It is a mistake to believe that a white coating on the tongue is a normal phenomenon of the body. The healthy color of the tongue is pink.
A thin white layer is allowed in the morning immediately after waking up, but it can be removed without any effort.
Whitish deposits accumulate in the mouth due to the presence of bacteria.
The bulk of bacteria collects closer to the root of the tongue.
The tip of the tongue is usually of normal color.
A thin, odorless layer is a normal phenomenon in the body.
The presence of an odor indicates the presence of some kind of disease, which caused the appearance of this feature in the oral cavity.
The thickness of the layer indicates the stage of the disease.
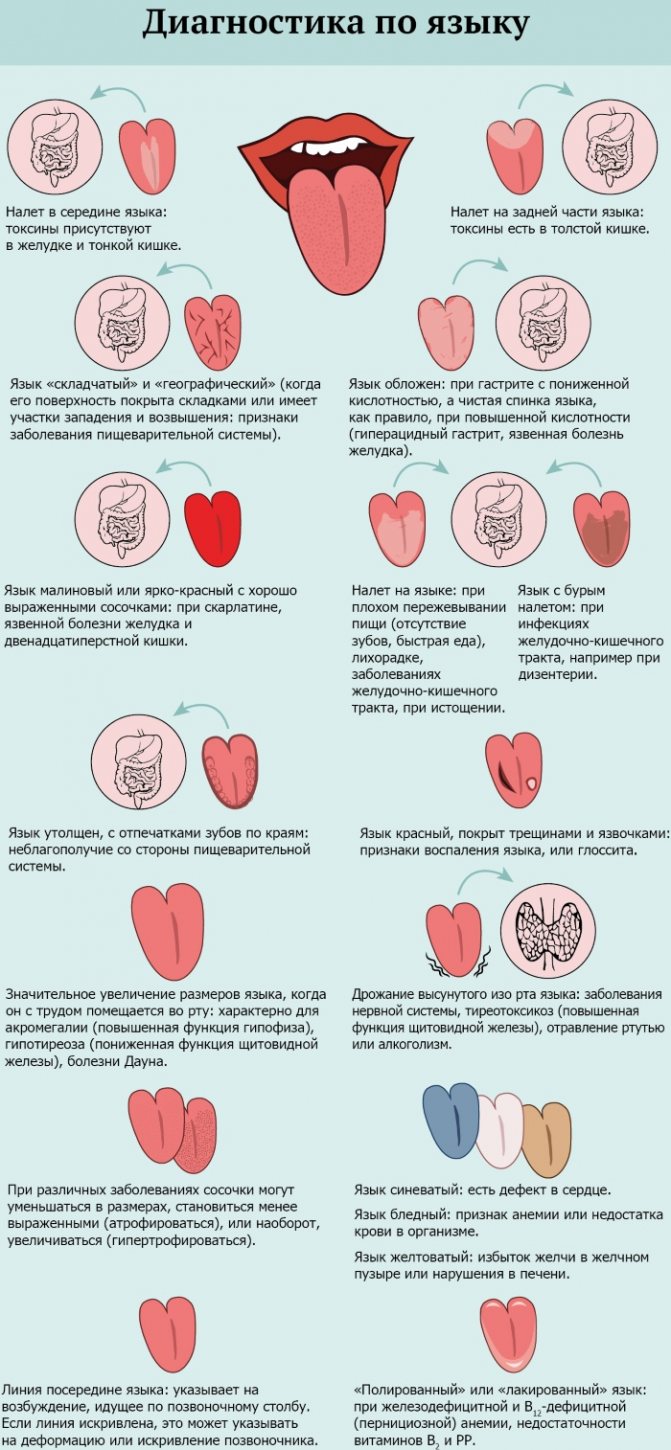
And by its location on the tongue it is possible to determine an unhealthy organ.
The tongue is covered with a white coating: reasons, what to do?
The human oral cavity is an indicator of the general condition of the body.
Ancient healers knew about this, successfully diagnosing many diseases by the presence of plaque on the surface of the tongue. And now, using these indicators, you can learn a lot about your health status and notice the development of certain pathological processes in time. Most often, a whitish coating appears on the tongue. This is not always a sign of illness. However, if the plaque is thick, has different shades, and the mouth feels bitter, dry, or has an unpleasant odor, we can talk about the presence of problems in the body. Of course, the doctor will determine the existing disease. Today we will talk about the possible reasons for this phenomenon.
So, why does dry mouth appear, a white coating on the tongue in adults? What are the causes and treatment for this phenomenon? Let's talk about it.
What does a healthy person's tongue look like?
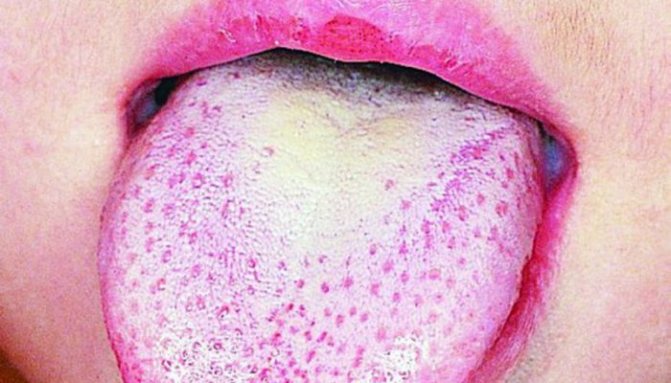
?
When everything is in order in the body, the tongue is not enlarged, moderately moist, and has a light pink tint. The papillae are not bright, moderately pronounced, their sensitivity is within normal limits. There is no bad breath.
In this case, the appearance of a light white, translucent coating is acceptable, which can be easily removed during cleaning. This is usually observed in the morning in every adult. After cleansing, plaque does not appear again throughout the day.
But, if the white coating is dense, persistent, difficult to clean off, and has an unpleasant odor, we can assume the development of a pathological process. So, why is the tongue covered with a white coating, what are the reasons for this?
Coated tongue - causes
Very often, a coated tongue is a sign of certain diseases. Let's briefly look at some of them:
— This phenomenon is very often observed during exacerbation of gastritis. If the acidity of the stomach is increased, the tongue becomes rough and excessively moist. With low acidity, it is, on the contrary, smooth and dry.
- Dry mouth, bitterness, white coating on the tongue, in particular at the root, may be a sign of a peptic ulcer. These symptoms remain throughout the treatment.
— In adult patients, the described phenomenon may be a sign of poor liver function, kidney disease, or pancreatic pathology. Accompanied by dry mouth and an unpleasant, bitter odor.
— Stomatitis may be accompanied by a coating on the tongue. In this case, it is white and moist, but dryness and bitterness in the mouth rarely appear.
— With angina, there is usually a coating of the throat and tongue, dryness of the oral mucosa.
— Similar symptoms can be observed with dysentery. If the white coating is pronounced - thick and dense, this indicates large-scale intoxication of the body.
— White plaque is always present with oral candidiasis.
— The cause may also be helminthic infestations.
— HIV infection, which is at the AIDS stage, is also accompanied by a thick, white coating of the tongue. This is due to the activity of bacteria, viruses or fungi. With normal functioning of the immune system, most of these infections simply do not develop.
Disorders not associated with pathology
Of course, white coating on the tongue in adults is not always a sign of an existing disease. For example, this may be a consequence of insufficient oral hygiene or excessive consumption of sweets. It is observed with smoking and alcohol consumption.
In addition, hormonal imbalance in the body, for example, during menopause, can also be accompanied by a persistent white coating and dryness of the oral mucosa.
What to do if there is a white coating on your tongue
?
To get rid of a coated tongue, you must cure the disease that caused its appearance.
The first step is to visit a dentist, who will carefully examine the oral cavity and conduct an examination to determine the possible cause of the plaque. If there is a suspicion of internal pathology, he will refer the patient to other specialists, in particular: a gastroenterologist, endocrinologist or infectious disease specialist.
If, as a result of the diagnosis, a disease of the digestive tract is discovered, further treatment will be carried out by a gastroenterologist. If the cause of the white plaque is thrush (candidiasis), the specialist will prescribe antifungal drugs.
Symptomatic therapy is carried out using drugs for antiseptic treatment of the mouth. An important factor in treatment is also the elimination of factors that provoke the appearance of plaque.
Home remedies for plaque
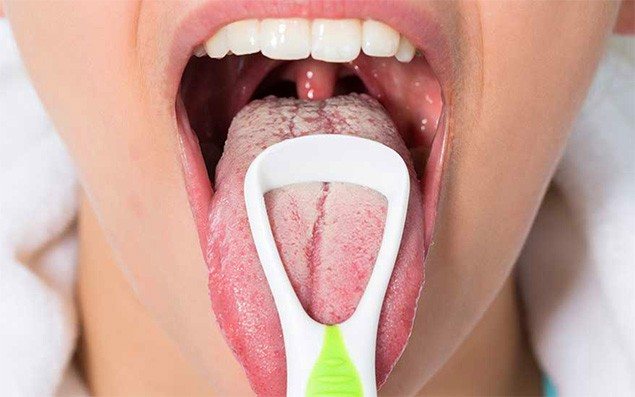
Simultaneously with the treatment and the implementation of medical recommendations, the patient is recommended to regularly, thoroughly cleanse the tongue of plaque. To do this, you can use a special scraper designed to clean the tongue.
An effective remedy is a paste that you can make yourself by mixing turmeric powder with lemon juice. This mixture copes well with plaque and disinfects the oral cavity.
To cleanse and prevent various inflammations, it is useful to use vegetable oil. You need to put 1 tablespoon of oil in your mouth and slowly rinse your mouth for 10 minutes. Then be sure to spit it out and brush your teeth. To enhance the disinfecting effect, you can add a few salt crystals to the oil. Be healthy!
Congestion in a child
Language is a kind of reflection of the body. An experienced specialist can easily determine by the language on the tongue which organ has malfunctions or problems. When you see your pediatrician, your baby's tongue is always examined. Most children have a white coating. It is very rare to find a coating of any other color on a child. In infants, a white coated tongue may indicate the presence of thrush, but in older adults it may indicate stomatitis or problems with the gastrointestinal tract. Also, children may be affected by infectious diseases, influenza and scarlet fever. Also, another cause of white plaque may be gastritis and dysbacteriosis.
In any case, if you notice a coating of any color on your baby’s tongue, contact your pediatrician for advice. Prevention doesn't hurt anyone.
Why there is a white coating on the tongue - causes of tongue coating in children and adults
Since time immemorial, the state of the tongue has been used to diagnose body diseases. The tongue signals even before the onset of pain and clear signs of illness. Ancient healers believed that the patient was not completely cured until the tongue looked healthy, even if all the symptoms of the underlying disease had already gone away.
A white coating on the tongue occurs when the processes of keratinization of filiform papillae cells are disrupted. At the same time, the horny masses become thick and difficult to clean. The tongue becomes coated due to various reasons: gastrointestinal pathology, infectious diseases, poor oral hygiene, taking medications.
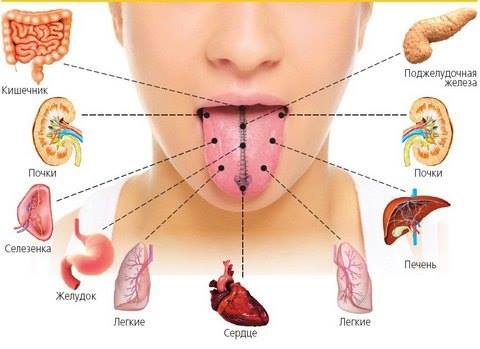
In Ayurveda, certain organs correspond to the tongue zones:
- anterior third – heart and liver
- middle – spleen, pancreas and stomach
- root - intestines
- lateral areas - kidneys
What should a normal language look like?
When should you start worrying?
- Color – pale pink
- Humidity – moderate
- Papillae – moderately pronounced
- Sensitivity, normal functioning
- It is acceptable to have a white-pink, easily cleaned coating on the tongue
- There is no unpleasant smell
- The tongue changes in size, swells, and teeth marks appear
- The color changes from pale pink to white, yellow, gray or other on the back of the tongue, the lateral surfaces become bright red
- Dryness appears
- Some papillae, especially on the base of the tongue, enlarge and look like small red spots
- Burning sensation, pain, and taste sensitivity begin to disturb
- On the back of the tongue there is a coating of different colors (most often white or yellow), abundant, difficult to clean, and after removal it quickly returns again
- There is a pronounced bad breath
The reasons for the appearance of white plaque on the tongue are varied:
- Acute and chronic lesions of the tongue itself: inflammation, infections, exposure to medications
- Lesions of the tongue in various diseases - infectious, internal organs, hypovitaminosis, dysbacteriosis, oncology and others
- Not associated with diseases: poor hygiene, eating white foods, alcohol, smoking, unsuitable toothpaste and mouthwash.
Often, a white coating on the tongue is a signal of gastrointestinal diseases, a consequence of eating white and sweet foods, poor oral hygiene or, conversely, using inappropriate hygiene products, smoking, drinking alcohol and thrush. Scientists have proven that even hormonal changes such as menopause lead to a coated tongue, dryness and burning (see symptoms of menopause in women).
Gastrointestinal diseases
with thrush in the area of the tongue, plaque and burning are disturbing, while white masses of a cheesy consistency are poorly removed, and a wound surface is found underneath them. Candidiasis is a common fungal disease that develops with long-term use of antibiotics, strong medications (cytostatics, glucocorticosteroids), drugs, oral contraceptives, alcohol abuse, in people with weakened immunity due to HIV infection, dysbacteriosis, hypovitaminosis, and severe general diseases.
Other reasons
- A white coating on the tongue appears after cottage cheese, milk, kefir, and cheese.
- When eating sweet foods, bacteria and fungi multiply quickly, so they provoke the formation of plaque. It does not pose any threat, since it is easily cleaned and does not form again.
- The tongue must be cleaned daily, as microscopic food debris accumulates on its papillae, causing microbes to multiply and an unpleasant odor to appear.
- downside: some toothpastes and rinses cause individual intolerance, which can result in chemical or allergic lesions of the mucous membrane of varying severity, leading to the fact that the tongue is constantly coated with a white coating.
- in case of poisoning with toxic substances, the tongue is coated with a dense white coating. Erosion and ulcers with dead cells can be found on the mucous membrane. The general condition suffers.
- smoking negatively affects the mucous membrane of the tongue through chemical factors and elevated temperature.
- Alcohol intake reduces the water content in the body and causes dry mouth. Everywhere the mucous membrane of the tongue reacts with the appearance of plaque.
Read also: Causes of white coating at the base of the tongue
It is for this reason that after a stormy party there is a high probability of finding a tongue with a white coating in the morning.
Causes of coated tongue
A specialist can determine exactly what diseases you have based on the appearance of your tongue alone. In some cases, you may notice that the tongue is coated. It can have different shapes, thicknesses and colors. It appears because there are many different bacteria . In the absence of diseases of the internal organs, as well as with proper oral hygiene, the plaque is very thin and can be easily separated. Even in a completely healthy person it is present. It may vary due to seasonal changes. In summer it is denser, in autumn it is inconspicuous and dry, and in winter there is a yellowish tint.
If your tongue is covered with a thick, strange-colored coating, then you urgently need to go to a specialist - there is something wrong with your body. The reasons for this may be:
- Dehydration or a large amount of water in the body depends on the location and color of the plaque.
- Cholecystitis, hepatitis.
- Infectious diseases.
- Candidiasis.
- Reduced immunity.
- Problems with the lungs and kidneys.
- Problems of the gastrointestinal tract (inflammation in the intestines or disruption of its functioning, worms).
- Alcoholism (in rare cases).
Also, the causes of a coated tongue can be the use of certain medications and smoking, improper and irregular oral hygiene.
Tongue diseases
- catarrhal, ulcerative, desquamative glossitis, “geographical” tongue
With desquamative and “geographical” glossitis, the tongue is covered with a white coating with red spots. Desquamative glossitis is a sign of general dysbiosis and serious systemic diseases of the body. Red spots represent areas where either the epithelium is absent or the altered papillae of the tongue are grouped together. The cause of “geographical” glossitis is not clear; inflammation in the areas of desquamation of epithelial cells is not detected. It is believed that the tongue becomes such a bizarre shape as a result of a genetic disorder.
Galvanic stomatitis occurs when there are metal prostheses in the mouth and is manifested by a white coating, spots in the form of pimples, and in severe cases, erosion and burning.
The use of carbolic acid, formaldehyde, antibiotics, sulfonamides, and even substances such as eucalyptol and anise oil found in toothpastes and cosmetics can cause tongue damage.
Infectious diseases
This is primarily scarlet fever, dysentery, diphtheria, tonsillitis, gonorrhea, HIV infection.
If a person is sick with one of these infectious diseases, he is unlikely to find out why there is a white coating on his tongue. These are quite serious diseases that bring suffering primarily with their main symptoms: high fever, pain, rashes, discomfort, diarrhea and others.
The doctor may see a red tongue with a white coating, pinpoint rashes on the tongue, ulcers also covered with a white coating and other changes that will be secondary to these infectious pathologies. After infection with HIV in the AIDS stage, a white coating on the tongue appears due to fungal, bacterial, viral infections, which, in the normal state of the immune system, do not make themselves felt.
Treatment methods
A blue coating on the tongue can be removed only after the exact cause of the change in its color has been determined. A gastroenterologist, dentist or family doctor will help you find out the reason. Only after examination by specialists, medical history and additional laboratory tests can appropriate treatment be selected.
It is also important to know that the tongue is visually divided into certain zones, which, by changing color, accurately indicate health problems in a particular organ. For example, the tip of the tongue is considered the upper part of the body, and the root is considered the lower part. Depending on which part of it the cyanosis is observed, one can judge the nature of the disease. The table below shows a map of the language.
| Tongue area | What organs belong to it? |
| The tip turned blue | There are problems with the functioning of the heart and lungs. |
| Horizontal part of the middle of the tongue | Indicates that the stomach, spleen, liver and pancreas need to be examined urgently. |
| Blue root | The intestines require urgent cleansing of toxins and taking prebiotics. |
| Blue sides of tongue | The function of the kidneys and urine excretion pathways is impaired. |
| The middle of the tongue is the vertical part | There are serious problems with the spine. |
The saturation of the blue color will also help to make a more accurate diagnosis:
- blue-violet tongue – heart failure;
- cyanosis of the oral mucosa – cyanosis;
- light blue tint in the center – anemia;
- bluish tint – blood circulation is impaired;
- blue-black spots – problems with the adrenal glands;
- blue-blue or blue-violet tint – pathologies of the blood and lungs.
If the cause of your blue tongue is the wine you drank, then don’t worry, the problem will disappear on its own, just brush your teeth and tongue.
A blue coating on the tongue is a symptom of coronavirus, but you need to remember that there is no vaccine for this disease. If an illness is detected, then urgent self-isolation and calling a health worker at home is necessary. To reduce high fever and relieve pain, take Paracetamol.
But you should not overdo it with it, as this drug has a toxic effect. They fight the symptoms of coronavirus with drugs to strengthen the immune system, proper nutrition and active physical activity.
Antibiotics
If it is determined that the cause of the blue tongue is related to the digestive system, then the specialist may recommend taking antibiotics, for example, Amoxicillin. This is an antimicrobial agent from the penicillin group. It is a broad-spectrum drug that effectively fights the bacterium Helicobacter pylori.

The drug is available in the form of granules, capsules, suspensions and tablets. The drug is indicated for infectious lesions of the digestive organs; it destroys bacterial cells and leads to their death. The course and dosage are selected individually.
Antispasmodics
Antispasmodics, for example, No-Shpa, may also be recommended. It affects smooth muscle cells and does not penetrate the brain. With their help, it is possible to stop the flow of calcium ions and some enzymes, thereby stopping muscle contraction.
Novigan
Novigan is a drug available in tablet form, which is recommended for use for renal and intestinal colic. This drug can harm people with serious intestinal diseases and is contraindicated for heart, kidney and liver diseases.
For vitamin deficiency, taking vitamins is recommended, and they should also be present in the daily diet.
Anti-inflammatory drugs
Anti-inflammatory drugs will help relieve inflammation in the digestive organs and abdominal cavity. Among the effective drugs, Mezavant and Salosinal can be distinguished.
Immunomodulators are also important, which are additionally prescribed for the inflammatory process. Medicines such as Viferon and Immunal are suitable. You can also use natural ingredients. So, for example, take 40 drops of alcohol tincture of Echinacea or Eleutherococcus every day.
Traditional methods
The blue coating observed on the tongue also accepts the use of traditional medicine. Decoctions and infusions of medicinal herbs are recommended for rinsing the mouth.
You can use the following recipes:

| Chamomile flowers | You need to take 1 tbsp. l. dry raw materials, pour 1 tbsp. boiling water, leave for 40 minutes. let it brew, then strain and rinse your mouth twice a day. | Duration of therapy is 10-14 days. |
| Calendula flowers | The decoction should be prepared as follows: take 1 tbsp. l. dried calendula flowers, pour 1 tbsp. cold water and place in a water bath, wait for the liquid to boil. Cool the broth, strain and rinse the mouth after each meal. | The duration of therapy lasts until the cyanosis disappears from the tongue. |
| Cinnamon and cloves | Take 5 buds of cloves and ½ tbsp. l. cinnamon powder, pour all 1 tbsp. boiling water and leave for 20 minutes. brew. Rinse your mouth while the mixture is warm. | Duration of therapy is 10 days. |
Diet
There are many reasons that provoke a bluish tint. Treatment is selected after identifying the cause, but before you start taking medications you need to change your diet.
First of all, you should exclude the following products:
- fast foods;
- fatty meats;
- nothing spicy or salty;
- remove marinades and smoked meats;
- completely eliminate carbonated drinks and alcohol-containing drinks;
- no mushrooms;
- as little flour and sweet as possible.
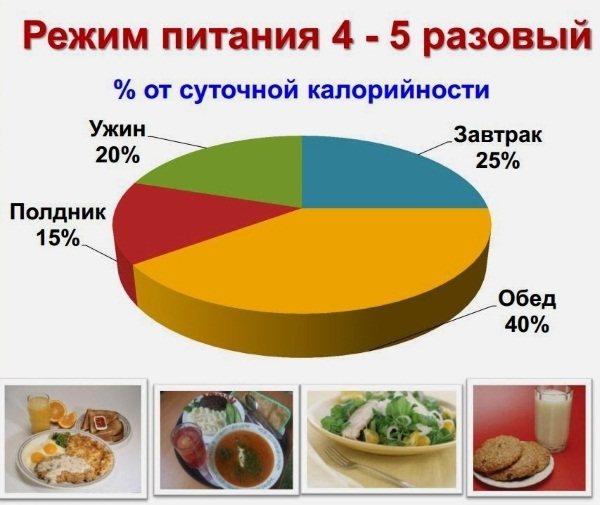
You need to eat up to 6 times a day, in small portions. Give preference to fresh vegetables and fruits, more lean meat, but better baked or boiled. Be sure to consume porridge and fermented milk products.
A blue tongue is the first sign that you need to sound the alarm and seek help from a specialist. Plaque on the tongue can be easily cleared with medicinal decoctions and brushing with a toothbrush, but this will not remove the cause and the cyanosis will soon reappear. Only eliminating the causes of such plaque will help prevent serious complications.
White coating on the child's tongue
Children may also develop a white coating on the tongue. Parents should not worry in the following cases:
- plaque covers the tongue with a thin layer and can be easily removed with a brush
- the child has just eaten milk, dairy or fermented milk products
- the baby does not like to brush his teeth, eats a lot of sweets - in this case, of course, you need to worry, but only in order to limit sweets and accustom the child to regular oral hygiene. The search for any disease should begin when these measures do not lead to clearing of the tongue.
- the child drew with white felt-tip pens, pencils, paints, and chalk. All these instruments could easily fall into the young artist’s mouth.
What to do if parents see a strong white coating on the baby’s tongue? The child probably has thrush - this is a common fungal disease of newborns, especially in the absence of breastfeeding, prematurity, improper care, hypothermia or overheating.
Plaque on the tongue of a newborn with thrush brings a lot of suffering, the child refuses to breastfeed and cries constantly. He experiences burning and pain on the mucous membrane, erosions are found under the plaque. The risk of developing thrush increases when the mother herself or the child eats sweets if complementary feeding has already been introduced (see complementary feeding table for children under one year of age).
Other oral problems also cause white plaque to appear:
- stomatitis - inflammation of the mucous membrane of the entire oral cavity (see stomatitis in children)
- glossitis - inflammation of the tongue
- caries and its complications
- tonsillitis - inflammation of the tonsils, tonsillitis (see treatment of tonsillitis in a child)
- pharyngitis and laryngitis are infectious diseases of the pharynx and larynx). In these cases, there is direct damage to the tongue by microbial plaque and intoxication.
You can also see a white coating on a baby’s tongue with more serious diseases:
- Scarlet fever is a childhood infectious disease characterized by a rash
- diphtheria is a severe childhood infection characterized by a white coating in the mouth
- diseases of the gastrointestinal tract: gastritis, enterocolitis, dysbacteriosis
- ARVI and influenza
- chronic hypovitaminosis
Possible reasons
Every person should perform oral hygiene procedures twice a day. During hygiene procedures, conduct a visual inspection of the tongue: is there any plaque and what color is it.

A change in shade may indicate serious problems in the body in one or another organ.
Red wine
Not all types of wine stain the tongue and lips. It all depends on the quality of the drink, the substances included in its composition and the grape variety. The most colorful wines are those that have been aged in oak barrels. Also, very young wine, which has just been brought from the vineyard and has not yet been aged in a barrel, can stain the lips.
Much depends on the grape variety. Varieties such as cabernet, shiraz, and pinotage have very thick skins that contain dye, but it is natural. Without this dye, you won’t get a beautiful wine, but your tongue and lips will turn blue after drinking it.
COVID-19 (coronavirus)
A blue coating on the tongue is one of the signs of coronavirus. The first signs of the virus are a sore throat, dry cough, fever and discoloration of the tongue. But not all patients note the appearance of plaque on the tongue. It quickly passes under the influence of powerful antibacterial and immunomodulatory therapy.
Chemotherapy
Oncology or cancer is a disease characterized by uncontrolled division and growth of pathological cells. These cells are called malignant. If cancer cells are detected in the body, chemotherapy is recommended.

It includes drugs that kill cancer cells in the body. These drugs kill cancer cells, but also harm healthy ones. Chemotherapy can cause a lot of unwanted effects, including color changes.
Cyanosis
When a person has problems with the vascular system, the level of oxygen in the blood decreases. As a result, a low level provokes a change in the color of the skin and the mucous membranes of the mouth and tongue acquire a bluish tint.
Anemia
When there is a lack of folic acid, iron and vitamin B12 in the human body, this indicates that problems will affect all internal organs. Anemia can be detected by pale skin and a blue tongue.
Diamond-shaped glossitis
The development of the disease can be determined by the dense base of the tongue and blue color. The disease itself occurs without any symptoms. Often the disease manifests itself in men who have considerable experience as smokers.
Vascular and cardiac insufficiency
A blue coating on the tongue will tell you about a similar problem long before any other signs of the disease appear. If a blue tint of the tongue is observed in its lower part, then this indicates that there is a disorder in the circulatory system, which is additionally aggravated by cardiopulmonary failure.
Kidney failure
This disease is accompanied by disturbances in the formation and excretion of urine. With this disease, the tongue at the edges of the throat itself becomes bluish in color.
Poisoning
A blue coating on the tongue may indicate that the body has received a serious toxic dose of heavy metals.

Mercury vapor poisoning. Symptoms
This often indicates that mercury vapor has entered the body.
Inflammation
An inflammatory process that affects organs in the abdominal cavity may be accompanied by high fever, pain in the abdominal area and a bluish color of the tongue.
Diagnostics
Who should I contact if I find a white coating on the tongue of an adult or child?
Of course, the first doctor is a dentist. He will conduct a thorough examination of the oral cavity, palpate the lymph nodes, and try to find out the possible cause of the plaque. If necessary, the doctor will refer the patient for a consultation with a gastroenterologist, infectious disease specialist, endocrinologist and other specialists.
You can independently take a general blood and urine test, culture from the mucous membrane of the tongue, test for HIV, syphilis, hepatitis B and C. The results of these tests will help the doctor make the correct diagnosis.
Treatment of white plaque on the tongue is aimed at eliminating the cause and symptoms. You should trust the treatment only to a specialist, without doing it yourself, since a white coating on the tongue can be a symptom of a serious illness, including tongue cancer.
The first signs of pneumonia
Experts cannot say with certainty which symptoms of pneumonia can be classified as strictly specific. The initial manifestations of the disease are similar to other inflammatory pathologies of the respiratory tract, and the signs of pneumonia in an adult are highly dependent on age, the state of the immune system and the type of pneumonia. The symptoms of acute, chronic, aspiration, bilateral or focal pneumonia vary greatly. However, the development of the disease can be suspected by the characteristic features of its usual manifestations:

- Cough, chest pain. At the very beginning of the disease, a dry, obsessive cough is observed, but sometimes it can be rare and mild. As the inflammatory process develops, the cough becomes wet, with mucous sputum of a yellow-green or “rusty” color. During coughing attacks and when taking deep breaths, the patient experiences stabbing pain in the chest, and later back pain may be added to it.
- Shortness of breath, lack of air. In pneumonia, bacterial microorganisms disrupt the functioning of the alveoli, the branches of the lung tissue. They stop participating in the breathing process, and this leads to a lack of oxygen. The patient's breathing becomes shallow, shallow and rapid, and he experiences shortness of breath.
- Heat. In normal cases, in the early stages of pneumonia, the temperature rises sharply to 38-39°C. Before this, the patient often experiences prolonged chills. During the initial diagnosis of the disease, special attention is paid to this sign of pneumonia in an adult. With a pulmonary infection, the temperature constantly fluctuates, either dropping or rising to its previous high value.
- Severe weakness, fatigue. Infectious pathogens that affect the lungs release toxins that poison the body and cause a state of general weakness. It is accompanied by dizziness, headache, confusion, loss of appetite, and sleep disturbances. If intoxication continues to develop, the patient develops additional disorders: gastrointestinal disorders, tachycardia, pain in joints and bones.

What is a raid?
Most often, a coated tongue can be observed in the morning. This is due to the fact that at night it is in a motionless state and particles of eaten food, epithelium, bacteria and fungi accumulate on it; after sleep, this feature is most noticeable. When the plaque is permanent, difficult to separate and has a large thickness, this indicates the presence of a disease.
What does a healthy tongue look like? The physiological norm is a light pink tint with visualized papillae. Plaque can appear as a result of many chronic and acute diseases. On a healthy tongue, the plaque is light in color, small in thickness and unevenly distributed. In addition, it should be easy to separate and not cause discomfort in the oral cavity.

Main reasons
By examining the tongue, you can suspect the presence of health problems. A certain localization of plaque suggests the development of a particular pathology. Disease of the internal organs is expressed in various ways, so examination is an integral part of any initial examination by a doctor. When the correct treatment is prescribed, it is possible to get rid of the pathological plaque and return the tongue to its natural color. Localization of changes depending on diseases:
- Pathology of the cardiovascular system is characterized by its location in the tip area. This localization is also characteristic of problems with the respiratory system.
- The longitudinal fold is a projection of the spinal column, therefore, if plaque is located in this area and if there is constant pain in the spine, it is recommended to consult a vertebrologist.
- The posterior surface of the anterior third of the tongue is the projection of the organs responsible for the production and secretion of bile. If there is persistent plaque in this area, it is necessary to suspect the development of pathology in the area of the liver and gallbladder.
- The middle third of the tongue can be used to judge the condition of the stomach and spleen. Changes localized to this area suggest gastritis, ulcers, or hepatosplenomegaly.
- The root of the tongue becomes covered with plaque in the event of persistent pathology of the underlying parts of the digestive tract.
Read also: Dark brown coating on the tongue
Brown coated tongue
A brown coated tongue can be caused by many different reasons.
If you have a yellow-brown coating, this indicates that you may have worsened respiratory tract diseases, inflamed joints, or impaired lymph flow.
Diseases of the bronchi and lungs, drug abuse, chronic alcoholism and problems with the gastrointestinal tract are indicated by a yellow-brown coating.
dysbiosis , diseases of the gallbladder, liver and kidneys, severe gastrointestinal diseases, and ARVI diseases are indicated by a dark brown coating . In such cases, taxation is the first alarm bell, after which you need to immediately contact a specialist.
There are many diseases that are practically asymptomatic, but then develop into chronic ones. Many people think that the body does not signal about such diseases, but this is not the case. It’s just that some people didn’t pay any attention to such signals. And such a signal is a brown coating on the tongue.
This plaque indicates the following diseases :
- Brown tongue coating may indicate a lack of vitamins, especially group B.
- Dehydration. High water consumption does not always help. It is for this reason that it is necessary to seek advice from a specialist.
- Advanced stomatitis. In this case, you need to urgently contact a specialist.
- If you have a brown coating on your tongue, and along with it nausea, weakness and dizziness, then this indicates poisoning of the body. Consulting a specialist will help you get rid of all the symptoms.
- Diseases of the oral cavity that were caused by fungus . In this case, you need to go to the doctor so that he can prescribe you a course of therapy.
- Taking medications such as Malavit, faringosept or antibiotics. Over time, the coating on the tongue will disappear.
- Congestion caused by drinking strong coffee and tea, chocolate or smoking. This coating is harmless and can be removed by performing hygienic procedures.
- Morning brown plaque accumulated on the tip of the tongue indicates disturbances in the functioning of the lungs and bronchi, or, if it accumulates on the root of the tongue, then the functioning of the digestive system is disrupted.
Diseases that cause white plaque
Why is my tongue covered with a white coating? There are a number of pathologies that contribute to the formation of changes on the surface of the tongue. They are mainly associated with improper functioning of the gastrointestinal tract. Various infectious diseases also make a significant contribution to the development of this symptom. Plaque can be caused by excessive bacterial, viral and fungal activity.
Pathology of the digestive tract
Gastritis is a disease caused by inflammation of the mucous layer of the stomach. The pathology is characterized by a long course, accompanied by dystrophic changes in the wall of the stomach. As a result of these processes, the glandular structures of the stomach are replaced by fibrous tissue. The diagnosis is made based on histological examination of the mucous membrane. The disease may be asymptomatic and not cause any discomfort.
The tongue with gastritis will be covered with a grayish coating, of high density, located in the middle and posterior third (except for the lateral sections). If gastritis is hyperacid in nature, then the symptoms are accompanied by an unpleasant aftertaste, and the plaque becomes pale yellow. The density of changes in the tongue depends on the severity of the disease. In addition, when the gastric mucosa is inflamed, a white coating is combined with a dry tongue. It acquires a grayish tint when gastritis is accompanied by low acidity. If inflammation of the mucous membrane is complicated by the appearance of an ulcer, then the changes will be denser in consistency and located closer to the root.
With gastric carcinoma, the plaque will be dense, thick and evenly distributed over the entire surface of the tongue. If such changes are accompanied by a sweetish-metallic odor from the oral cavity, then the development of gastric bleeding can be assumed.
If the papillae atrophy and the tongue becomes dry and white with plaque, then these signs indicate pancreatitis. In addition, it has been recorded that a yellowish coating on the tongue may precede acute inflammation of the pancreas. Intestinal inflammation, as well as prolonged congestion in the digestive tract, are accompanied by an unpleasant odor and a light coating on the tongue. Young children are characterized by the appearance of plaque on the tongue during prolonged diarrhea, accompanied by a decrease in the total amount of circulating fluid in the body.
Diseases of the liver and gall bladder are characterized by a change in plaque color from pale white to yellow-green. Similar changes are characteristic of obstructive jaundice and hepatitis.
Other diseases
Other causes of plaque on the tongue are infectious diseases. For example, with scarlet fever, a pale gray film appears on the tongue, on which teeth prints are visualized. With the development of dysentery, the plaque will be thick, difficult to remove, with the subsequent formation of small ulcers at the site of the former localization.
In addition to all the above-mentioned diseases, the tongue can be covered with a white coating even with a normal increase in temperature. Fever is often accompanied by changes in the oral cavity. However, all symptoms begin to quickly subside as soon as adequate treatment is prescribed.
Damage to the oral mucosa by a fungus from the genus Candida is manifested by the formation of ulcers and the formation of a white film that is unevenly distributed over the surface of the tongue. It is not uncommon for the tongue and membranes of the mouth to become inflamed during candidiasis, while patients also complain of severe itching. There is a risk group for candidiasis, which includes:
- HIV-infected;
- Pregnant;
- Newborns;
- Elderly people.
Treatment of plaque on the tongue can be etiological or local. For local processing, you only need a small spatula, which is convenient for removing the film from the tongue. Dentists recommend performing this procedure twice a day. It is also necessary to brush your teeth and treat the oral cavity with special disinfectant solutions after each meal. Such actions will reduce the number of pathogenic microorganisms involved in the formation of annoying plaque.
It must be remembered that for a complete recovery, you need to focus your energy on fighting the underlying disease. With the development of hyperacid gastritis, drugs that reduce gastric acidity (Omeprazole, Famotidine, etc.) are prescribed. In case of hepatitis, interferon therapy comes to the fore. Obstructive jaundice is not treated conservatively. As a rule, this disease occurs due to a violation of the outflow of bile due to a stone stuck in the bile duct. The patient requires treatment in a surgical hospital.
The information presented in the article is not a guide to action. To receive quality medical care, you must seek advice from a specialist.
For therapeutic purposes, antifungal drugs are used to eliminate signs of oral candidiasis. Pregnant women and young children should not take such medications. To treat this group of patients, topical drugs are used, as a rule, these are drugs from the cain group (lidocaine, novocaine).
What does the color of the tongue mean?
According to the practice of Ayurveda, the color of the tongue eloquently communicates problems with internal organs. Having carried out a competent diagnosis and knowing what color of the tongue is typical for what diseases, you can determine what a person is sick with.
They take into account not only the color of the mucous membrane itself, but also the color of the plaque. An important factor is the amount of plaque, as well as the nature of its distribution over the surface. Based on these signs, you can not only determine the disease itself, but also draw a conclusion about the severity of its course.
Plaque is not always a sign of pathology. It is also present in a person who is completely healthy. The normal color of the tongue is pale pink. And the coating is distinguished by a white or grayish tint, and there is very little of it.
It should not be dense, the pink color should be visible through it. If the surface layer thickens to such an extent that the natural color of the tongue is not even visible and becomes loose, then there is reason to assume the development of a disease.
Gastritis, sore throat, liver disease - all this is revealed by the color of the tongue and the plaque on it. Usually, in the initial stages of disease, the plaque is white. Worsening of the disease causes a change from white to gray. This means that the symptoms are intensifying, and they will intensify in direct proportion to the darkening of the plaque.
White
White color is a sign of fungal infections in the body - thrush, as well as acute respiratory viral infections, influenza. It may indicate a lack of water in the body. Also, a coating of this color appears with quite serious diseases of the gastrointestinal tract - gastritis, ulcers, stomach cancer.
Hypovitaminosis is also characterized by a whitish coating.
Gray color
Gray plaque usually also indicates problems with the stomach or gastrointestinal tract. A person who has such a plaque may develop a stomach ulcer (in this case, the white plaque is combined with hunger pains), chronic gastritis (complemented by heaviness in the stomach).
Yellow color
The color of the tongue in case of gallbladder diseases is no longer white, but yellow. There is a possibility of bile accumulation in the body; it is necessary to check the correct functioning of the liver.
A yellowish coating is characteristic of acute pancreatitis and gastritis. The yellow color of the tongue is typical in hepatitis and cirrhosis of the liver.
Less serious causes of yellow plaque include bacterial and fungal infections.
A dirty yellow tongue is usually found in heavy smokers.
Green color
Another symptom, but of a different disease, will be a green tongue.
The most common diagnosis, which gives a green tongue as one of the symptoms, is the improper functioning of the gastrointestinal tract, in particular the duodenum.
In certain cases, this color of the tongue appears when there is a problem with the gallbladder, for example, when there is insufficient outflow of bile.
Dark, black color
There are times when the tongue becomes dark and even black. This is a likely indicator of a disease such as acidosis. Acidosis is dehydration associated with problems in the pancreas.
A tongue that is too dark also warns of the development of chronic diseases.
A black tongue indicates abscesses, problems with the spleen, or severe viral infections in the body. In rare cases, a black tongue is a sign of Crohn's disease.
Blue color
A bluish tongue is a sign of lung disease. A blue tongue may indicate problems with the kidneys.
A blue or dark gray tongue indicates abdominal diseases, in particular, a purulent abscess of the abdominal cavity. If, in addition to the strange color of the tongue, there are symptoms such as abdominal pain, fluctuations in body temperature, then it is best to call a doctor or go to the hospital.
Brown
A brown tongue may indicate bleeding in the mouth. When plaque of this color appears, diseases of the liver, gallbladder, and pancreas are often diagnosed.
A brown tongue is typical for heavy smokers.
Iodine-containing preparations also provoke the appearance of a brown coating on the tongue.
Of red color
Red color is a clear sign of infection or inflammatory process.
A red tongue, for example, is characteristic of feverish colds accompanied by high fever. Inflammation can occur in the gastrointestinal tract and lungs. A dry red tongue is a symptom of inflammation of the gray matter of the brain.
A rich red color can also indicate blood diseases or problems with the cardiovascular system.
Allergy manifests itself in the form of an uneven red color of the tongue.
Raspberry color
By adding a crimson hue to the red color, a specialist can diagnose a sore throat, scarlet fever or pneumonia. Moreover, with scarlet fever, the tongue becomes shiny and smooth, the papillae become less pronounced.
Causes and mechanisms
Under normal conditions, the tongue appears pale pink with clearly visible papillae. It is soft and does not cause any unpleasant sensations when moving. The surface must be clean, but a coated tongue can also be a consequence of physiological processes. Therefore, before sounding the alarm, you should familiarize yourself with such conditions. These include:
- Nature of food.
- Seasonal variations.
- Insufficient oral hygiene.
- Hormonal changes in the body.
In the morning, plaque appears due to the fact that during the night, keratinized epithelium of the papillae and food particles accumulate on the back of the tongue, which are decomposed by the microflora present in the oral cavity. It becomes more pronounced in the summer, and in winter it acquires a slightly yellowish tint. Insufficient hygienic care promotes the development of bacteria, so the buildup increases. A similar condition can also occur during hormonal surges, for example, in children with puberty or during pregnancy. Only this plaque is insignificant, mostly white, easily removed and the papillae are always visible through it.
Another situation arises if the causes of a coated tongue are associated with pathological processes. Plaque becomes a sign of various health problems. Among them it is necessary to highlight the following conditions:
- Stomatitis.
- Infectious diseases: tonsillitis, scarlet fever, whooping cough, diphtheria, cholera.
- Gastrointestinal diseases: gastritis, peptic ulcer, pancreatitis and cholecystitis, colitis, dysbacteriosis.
- Renal pathology: acute and chronic failure.
- Anemia.
- Radiation sickness.
In addition, plaque on the tongue occurs in heavy smokers and alcohol abusers. And in a child it can appear even with a common cold or other respiratory disease, as a result of helminthic infestation or giardiasis. We can say that a coated tongue becomes a sign of infectious, inflammatory or metabolic processes that affect the condition of the oral mucosa.
When the tongue is covered with a white coating, the reasons can be very diverse: from completely harmless to pathological.
Read also: White spot under the tongue
In the diagnostic process, very important importance is given to the initial examination of the patient. First, the doctor identifies complaints, focusing not only on the main ones, but also on additional ones, which at first glance do not seem to be related to a coating on the tongue. But a detailed analysis allows us to understand many cause-and-effect relationships. Next, an examination of the oral cavity is performed, during which the following plaque characteristics are assessed:
- Color: white, gray, yellowish, brown, green and even black.
- Thickness: thin or thick.
- Consistency: wet or dry, curd-like or fatty.
- Location: only in certain areas (local) or covers the entire surface (diffuse).
- Can be removed well (soft) or poorly (dense).
You should pay attention to the mucous membrane under the plaque layer. It may have a normal structure and color, but sometimes it becomes inflamed or trophically altered (smoothed papillae). The tongue itself can change shape and appearance, and acquire teeth marks on the sides. During the examination, the condition of the mucous membrane of the oral cavity, tonsils, and the back wall of the pharynx is assessed. The doctor immediately understands whether there is a foreign odor from the mouth and how freely nasal breathing is. A physical examination includes identifying any symptoms likely associated with plaque.
White plaque in the mouth and tongue often appears due to stomatitis. It is caused by bacterial, viral flora or fungi. In the latter case, the disease is called candidiasis, but many are familiar with it under the name thrush. It often affects young children because their saliva does not contain enough antimicrobial substances.
Fungal stomatitis first manifests itself as redness of the oral mucosa. After a couple of days, a white, cheesy coating forms on the tongue, which soon spreads to other areas: cheeks, palate, lips. “Sticks” appear in the corners of the mouth. Subsequently, small wounds appear at the site of inflammation. Herpetic stomatitis is characterized by blistering rashes with transparent contents. In the erosive-ulcerative form of the disease, the mucous membrane is covered with a thick gray-green coating, with deep bleeding defects underneath. The mouth emits a putrid odor, the tongue swells, and teeth marks appear on it.
With severe stomatitis, difficulties arise when chewing food, appetite decreases, the child becomes capricious and often refuses to breastfeed. Regional lymph nodes enlarge, and body temperature may also increase. In adulthood, complaints include burning, dryness, pain, and decreased sense of taste.
Infectious diseases

Many infectious diseases are accompanied by a coated tongue. For each pathology, the plaque is different, it has its own characteristics:
- Scarlet fever: white-gray, appearing from the first day, but disappearing from 3–5 days; sharply enlarged papillae (“crimson tongue”) are visible.
- Diphtheria: grayish dense films on the tonsils, palate and root of the tongue, difficult to remove, underneath there is a bright red mucous membrane.
- Whooping cough: whitish-yellow, small ulcerations, bad breath.
- Cholera: dark in color, even black, dry tongue (a consequence of severe dehydration).
Any infection is accompanied by signs of intoxication, which include fever, weakness and malaise, headaches, and loss of appetite. Catarrhal symptoms include sore throat, runny nose, and cough. With diphtheria, there is a real danger of asphyxia due to the covering of the larynx with films. If the disease affects the gastrointestinal tract (dysentery, cholera), then the complaints are accompanied by nausea and vomiting, diarrhea (from scanty to profuse loose stools). Severe dehydration causes hypovolemic shock - blood pressure decreases, pulse increases, and consciousness is depressed. This condition poses a real threat to life.
Infectious diseases, especially children's ones, are often accompanied by a coated tongue.
Pathology of the gastrointestinal tract

It is not for nothing that the tongue is called the mirror of the digestive tract. Its appearance can say a lot about the condition of the stomach and intestines. If the tongue is covered with a white coating, then you should wonder if everything is okay with these organs. The cause most often is inflammatory processes, the nature and localization of which determines the picture in the oral cavity, including the type of plaque:
- Acute gastritis: thick grayish with mucus, covering the entire back of the tongue, except for the tip and sides; dry mouth, sour taste.
- Chronic gastritis: white-yellow in the root and back of the back; the tongue is swollen, sometimes with deep furrows and atrophic papillae (“lacquered”).
- Peptic ulcer: grayish-white in the posterior parts of the tongue, difficult to remove.
- Enterocolitis: gray-yellow, dense.
- Hepatitis and cholecystitis: yellow-brown in color, in the back or anterior regions; bitter taste in the mouth.
- Pancreatitis: grayish-yellow with desquamated epithelium and hypertrophy of the papillae.
Dyspeptic manifestations will be an obligatory component of diseases of the digestive system. These include decreased appetite, nausea and vomiting, flatulence, constipation and diarrhea. Pain often occurs in various parts of the abdomen: in the epigastrium, right and left hypochondrium, periumbilical or iliac zone.
Other diseases
When a patient has a white coated tongue, all possible causes should be considered. They can also be diseases with metabolic or immune disorders. For example, with renal pathology with functional failure, uremic intoxication develops, so the tongue is abundantly covered with a grayish-white coating. When dehydrated due to non-infectious diseases, its color changes to black. Iron and B12 deficiency anemia are accompanied by smoothness of the papillae and deterioration of taste sensitivity. And radiation exposure provokes thickening of the tongue and trophic changes in it: cracks, ulcers, necrosis.
Dysbacteriosis of the oral cavity
In the human oral cavity there are many microorganisms (aerobes, obligate and facultative anaerobes, gram-positive and gram-negative bacteria), which coexist quite peacefully if they are in a certain ratio.
Violation of the quantitative balance leads to the development of oral dysbiosis. One of the most common causes of the disease is the irrational use of antibiotics. Dysbacteriosis of the oral cavity is manifested by inflammation of the mucous membrane, which can lead to the development of stomatitis, glossitis, and bacterial tonsillitis.
Reasons for the development of oral dysbiosis
As a rule, oral dysbiosis develops due to the proliferation of yeast-like fungi Candida albicans. These fungi have an adhesive ability to the epithelial cells of the oral mucosa, and the presence of carious cavities in teeth creates conditions for their long-term existence.
With prolonged antibiotic therapy or immunodeficiency, the obligate microflora that suppresses the development of fungi dies due to which candidiasis develops. Proteases, neuraminidases and other enzymes synthesized by fungi play an important role in pathogenesis.
Yeast fungi attach to the epithelial cells of the oral mucosa, and sucrose, glucose, maltose and other carbohydrates further increase adhesion activity.
The strength of attachment (adhesiveness) of the fungus determines its ability to spread. For example, C.
albicans attaches to epithelial cells 1.5 times faster than other species, and the more antibiotics a person takes, the stronger the adhesion.
The yeast-like fungus destroys tooth enamel and “settles” in carious cavities and further contributes to the development of fungal stomatitis and tonsillitis. Lactic acid produced by lactobacilli prevents the proliferation of yeast-like fungi, so microorganisms cannot multiply uncontrollably.
However, they are given this opportunity if a person takes antibiotics (especially broad-spectrum antibiotics) or suffers from immunodeficiency conditions. Candidiasis can cause local lesions of the oral cavity or provoke multiple lesions of internal organs (generalized candidiasis).
The development of oral dysbiosis can be caused by:
- intestinal infections;
- chronic inflammatory diseases of the gastrointestinal tract;
- a diet limiting the consumption of animal protein;
- lack of vitamins;
- allergic diseases;
- use of medications (hormonal contraceptives, steroids, antiviral drugs);
- smoking and drinking alcohol.
To confirm the diagnosis, bacteriological tests are performed:
Dysbacteriosis in pregnant women
- bacterial culture of saliva or scrapings from the gums. The analysis makes it possible to determine the degree of contamination of the oral cavity with pathogenic microorganisms;
- urease test. Reveals the ratio of urease and lysozyme (if the indicator is more than one, then this indicates the development of dysbacteriosis);
- Gram staining. The quantitative ratio of gram-positive and gram-negative microbes is checked;
- determining the amount of bacteria in exhaled air and comparing the indicator with a smear taken from the oral cavity.
Signs of oral dysbiosis
Bacteriosis of the oral cavity proceeds relatively slowly; its development is divided into three stages:
- Compensation. There is a slight increase in pathogenic microflora. If the body's immune defense is sufficient, the disease does not progress. The only sign of pathology is bad breath;
- Subcompensations. The disease progresses as the number of harmful microbes increases. Symptoms of dysbacteriosis at this stage are more pronounced (burning and dry mouth, a noticeable coating on the tongue, bad breath, discolored mucous membrane);
- Decompensation. Local immunity is reduced, so there are no obstacles to the development of pathogenic flora, which makes up the majority of the oral microflora. Lesions appear on the mucous membrane, bleeding gums, inflammation of the tonsils and soft palate are noted, and a putrid odor from the mouth is characteristic.
As the pathology progresses, inflammatory and dystrophic processes spread to the throat
If left untreated, oral dysbiosis manifests itself:
- inflammation of the gums and mucous membrane;
- the presence of plaque on the tongue and teeth;
- gingivitis (bleeding gums);
- the occurrence of ulcers, erosions on the mucous membrane and tongue;
- swelling, redness and soreness;
- putrid odor, unpleasant taste in the mouth;
- dry facial skin, cracks in the corners of the mouth.
In some cases, there are no symptoms of oral dysbiosis, and the disease becomes chronic, leading to frequent ARIs. Plaque or ulcers are clearly visible in photographs of the patients’ oral cavity, so you can suspect a pathology simply by looking at the tongue.
Treatment
Depending on the stage of the disease and its causative agent, therapy is prescribed, which may include:
- sanitation of the oral cavity. Plaque and tartar must be removed from the teeth, and carious cavities must also be filled, since they act as a breeding ground for pathogenic bacteria;
- taking antiseptics or antimycotics to eliminate pathogenic microorganisms;
- taking immunostimulants. These drugs help increase local and systemic immunity;
- consumption of vitamins. Vitamins A, E, C help restore the oral mucosa. In addition, with pathology, the absorption of nutrients is impaired, and vitamin complexes help to avoid a lack of vitamins and minerals.
The causative agents of disease are most often fungi of the genus Candida, Escherichia coli, Proteus, and enterococci.
Depending on the causative agent of the disease, antibacterial or antimycotic drugs are prescribed. To destroy bacterial microflora in the oral cavity, the following can be used:
- "Tantum Verde". It has an antiseptic and anti-inflammatory effect and also reduces pain. The active substance is benzydamine hydrochloride. Available in the form of a spray, lozenges, and solution. You need to take the product every three hours;
- "Orasept." The active ingredients are phenol (fungicidal and antifungal action) and glycerin (relieves irritation). Available in spray form;
- "Yox." Contains povidone-iodine, allantoin, levomenthol, due to which it has antiseptic and anti-inflammatory properties. The drug is active against gram-positive and gram-negative cocci, protozoan viruses, and yeast. Available in solution and spray;
- "Chlorhexidine." Has a bactericidal effect. So, rinse the mouth with a 0.5% solution for 30 seconds, then spit out the liquid.
If dysbiosis of the oral cavity has developed due to a fungus, then the drug “Candide” is prescribed, the active component of which is clotrimazole, which has an antimycotic and antibacterial effect. The product destroys mold and yeast-like fungi, gram-positive and gram-negative bacteria. The solution is used to wipe the affected areas of the mucous membrane.
In severe cases of the disease, the doctor prescribes narrow-spectrum drugs that are aimed at combating a specific type of bacteria.
So, when staphylococcus is detected, macrolides or pyobacteriophage (Josamycin, Clarithromycin) are prescribed, enterococci are destroyed with macrolides, penicillins, nitrofurans (Furazolidone), drugs nalidixic acid, sulfonamides will get rid of Proteus, and for Pseudomonas aeruginosa, Gentomycin is indicated.
Also, treatment of oral dysbiosis involves the use of prebiotics and probiotics. Prebiotics stimulate the development of beneficial microflora. They are not digested or absorbed in the stomach and intestines, but are broken down by the microflora of the large intestine, that is, they are food for bifidobacteria and lactobacilli.
Prebiotics include di- and trisaccharides, oligo- and polysaccharides, amino acids, peptides, polyhydric alcohols, enzymes, fatty acids, antioxidants and others.
Biotics can be naturally or artificially synthesized
Natural prebiotics are found in cereals and bran, seaweed, vegetables, fruits and dried fruits, leafy greens, and dairy products (lactulose and lactose). They love beneficial bacteria and inulin contained in garlic, onions, bananas, chicory, and wheat. Synthesized prebiotics can be purchased at the pharmacy (Duphalac, Normaze, Laktofiltrum).
Probiotics contain live beneficial bacteria that prevent the development of pathogenic microflora. Pharmaceutical preparations may contain one strain of bacteria (lactobacteria, bifidobacteria) or several types of microorganisms that enhance each other’s effects. Probiotics include “Acilact”, “Bifidumbacterin”, “Lactobacterin”, “Linex”, “Polibacterin”, “Hilak forte”.
Products are available in capsules, tablets, powders, suspensions, and suppositories. The duration of their intake varies depending on the generation of the probiotic (from 4 weeks to 7 days). “BioGaia” is effective for oral dysbacteriosis. This medicine contains lactobacilli. It is used sublingually (placed under the tongue or chewed), which means it has only a local effect.
Live microcultures are also found in kefir, yoghurt, curdled milk, kumiss, cottage cheese, buttermilk, quick-ripening cheese, sauerkraut and other drinks prepared using starter culture or enzymes.
More than 10 types of beneficial bacteria are involved in the production of kefir; fermented baked milk and yogurt contain mesophilic and thermophilic bacteria, acidophilus bacilli; 1 gram of cheese accounts for almost 100 million.
beneficial bacteria.
When treating oral dysbiosis, it is necessary not only to increase the consumption of foods containing beneficial probiotics and prebiotics, but also to exclude fast carbohydrates, fast food, fatty, fried and salty foods from the diet.
The more sweets a person eats, the more yeast-like fungi attach to epithelial cells, which means it is more difficult to get rid of them
Folk remedies will help get rid of oral dysbiosis:
- homemade curdled milk. You need to boil a liter of milk and add a few pieces of dried black bread to it, leave to infuse in a warm place for a day. Use yogurt within a week;
- strawberries Berries stimulate salivation, which leads to the release of substances that destroy pathogenic microorganisms. Thus, conditions are created for the reproduction of obligate microflora;
- bloodroot. Potentilla decoction has soothing, anti-inflammatory and antiseptic properties. A spoonful of the dried plant is poured with two glasses of boiling water and boiled for half an hour. You need to drink the decoction twice a day before meals.
To prevent the development of dysbiosis, it is necessary to monitor oral hygiene, adhere to a healthy diet, and promptly treat gastrointestinal diseases.
Since doctors consider medication use to be the main factor in the development of pathology, the use of antibiotics, hormonal and antiviral drugs should be monitored by the attending physician.
If drug therapy is long-term, then prophylactic administration of drugs based on bifidobacteria and lactobacilli is advisable.
Source: https://vrbiz.ru/diagnostika/disbakterioz-polosti-rta
Additional diagnostics
Considering the variety of factors that can initiate changes in the oral cavity, it is possible to say exactly why the tongue is covered with a white coating only after a comprehensive examination. It includes various laboratory and instrumental tools:
- Complete blood count (erythrocytes, hemoglobin, leukocytes, ESR).
- Blood biochemistry (proteinogram, liver and kidney tests, antibodies to infections, serum iron).
- Oral smear (microscopy, bacterial culture, PCR).
- General (coprogram) and bacteriological analysis of stool.
- Ultrasound of internal organs.
- Gastroscopy.
It is very important to carry out a differential diagnosis of probable conditions, since it is difficult to say anything based only on changes in the oral cavity.
Diagnostic measures consist of laboratory and instrumental control methods to determine the nature of the disorders.
A disease can be treated only when its cause is clearly established. And all therapeutic measures should be aimed at eliminating it. You should not try to simply remove plaque from the tongue, since it is just a symptom of deeper disorders. If local inflammatory disorders (stomatitis) are detected, then treatment will consist of rinsing, washing and applications with antiseptics and antimicrobials (Givalex, furacillin, Iodinol). If an infant has a coated tongue, you can even use a simple solution of soda, a decoction of chamomile or calendula.
Infectious diseases may require specific treatment with antibiotics and antivirals, taking into account the sensitivity of the pathogen to them. For pathology of the digestive tract, antisecretory drugs (Nolpaza, Omez), enzymes (Mezim, Creon), prokinetics (Motilium), choleretic drugs (Hofitol) are needed. Inflammatory processes are suppressed by non-steroidal drugs; in some cases, infusion and detoxification therapy is required. Each disease is treated differently.
Prevention

To keep your tongue always clean, you should first of all pay increased attention to oral hygiene. It's not just your teeth that require care. The tongue should also be cleaned daily of physiological plaque (with the ribbed surface on the back of the toothbrush). And if any alarming symptoms appear, you should immediately consult a doctor without expecting their further progression.
A coated tongue is a symptom of many local and systemic diseases. There are also quite banal reasons for the appearance of plaque. But to rule out dangerous conditions, it is best to consult a doctor. A specialist will conduct a study and tell you why your tongue is coated and how to deal with it.









