- calcium antagonists (Nifedipine, Verapamil) relieve attacks of dysphagia;
- antacids (Maalox, Phosphalugel) are indicated for gastritis with high acidity, which provokes spasms of the esophagus;
- Atropine relieves gastrointestinal spasms well, but has an undesirable side effect on the central nervous system: it depresses consciousness, causes anxiety or drowsiness;
- enhanced vitamin therapy is necessary in advanced stages of the disease; to improve well-being, take B vitamins, which strengthen the nervous system.