Causes
Frequent, predominantly false urges to go out of nature are called “tenesmus.” Typically, such problems in the body’s functioning cause a lot of unpleasant sensations associated with concern for one’s health. For what reasons does tenesmus most often occur?
- A frequent desire to visit the restroom may occur due to the development of a benign or malignant tumor.
- The progress of hemorrhoids turns around
constant urges. - The problem may be a reaction to chronic diseases such as pancreatitis and ulcers.
- The appearance of fistulas, polyps and other neoplasms in the digestive system stimulates frequent bowel movements.
- This symptom may also indicate a disruption of the normal intestinal microflora.
In adults and children, frequent urges can be associated with elementary constipation: unable to remove feces from their body, a person every now and then feels the desire to try again.
False urges often indicate the development of inflammatory processes in the body or elementary signs of poisoning. Poor quality water or food that has expired can have such an impact on the gastrointestinal tract that the urge will accompany a person almost every minute.
Sometimes a problem occurs
as a reaction to a more serious illness. For example, malignant tumors, ulcers and pancreatitis are accompanied by this unpleasant symptom. It is impossible to make a diagnosis on your own, since you need to see the whole picture. That is why only a thorough examination will help to find out the cause of the problems that have arisen in the body.
Diagnostics
If you have frequent false urges to have a bowel movement, especially if they are accompanied by discharge of blood, pus and mucus, you should rush to a proctologist for examination.
Methods used to determine the causes of tenesmus:
- coprogram - fecal occult blood test;
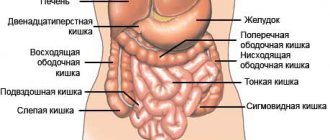
- sigmoidoscopy (examination of the rectum and sigmoid colon using an optical tube - rectoscope), makes it possible to determine the presence of internal hemorrhoids and assess the condition of the mucous membrane of this segment of the colon;
- irrigoscopy - radiography using a contrast agent to identify defects in the mucous membrane of the large intestine (now rarely used);
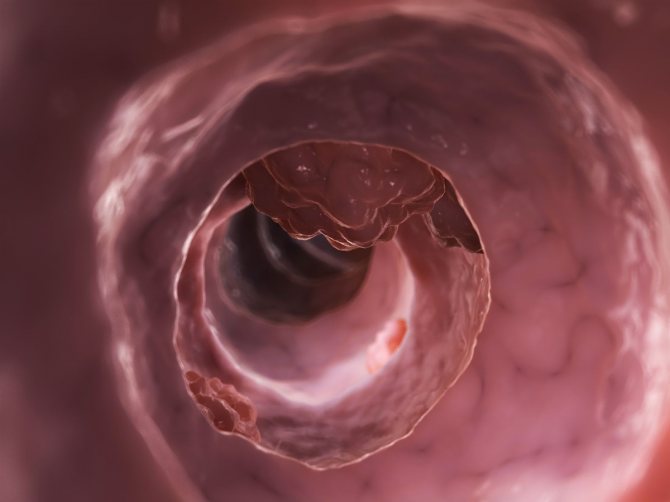
- colonoscopy - a detailed examination of the colon using a fiber optic probe with the ability to take tissue samples, providing information about the presence of benign and malignant neoplasms, diverticula, ulcers, etc. in the colon.
Constant urge to defecate
With diarrhea or an intestinal infection, the urge occurs suddenly and continues to bother the person for 2-3 days. However, there are cases when the urge to defecate does not disappear over time. A person may suffer from unpleasant sensations for a week, or even a month.
The most common cause is irritation and inflammation in the rectum. It occurs due to an incorrectly administered enema or frequent practice of anal sex. Abuse of laxatives, the presence of inflamed hemorrhoids - all this can cause regular urges that cannot be controlled. It is not difficult to notice the progress of the problem, because it is usually accompanied by the following symptoms:

- involuntary bowel movement;
- severe pain in the anal area;
- the appearance of blood and mucus in the stool.
The last sign is especially dangerous, because it indicates an extreme stage of development of the problem. If the frequent urge to defecate due to advanced hemorrhoids or a serious intestinal infection does not stop, a person may in the future face global complications that will have to be eliminated surgically.
Characteristics of false urges
Characteristic signs of involuntary contractions of the muscular structure of the intestine manifest themselves in attacks of sharp pain in the abdominal area, having cramping properties. The urge to defecate does not provide relief; a small amount of feces with blood and mucous impurities may be released.
Among women
The occurrence of tenesmus in the female half of the population is often a consequence of gynecological diseases. The anatomical structure of the female body is conducive to the rapid spread of inflammation to segments of the large intestine, which causes a failure of reflexes in the intestinal nervous system.
Women often complain of an imaginary urge to have a bowel movement in the first trimester of pregnancy, which is associated with hormonal changes in the body. In the later stages, constipation often occurs due to the pressure of the uterus on the intestinal walls. The next monthly cycle can also cause a similar problem due to an increase in hormonal levels. Additionally, attacks of mild nausea with possible vomiting occur.
Men
Pathologies in the male reproductive system can also lead to an increase in futile trips to the toilet. An increase in the size of the prostate gland due to prostate adenoma increases pressure on the intestinal walls, which provokes disturbances in the nervous reactions of the muscular structure of the intestine. Hyperplasia of the gland can also cause a false urge to urinate, due to the narrowing of the lumen of the urethra.
During certain surgical operations on the prostate gland, the integrity of the intestinal walls is disrupted and, as a result, disruptions in the nervous regulation of muscle contractions occur. The desire to go to the toilet is accompanied by signs of flatulence and rumbling in the stomach.
Children
The appearance of symptoms of tenesmus in a child usually indicates pathologies of the lower intestinal tract. The uncomfortable state is accompanied by noticeable pain, the presence of mucous and blood impurities in the stool. When going to the toilet, the baby may scream loudly, and he may experience redness of the facial skin from strong efforts during bowel movements. Fluctuations in temperature and manifestations of general weakness are possible. The abdominal area upon palpation is dense and enlarged, which indicates a disruption in the processes of emptying and the development of flatulence.
Doctors' advice
Having told the doctor that bowel movements are irregular, a person usually expects to receive a list of medications for treatment. However, the easiest way to eliminate the problem is with a competent and balanced diet. What is the diet for frequent urges?
- Fatty and spicy foods are removed from the diet.
- You will have to avoid pickled foods, as well as fast food.
- Experts recommend

eat more vegetables and fruits, as they can prevent the development of constipation. - You cannot ignore your drinking regime: during each meal you need to drink 300–400 ml of water.
- You will also have to give up dairy products, giving preference to cereals, soups and salads.
Doctors recommend eating in portions, eating no more than 200–300 grams of any food at a time. Otherwise, the urge to defecate will not disappear, continuing to terrorize the patient. If you are prone to constipation, you should include dried fruits and legumes in your diet.
As for medications, doctors do not always prescribe them. Typically, specialists turn to antibacterial and antiviral drugs, but here everything is individual and depends on the diagnosis. A person with an intestinal infection will not be able to take the same pills as a patient with a stomach ulcer.
If severe pain and spasms occur, you need to drink No-Shpu or Papaverine. It is believed that these drugs most effectively eliminate pain, without having a negative effect on the functioning of the entire body.
Your doctor may also advise

cold sitz baths that will soothe the smooth muscles of the rectum. If all the methods prescribed by a specialist turn out to be ineffective, you can always turn to folk remedies.
Two problems nearby: hemorrhoids and prostatitis - we treat them together
The frequent connection between prostatitis and hemorrhoids has been confirmed by medical practice and is a fact. The manifestation of one of these diseases provokes the appearance of another.
In the male body, the organs in which these diseases usually occur are located nearby, and their work is interconnected. Naturally, the incorrect operation of one of them entails problems in another organ located nearby.
If a patient is diagnosed with hemorrhoids, neighboring organs are checked for possible abnormalities in their functioning, since both diseases require therapy at the same time.
Causes of diseases
Both diseases are an inflammatory process that occurs in the pelvis. Since the organs in it are closely located, the pathogenic process occurring in any of them negatively affects the surrounding tissues and systems.
With such a close connection, the causes of both diseases are almost identical. And also one of these related diseases becomes the cause of another. Thus, the development of hemorrhoids negatively affects the prostate and leads to the onset of prostatitis.
Hemorrhoids and prostatitis develop simultaneously or separately in men:
- having a sedentary profession: cashier, programmer, driver;
- those suffering from constipation or diarrhea, causing blood stagnation in the circulatory system of the pelvis;
- survivors of severe psycho-emotional stress: suppression of androgen production and overflow of the pelvic vessels with blood;
- regularly freezing entirely or locally in the pelvic area;
- those who neglect proper nutrition: too much meat and lack of vegetables and fruits;
- those who do not follow a healthy lifestyle: bad habits, alcohol and drug addiction;
- leading an irregular, promiscuous or unconventional sex life: threat of infections, damage to the anus and mucous membrane;
- characterized by an excess of male hormones.
Disease connection
Difficulty urinating can occur with hemorrhoids and constipation.
To distinguish hemorrhoids from other diseases, you need to know the symptoms of the disease, monitor the condition of the body and undergo regular examinations with a doctor.
If you independently detect one of these diseases, you need to undergo a comprehensive examination of the pelvic organs and diagnose all systems and processes occurring in this part of the body. In a small percentage of patients, prostatitis and hemorrhoids appear together and occur with the simultaneous appearance of symptoms of both diseases.
So, with constipation and the development of hemorrhoids, urination becomes difficult. Most patients are first diagnosed with one of these diseases, and then, during treatment, the presence of the second is discovered.
The main reason for the development of hemorrhoids with prostatitis or prostatitis with hemorrhoids is considered to be untimely detection of both diseases and an incorrect approach to their treatment.
The effect of hemorrhoids on the prostate
With the development of internal hemorrhoids, formations in the anus are located in close proximity to the prostate. When the disease is advanced and the hemorrhoids become large, they block the proper supply to the nearby prostate gland. Tissues in a poorly supplied organ begin to atrophy and function incorrectly.
With this development of diseases, stagnation of urine in the bladder and difficulty urinating are possible. The inflammatory process, provoked by the penetration of pathogenic organisms into the rectal opening, can affect the functioning of the prostate and provoke prostatitis.
A frequent onset of infection is considered to be invasion of Escherichia coli, which, multiplying in the anus, infects the urethra.
The effect of prostatitis on hemorrhoids
With inflammation of the prostate in men, libido weakens, which leads to a decrease in the tone of the pelvic floor muscles due to rare sexual intercourse.
When prostatitis forms, the prostate enlarges and changes structurally, which entails weakening of the ligaments and muscles of the rectum.
Weakened muscles and ligamentous tissue can no longer perform their functions correctly, which is why hemorrhoids appear. With the inflammatory process in the prostate gland, male attraction to the opposite sex decreases, and sexual intercourse becomes rare.
Because of this, regular muscle training in this area does not occur, which provokes hemorrhoids.
Joint treatment
Stages of treatmentDescription
| Relief of acute inflammation and pain syndrome | Stage aimed at rapid relief, for prescribing further health measures |
| Establishing blood flow in the pelvis | Carried out to speed up regenerative processes and prevent relapses |
| Normalization of intestinal function | Relieves pain and additional bowel irritation during bowel movements |
| Strengthening the walls of the circulatory system and tissue regeneration | Prevents the recurrence of both diseases and accelerates the healing of internal tissues. |
Medicines against prostatitis and hemorrhoids
Most often, after an examination and diagnosis, the doctor prescribes the use of suppositories for hemorrhoids and prostatitis. This combination medicine treats both diseases and relieves the patient from painful bowel movements.
As well as drugs prescribed for hemorrhoids and prostatitis, they stop the inflammatory process and improve regeneration. They act as angioprotectors. Of the active ingredients, doctors prescribe the use of methyluracil or ichthyol rectal suppositories.
The pharmacy sells “Prostopin”, “Anestezol”, “Voltaren”, “Betiol”. To stop inflammation and help regeneration, use suppositories with propolis.
Diet for hemorrhoids combined with prostatitis
For more successful treatment, you need to reduce the amount of salt consumed.
To help medications do their job, you need to properly adjust your diet and fluid intake. It is recommended to drink more than 2 liters of water per day.
To achieve the desired effect, you will have to eat small portions 5-6 times a day. The diet menu for constipation is based on the maximum amount of fiber and the minimum allowable amount of protein food. It is recommended to reduce the amount of salty foods and salt in general, hot seasonings and spices.
Elimination of all unhealthy addictions is mandatory.
Massage, physical therapy procedures
Carrying out additional procedures in combination with the main treatment helps heal and speeds up recovery. For prostatitis, a course of prostate massage effectively speeds up the healing process. Due to the structural features of hemorrhoidal cones, it is impossible to massage the prostate with hemorrhoids.
It turns into a dangerous event that can cause bleeding or infection. Moderate physical activity is recommended to maintain muscles and connective tissues in good shape. Physical education or gymnastics improves blood flow in the pelvis, which speeds up the process of regeneration and recovery.
The list of permitted procedures begins with walking with long steps (without overexertion), bending the body to the sides and turning the body in a circular motion, standing with legs wide apart. You can strengthen the muscles of the hip region with the help of a “bicycle” and a “bridge”.
Retracting your abdominal muscles will help.
Source: //EtoGemor.ru/gem/vazhno/gemorroj-i-prostatit.html
Traditional medicine in the fight against frequent urges
If a person goes to the toilet in small portions, and bowel movements are not complete all the time, you can turn to recipes from grandma’s chests. Thus, fans of traditional medicine advise using the following techniques:
- administering enemas with a weak solution of potassium permanganate;
- cool baths with chamomile infusion;
- You can also take a decoction of watermelon rinds: to do this, 100 grams of dried rinds must be boiled in a liter of water, after which the liquid must be filtered and taken orally cold;
- Bran, which can be brewed with a glass of milk or water, is an excellent remedy for constipation;
- Goat milk also has similar properties, which must be taken daily for breakfast for 30 days.
It is impossible to give yourself completely to the power of traditional medicine, since instead of bowel movements, a person may only experience a deterioration in general well-being. Such techniques are advisable only after a final diagnosis has been made. It is important to know what exactly the patient is being treated for, and only then move on to home procedures.
If severe pain does not leave a person even with intensive treatment, he should try taking soothing baths with chamomile infusion. It is believed that chamomile eliminates even the most serious pain and temporarily relieves unpleasant spasms.
There are some processes going on in the rectum all the time, and sometimes a person has to deal with constipation or, conversely, too frequent urges to go to the toilet. It is useless to fight this until the source of the problem is identified and completely eliminated.
Treatment
Treatment in most cases is conservative - medications and diet are selected.
The pharmacological part of treatment may be based on the following drugs:
- antispasmodics;
- mild laxatives;
- painkillers, but only if necessary;
- antibiotics;
- drugs to improve blood circulation in the pelvic organs;
- rectal suppositories.
The diet is based on a gentle diet - spicy, fatty, floury foods should be excluded. Food should be liquid or puree, high in calories. It is important to maintain an optimal drinking regime - at least two liters of water per day.
In this case, folk remedies are not excluded, but they can be used only as prescribed by a doctor, used as additional, and not primary methods of therapy. To eliminate the unpleasant symptom, you can do sitz baths based on chamomile, calendula, and sage.
In most cases, the prognosis is favorable. As a rule, normalizing your diet, taking medications prescribed by your doctor and maintaining a healthy lifestyle are enough to eliminate intestinal tenesmus.
Treatment
The main therapy for tenesmus or false urge to defecate is to eliminate the cause that caused the symptom.
The main directions for correcting the condition include:
- diet therapy;
- drug improvement of food digestion;
- normalization of peristalsis;
- restoring the balance of intestinal microflora.
In the presence of surgical pathology (peptic ulcer, polyposis, hemorrhoids, anal fissures, mucous membrane prolapse, etc.), surgical intervention is performed if necessary. It is important to normalize the emotional background and hormonal disorders, if any.
Diet therapy
A diet is recommended that facilitates the digestion and passage of food through the gastrointestinal tract. The main postulates during treatment should be:
- normalization of diet: eat meals in small portions at the same time, at least 5 times a day;
- the diet is dominated by plant products that help stimulate peristalsis and normalize microflora due to the fiber they contain;
- exclude foods that contribute to increased gas formation (cabbage, legumes);
- food must be sufficiently crushed (preferably blended) and thermally processed.
Drug therapy
The main drugs that can be used to relieve tenesmus are:
- antispasmodics (No-shpa, Papaverine, Spazmalgon), which help reduce intestinal colic and reduce the tone of the intestinal wall;
- prokinetics (Metoclopramide, Motilium), which improve peristalsis and normalize the movement of feces through the intestines, preventing incomplete bowel movements;
- probiotics (Bifidumbacterin, Linex, Bifiform) help normalize the balance of microflora;
- antidepressants and tranquilizers (Eglonil, Afobazol), which help normalize the psychological background, stopping attacks of aggression, helping to improve mood;
- anthelmintic drugs - used to detect helminthic infestation;
- antibacterial drugs - prescribed only if there are signs of intestinal infection (fever, diarrhea, hemocolitis) or based on the results of bacteriological culture of stool (carriage of pathogenic microflora).
Psychotherapy
Correction of the emotional background through psychotherapy sessions in some cases is the best way to treat tenesmus that has formed due to stress and depression.
However, this is not the only case where sessions can be useful. So, with chronic false urges, the patient becomes fixated on them, problems with the emotional background begin, which only aggravates the situation. According to statistics, more than 70% of patients with tenesmus need the help of a qualified psychologist.