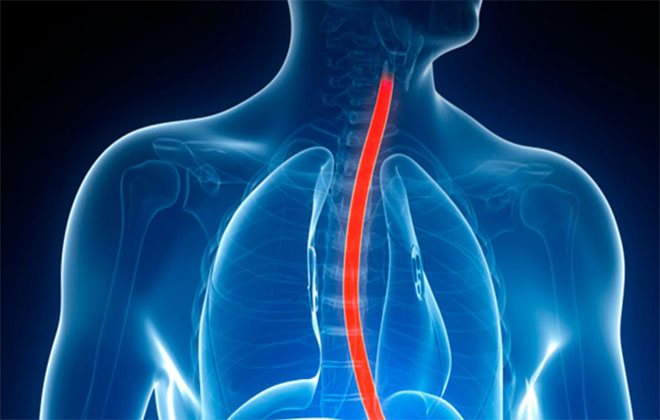
Varicose veins of the esophagus - what is it?
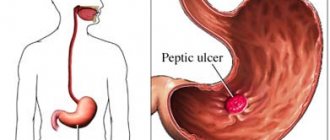
Varicose veins are characterized by damage to the gastrointestinal tract vessels - gaps and nodes are formed. The vessels twist, and their walls become thinner, as a result of which the mucous membrane becomes susceptible to inflammation and erosion.
The initial stage of development of the pathology has no symptoms, so it is almost impossible to determine it. The next condition that signals the disease is bleeding. Unfortunately, it becomes fatal.
Reference! VRVP has a code of 185.0 according to ICD-10 - the international classification of diseases in the 10th review.
How doctors can help
It is extremely necessary to treat varicose veins of the esophagus in a timely manner. Initially, it will be necessary to eliminate the disease that led to the development of the pathology, for example, problems with the cardiovascular system, liver disease, etc.

For esophageal varicose veins, treatment is mainly aimed at preventing bleeding. The main requirements for the patient in this case are a fuller awareness that the bleeding that has begun can threaten his life. Therefore, he must adhere to a certain gentle diet, avoid exercise and follow a daily routine.
Treatment is aimed at eliminating the underlying disease and symptoms of esophageal varices.
In this case, the doctor may prescribe a course of vitamin therapy and astringents.
If the bleeding is minor, treatment is carried out according to the following scheme:
- Transfusion of blood and colloid solutions.
- Taking medications that stop bleeding and constrict blood vessels.
- Electrocoagulation of a vessel that has been damaged.
- A probe is inserted into the esophagus, which is aimed at squeezing the bleeding vessels.
But still, the surgical method is the most effective in this case. If we look at statistics, there is evidence that the mortality rate of people after surgery from varicose veins is much lower than after conservative treatment. Patients must realize that this pathology is incurable, therefore, in order to avoid bleeding, which poses a clear threat to their life, they must strictly adhere to all doctor’s recommendations.
Classification of diseases
All cases of varicose veins can be divided into congenital and acquired. Congenital phlebectasia is a rare pathology that is accompanied by other, no less serious, diseases. This type is due to genetic predisposition. Acquired varicose veins occur due to impaired blood flow. Very common in patients with liver cirrhosis.
Depending on the severity of varicose veins, four stages of development are distinguished.
| Stages of development of VRVP | Vascular condition | Condition of blood vessels on x-ray | State of the gastrointestinal tract | Symptoms |
| 1st degree | A small number of dilated vessels | Dilated veins of the gastrointestinal tract are not detected | Satisfactory | Absent |
| 2nd degree | Dilated vessels wriggle, enlarged esophageal varices appear | A clear venous contour and areas of distended vessels can be observed | The mucous membrane is not affected | Unpleasant sensations when swallowing food |
| 3rd degree | The gaps in the vessels narrow, taking on a serpentine shape, and dilations begin to appear | Obvious swelling of blood vessels, venous nodes in the gastrointestinal tract | Thinned mucous membrane with minor inflammation and erosion | Belching and pain |
| 4th degree | The vessels are twisted, a large number of nodes with extensions are observed | The gastrointestinal tract is narrowed, on x-ray you can see polyp-shaped and grape-shaped expansions | Thinned mucous membrane with a significant amount of inflammation and erosion | There is a taste of blood |
How to treat
If a patient has varicose veins of the esophagus, it is necessary to treat first of all the pathology that provoked its appearance. Additionally, medications are prescribed that reduce the risk of massive bleeding, vitamin complexes and drugs necessary to suppress the production of acid in the stomach.
Important information: What anti-cellulite massage can be done for varicose veins (varicose veins) on the legs

In some cases, the introduction of colloidal solutions is justified. Drugs that are often included in the treatment regimen also include drugs that help narrow the lumen of blood vessels and strengthen their walls. Medicines that stimulate hematopoiesis may also be recommended. In severe cases, when conservative methods do not achieve a positive result, surgical treatment may be prescribed.
Endoscopic methods
For a disease such as varicose veins of the esophagus, treatment is often performed using low-traumatic endoscopic methods. The most widespread are intranasal and paravasal methods of administering sclerosant. In the first case, a special substance is introduced into the area of the node. In the second case, the sclerosant is introduced into the submycotic layer.
At the site of injection of the substance, blood flow is blocked and damaged tissue is replaced with connective tissue. This approach to treatment allows you to eliminate dilated veins with minimal risk of complications, but there is a high probability of relapse of the disease.
Balloon tamponade
This treatment method is used as part of surgical care when the patient develops massive bleeding from a dilated vessel. The balloon tamponade procedure for a disorder such as esophageal varicose veins involves the insertion of a special probe equipped with balloons into the esophagus. Air is pumped into these cavities of the apparatus.
Thus, the vessel is pressed, which leads to stopping bleeding. Nowadays this treatment method is used extremely rarely, because it is associated with a high risk of complications. There is a high probability of bleeding. This way you can block one bleeding area, but open up several more. Open bleeding can be treated using less traumatic methods.
Important information: Why you should not drink chicory if you have varicose veins
Surgical methods
When a patient's esophageal varices progress, treatment may require surgery. Often this therapy is resorted to when the vessels begin to bleed. These methods include:
- devascularization;
- venous bypass;
- transjugular intrahepatic portosystemic shunt.
The method of surgical intervention is selected individually, taking into account the degree of neglect of the process. When using this approach to treatment, the patient requires rehabilitation. The risk of re-expansion of the veins is extremely low.
Varicose veins of the esophagus: causes

The main factor causing expansion is excess pressure in the cavity of the portal vein. It transports blood from the stomach, pancreas, spleen to the liver. This phenomenon is called “portal hypertension.”
Excessive blood pressure is a consequence of such diseases:
- chronic hepatitis;
- cirrhosis;
- tuberculosis;
- neoplasms;
- amyloidosis;
- sclerosis;
- thrombosis;
- Budd-Chiari syndrome;
- cardiovascular failure.
Varicose veins of the esophagus with cirrhosis of the liver
Liver cirrhosis becomes a factor in the development of varicose veins in 70% of cases. With this pathology, healthy organ cells are replaced by scar tissue, which interferes with normal blood flow. Stagnation forms in the portal vein, which leads to varicose veins in the lower part of the esophagus.
Factors for the development of liver cirrhosis are:
- drinking alcohol;
- viral hepatitis;
- taking medications;
- genetic predisposition;
- In newborns, cirrhosis of the liver occurs due to diseases suffered by the mother during gestation: herpes, hepatitis, rubella.
Signs of varicose veins of the esophagus

Grade 1 esophageal varicose veins, which can develop over years, do not have obvious symptoms. Sometimes the patient may feel heartburn, heaviness in the chest, and belching. Periodically, the patient complains of discomfort when swallowing food. Sometimes VRVP is accompanied by a venous pattern on the anterior wall of the abdominal cavity.
Reference! The first symptoms, as a rule, appear several days before the onset of bleeding. It consists of significant heaviness in the chest area and a deterioration in the general condition of the patient. Ascites is sometimes observed.
Immediately after a vein rupture, the patient experiences the following symptoms of esophageal varicose veins:
- A sharp decrease in blood pressure.
- Vomiting with blood.
- Bloody stool.
- Tachycardia.
- Light bleeding is accompanied by weakness and symptoms of anemia.
Causes and symptoms of the disease
Esophageal varices are characterized by the presence of internal bleeding in the patient. The reasons why the disease develops can vary significantly. For example, bleeding may occur due to injury to a large vessel of the esophagus. This phenomenon is most often observed when a tumor grows into part of a large aorta. Sometimes the cause is mechanical damage. For example, if a foreign body with sharp edges enters the esophagus, it damages the walls of the esophagus, resulting in internal bleeding, which is quite difficult to stop.
Varicose veins in the lower part of the esophagus in most cases are formed due to congestion that occurs with cirrhosis. In this case, bleeding may occur spontaneously or after heavy physical exertion. Among other causes, doctors note Rendu-Osler disease. In rare cases, the causes lie in congenital pathologies of the esophagus. Recent studies have shown that esophageal varices develop due to thrombosis or sclerosis.
The symptoms that occur with this disease can vary significantly. Doctors say that in most cases with varicose veins of the esophagus, the patient has no characteristic symptoms at all. However, over time, the patient begins to feel heaviness in the chest. This sign is a harbinger of bleeding. Sometimes other symptoms appear, such as heartburn or belching. Such symptoms most often appear in people suffering from esophagitis or other chronic gastrointestinal diseases.
If acute bleeding develops, the patient develops streaks of blood in the sputum. Vomiting often occurs, in which blood can be seen. Pain in the chest area increases significantly. In rare cases, the patient experiences diarrhea.
If bleeding is not stopped in a timely manner, the patient develops anemia. It is manifested by rapid heartbeat, shortness of breath, general weakness and sudden weight loss.
Why are varicose veins of the esophagus dangerous?

Minor but regular bleeding can cause anemia. Significant - without medical intervention, they lead to the death of the patient. Before the onset of blood loss, the patient feels a salty taste and a slight tickling in the throat. After this, vomiting occurs with impurities of blood of various colors and consistencies.
The following factors can cause bleeding:
- lifting weights;
- increased blood pressure;
- binge eating;
- straining;
- ulcers;
- vomit.
Symptoms of the disease
The main manifestations depend on the severity of the condition. Grade 1 varicose veins of the esophagus are characterized by initial changes:
- VRV extension;
- expansion of vein diameter;
- bleeding;
- decrease in blood pressure;
- tachycardia;
- admixture of blood in vomit and feces.
Other characteristic symptoms: splenomegaly (enlarged spleen), increased bleeding, ascites, yellowing of the skin, itching and rashes - all these symptoms depend on the causes that caused esophageal varices.
Which doctor treats the disease?

First of all, you need to contact your local physician to make a diagnosis. When the disease becomes known, the doctor will give referrals to more specialized specialists: phlebologist, angiologist or gastroenterologist.
A phlebologist is a doctor of specialized practice. The angiologist’s specialization is extensive - he deals with pathologies of any vessels: veins, arteries, capillaries. During surgery, a gastroenterologist and a vascular surgeon will treat varicose veins.
Diagnosis of the disease
Diagnostic measures are aimed at identifying the root cause of varicose veins and clarifying the severity of the disease. After collecting anamnesis, the specialist prescribes clinical and instrumental research methods.
Diagnosis of VRVP is as follows:
- Anamnesis collection. The doctor collects information about the patient’s well-being and previous illnesses. Conducts an examination: determines the color of the skin, mucous membranes, diagnoses the presence of tumors, performs palpation and percussion.
- Then the specialist prescribes clinical studies of biomaterials: general and biochemical blood tests, coagulogram.
- Instrumental examination methods include esophagoscopy, ultrasound, and x-rays.
Radiography and esophagoscopy are the preferred research methods:
- When performing an X-ray, you can distinguish the contours of the esophagus, assess the condition of the mucous membrane and see accumulations.
- Fibroesophagoscopy is a more advanced method of examination. Thanks to it, you can assess the condition of the esophagus from the inside. But the study must be carried out very carefully, since it is possible to easily injure an already damaged organ, which will cause bleeding. With the help of esophagoscopy, you can determine the causes of the disease, its degree, and make a prediction about the subsequent rupture.
Diagnostics
In making the diagnosis of varicose veins, the following play a role:
- patient complaints;
- anamnesis of the disease and life (how long ago the complaints arose, how the disease proceeded, previous illnesses, in particular, hepatitis, cirrhosis, tumors);
- assessment of the patient’s objective status (pallor or yellowness of the skin, the presence of hemorrhages or spider veins on the skin, enlargement of the abdomen in general, the liver and spleen in particular, the presence of varicose veins on the anterior abdominal wall, swelling of the limbs and torso and other signs);
- laboratory tests (general blood count (leuko-, thrombocytopenia), biochemical blood test (increased levels of bilirubin, liver enzymes, cholesterol, decreased protein content), determination of parameters of the blood coagulation system; in case of bleeding, it is also necessary to determine the blood type, Rh factor and perform cross-compatibility test for 6 doses of er-mass);
- instrumental methods (esophagogastroduodenoscopy - EGDS), ultrasound of the abdominal organs, X-ray contrast examination of the esophagus).
Treatment
The basic treatment regimen for esophageal varicose veins is as follows:
- Treatment of the root cause of the disease.
- Delay in the process of vasodilation.
- Preventing the occurrence of hemorrhagic complications.
- Stop bleeding.
- Rehabilitation activities.
- Rule out relapse.
Grade 1 varicose veins of the esophagus

The main method of treating dilated veins of the esophagus at this stage is taking medications. It is mainly aimed at getting rid of the cause of varicose veins. Treatment is carried out by a gastroenterologist.
In addition to medications, the patient is prescribed:
- dietary nutrition;
- lack of physical activity;
- establish a sleep and rest schedule;
- prevention of esophagitis.
Esophageal varicose veins, grade 2
At this stage the patient is prescribed:
- medications that increase the acidity of gastric juice;
- hemostatics;
- mineral complexes to strengthen venous walls;
- iron-containing preparations;
- vasoconstrictor medications.
Grade 3 varicose veins of the esophagus

With the third degree of varicose veins of the stomach and esophagus, bleeding develops, so the primary task of doctors is to prevent rupture of blood vessels.
Treatment of varicose veins of the esophagus is carried out as follows:
- prescribe medications, prescribe a diet;
- transfusion of blood, plasma, red blood cells;
- Vasoconstrictor medications are administered.
If bleeding has already started, measures will be aimed at stopping the bleeding and rehabilitation:
- Vascular tamponade is performed using a Blackmore probe.
- Bandage the bleeding vessels. This event is called “esophageal vein ligation.”
- Blood transfusion or blood substitutes are given.
- Measures are taken to prevent infection of the mucous membrane and blood vessels.
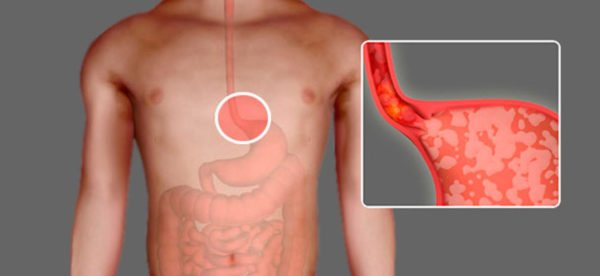
Classification
With such a pathological condition as varicose veins of the esophagus, the classification used by medical personnel is primarily determined by the stages of neglect of the process. According to this parameter, 3 degrees of the disease are distinguished. The degree of neglect of the process can only be determined by conducting a comprehensive examination, since symptoms may remain nonspecific for a long time.
- Grade 1 varicose veins of the esophagus reach a diameter of no more than 5 mm. They have a slightly elongated structure, but no pronounced nodes have yet been noted.
- Stage 2 vascular varicose vein disease is diagnosed when examination reveals severe tortuous deformation of the vessels. Their diameter expands to 10 mm. The veins are affected not only in the lower, but also in the middle part of the esophagus. At this stage, pronounced signs of pathology development appear.
- With grade 3 VRVP, the diameter of the veins increases to more than 10 mm. Thinning of the walls of blood vessels and the appearance of nodes that block the lumen of the esophagus by approximately 2/3 can be detected. Red spots appear on the surface of its mucosa.
Important information: Is it possible to massage the lower extremities (legs) with varicose veins (varicose veins) and how to do self-massage at home
Diet for varicose veins of the esophagus

Nutrition adjustment is one of the important points in the treatment of varicose veins. The patient will have to change his lifestyle so that sticking to the diet is comfortable, since he will have to follow the diet for the rest of his life.
If a pathology is detected, the patient, first of all, needs to establish a diet: during the day you should eat 4 to 6 times in small portions. The most nutritious meal should be at breakfast, and the lowest calorie meal should be at dinner.
In order for food to be digested better, the patient should prefer cooking methods such as boiling, steaming, and pureeing foods. Definitely, you need to give up fried foods.
Reference! The temperature of the food should be such as not to cause discomfort to the person while eating. Therefore, you should avoid hot and too cold foods.
The following types of products should be avoided:
- from solid foods that can damage the gastrointestinal mucosa: crackers, nuts, hard fruits, raw vegetables;
- from products that irritate the gastrointestinal tract: pickles, marinades, concentrated juices, spices;
- from fatty foods;
- from alcoholic, carbonated drinks;
- from coffee, chocolate.
And, on the contrary, it is worth adding to the diet:
- lean varieties of meat, fish, poultry;
- dishes that envelop the gastrointestinal tract: porridge and jelly;
- low-fat dairy and fermented milk products.
Prognosis for liver cirrhosis
Vascular disease of the gastrointestinal tract is characterized by high mortality. In cirrhosis it reaches 50%. Mortality does not depend on the nature of the bleeding, but on the severity of organ damage.
In 80% of cases, hemorrhage occurs on its own, so the likelihood of recovery is in those patients who have good liver condition. But 75% of patients are susceptible to relapse within the first two years.
To improve the condition of varicose veins, it is necessary to regularly undergo drug support and endoscopic treatment.
Although VRVP cannot be treated, the patient can live for decades if he maintains his condition with timely examinations, adjusts his diet and sleep and rest patterns. Be healthy!