Etiology
There can be many etiological factors that can cause the formation of such an anomaly. Quite often, the pathology is diagnosed in a newborn child, which means that the disease was formed in the womb.
Congenital deformity occurs due to abnormal intrauterine development. Provoking factors may include:
- heredity;
- Improper lifestyle of a woman during pregnancy - consumption of nicotine, alcohol, excessive activity.
The disease can also be an acquired disease, which means that the process of development of a deformed organ begins not at birth, but during life. The following factors may be the reasons:
- inflammation of the bile ducts;
- the appearance of stones in the organ or its canals;
- excessive food consumption;
- frequent strain on the abdominal muscles;
- formation of adhesions;
- weak diaphragm;
- gastrointestinal diseases;
- biliary dyskinesia;
- tumors of malignant or benign origin.
Symptoms
Depending on the type of degree of deformation of the gallbladder, the child experiences different signs of the disease. Quite often, pathology immediately affects the functioning of the gastrointestinal tract, which means that abdominal pain, abnormal stool, and dyspeptic disorders immediately appear. The pain syndrome is felt under the right rib and can spread to the shoulder blade, collarbone, sternum, intestines and spine.
With the slow development of the disease, the child has almost invisible signs of deformation of the gallbladder. Symptoms are hardly felt, but the pathological process can be identified by the following indicators:
- loss of appetite;
- light shade of stool;
- fatty elements in stones;
- gradual weight loss.
If, with the development of pathology, the neck of the bladder is twisted in a child, this can provoke necrosis of the organ area and the entry of bile into the abdominal cavity. As the complicated form progresses, the little patient is overcome by severe pain under the left rib or throughout the entire abdominal area. The temperature may rise, nausea, weakness may appear, and the abdomen may increase in volume. During palpation of the inflamed area, the small patient feels severe pain of a paroxysmal nature. In this case, you need urgent doctor's help.
Diagnostics
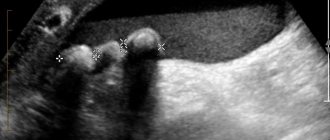
During an examination of the condition of the gallbladder, the doctor interviews the patient or his parents for the presence of other pathologies and the manifestation of symptoms. After a physical examination, the patient is prescribed an instrumental examination - ultrasound of the abdominal cavity.
Ultrasound examination is the most informative diagnostic method, which allows you to determine the deformation of an organ and the compaction of its walls. Also, during the establishment of the diagnosis and the causes of the anomaly, the computed tomography method is often used.
When examining the biliary organs, it is important for the doctor to pay attention to the size, location, shape of the organ, its movement during inhalation and exhalation, the outline of the bladder and liver. It is also important to determine the density and structure of the shell, the degree of filling and release of the organ.
When the gallbladder is inflamed, the patient is diagnosed with the following echo signs of the disease:
- the walls are thickened and compacted;
- an inflection has been identified;
- wall retraction;
- Violations of the shape and outline of the organ are significantly expressed.
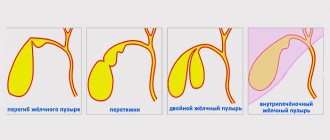
Anomalies of gallbladder development
An abnormal state of the gallbladder was noted in 28% of cases of pathological changes in the biliary tract. According to the standard classification of the disease, there is one type of anomaly acquired during intrauterine growth - complete absence or underdevelopment. Depending on the nature, location of the form and other criteria, subtypes are distinguished - agenesis, aplasia, hypoplasia and other abnormal features in the anatomy of this organ. The main reason for their occurrence is disruptions during intrauterine development.
The classification is different depending on the nature, location, shape and other criteria of the gallstone.
Treatment
In treating the disease, doctors try to normalize the process of bile outflow, eliminate attacks of pain and inflammation. To achieve these goals, the patient must adhere to the following recommendations:
- bed rest during exacerbation;
- compliance with the rules of dietary table No. 5;
- taking antispasmodics and painkillers;
- antibacterial therapy;
- detoxification treatment;
- use of choleretic drugs;
- increasing immunity;
- undergoing a course of physiotherapy;
- herbal therapy at the time of remission and subsidence of symptoms.
Also, physical therapy is important for the effective outflow of bile. Thanks to exercise therapy, the chance of exacerbations and stones is reduced. However, do not forget that excessive exercise can only aggravate the situation.
If a child is diagnosed with a congenital anomaly of the bladder and there are no manifestations, then treatment with these methods is not carried out. The patient continues to be monitored and preventive measures are taken to maintain normal functioning of the organ.
Increasingly recently, specialists are diagnosing abnormal forms of the gallbladder in children of various ages - according to statistics, this is 25% of the younger generation. The most common disorders are observed in adolescents - against the background of rapid physical development, stagnation of bile for a long time becomes the cause of acute inflammatory processes, up to the formation of stones and sand in the ducts that remove bile and the gallbladder. The achievements of modern medicine help to cope with most diseases, while the main task of parents remains the timely detection of the disease and seeking help from specialists. After all, treatment cannot be delayed, much less self-medication.
Drug treatment
No conservative method of therapy can eliminate a violation of the shape of the gallbladder, regardless of whether it is congenital or acquired. All non-surgical techniques are aimed at relieving symptoms.
For this purpose, use:
- Following a diet with limited consumption of fatty, fried and spicy foods, and alcoholic beverages.
- Choleretic drugs (Alohol, Holiver, Hofitol).
- Antispasmodics (No-shpa, Baralgin).
- With the development of acute cholecystitis - antibacterial agents.
People with gallbladder pathology benefit greatly from normalizing and maintaining a healthy weight through proper nutrition and moderate exercise.
For diseases of the gallbladder, doctors advise excluding fatty meats and rich broths from the diet. You cannot smoke or fry foods; it is better to use steam and stewing for cooking.
In case of gallbladder diseases, it is necessary to take into account not only the menu, but also the food consumption schedule. It is advisable to eat at least 5-6 times a day. Portions should be small. A few hours before bedtime, it is better to refuse food altogether.
- To remove the cause of the disease, doctors prescribe etiotropic treatment.
This may include antibiotics and/or surgery (depending on the type of disease).
- To restore normal functioning of the gallbladder, pathogenetic treatment is prescribed.
Depending on the problem, these may be antispasmodics and/or enzymatic agents like Mezim.
- To reduce the intensity or completely eliminate the symptoms of diseases, anti-inflammatory drugs, painkillers and antispasmodics are prescribed.
This could be No-shpa, Ketanov, Paracetamol and other medications.
Causes of abnormal forms of gall bladder in young children and adolescents
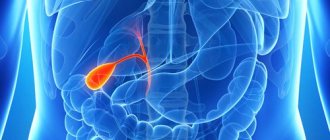
The gallbladder is a complex system, without the normal functioning of which the body can be suppressed, resulting in deterioration in health, decreased activity and other consequences.
So, this organ is a combination of three functional elements: body, neck and fundus. As the child grows, their location relative to each other changes, resulting in deformation - this can be a bend and constriction of the bladder, twisting and bending of the neck, as well as a number of other anomalies.
The causes of this disease are various factors, primarily depending on whether it is a congenital or acquired deformity. To identify the nature of the disease, doctors prescribe an ultrasound examination.
Causes of congenital anomaly
Congenital deformation of the gallbladder can be caused by various negative factors, the impact of which was exerted on the mother’s body during the formation of the child’s digestive organs - this is the first 14 weeks of pregnancy.
Depressing factors include:
- infectious or chronic disease of the expectant mother;
- taking certain medications;
- passive and active forms of smoking;
- consumption of alcoholic beverages.
Causes of acquired anomaly
The most common causes of acquired abnormal forms of the bladder include inflammatory processes occurring directly in the bile ducts and its ducts, as well as inflammation of the gastrointestinal tract. The consequence of inflammation is deformation of the bile ducts - as a result, the outflow of bile becomes difficult and stagnation occurs. It is he who provokes the appearance of cholelithiasis, the onset of inflammatory processes in the gall bladder.
Anomalies of gallbladder development
The gallbladder is a reservoir
bile. In newborns it has a spindle-shaped or cylindrical shape. Its bottom does not protrude from under the edge of the liver. In an adult, the length of the bladder is 8-12 cm. The capacity is equal in adults - 30-65 ml, on average 45 ml. The gallbladder is adjacent to the abdominal wall in the place where the angle formed by the costal arch and the outer edge of the rectus abdominis muscle (Ker's point) is located.
Bile is secreted by the liver continuously, but on its way to the duodenum it meets the sphincter, so it is sent to the gallbladder, where the mucous membrane absorbs water and the bile is concentrated 5 times. From 3 to 4.5 liters of provisional bile is secreted per day; it thickens in the gallbladder. If 40 cm 3 of bile accumulates in the gallbladder, its nerve elements are irritated, the muscles are reflexively excited, and the spiral fold relaxes, as a result of which a portion of bile is released into the duodenum. In the same way, bile is released reflexively if food enters the duodenum.
The right and left hepatic ducts unite at the porta hepatis to form the common hepatic duct. The latter merges with the cystic duct, forming the common bile duct. Various options for the relationship between the cystic and common bile ducts are observed. The cystic duct may cross the common bile duct or be located next to it. Sometimes both ducts flow separately into the duodenum.
The common bile duct in half of the cases connects with the pancreatic duct, forming the hepatopancreatic ampulla, which is located in the major duodenal papilla. Here, a special device is formed that regulates the flow of bile and pancreatic juice into the intestines - the sphincter of the hepatopancreatic ampulla, which continues into the sphincter of the common bile duct and the sphincter of the pancreas. The sphincter of the ampulla consists of interwoven bundles of smooth muscle cells running in a circular, longitudinal and oblique direction, covering the ampulla and the terminal sections of the common bile and pancreatic ducts. In newborns and in the thoracic period, the sphincter of the ampulla is poorly developed and is represented mainly by circular muscles. By 2-4 years, the number of muscle cells in it increases, and it acquires a characteristic structure.
1. Agenesis of the gallbladder
– it is based on damage to the caudal part of the hepatic diverticulum during the 4th week of embryonic development. There are 2 forms:
A) complete – absence of gall bladder and extrahepatic ducts;
B) while maintaining the biliary tract.
2. Gallbladder hypoplasia
– appears in the form of a very small bubble.
3. Dystopia of the gallbladder
– change in the position of the gallbladder. There are several position options:
B) intraperitoneal (syn. vagus gallbladder) - insufficient fixation of the gallbladder to the liver, when it lies completely outside it, is covered on all sides by the peritoneum and has a mesentery, which can cause volvulus of the gallbladder.
D) under the left lobe of the liver,
D) left-sided with the reverse arrangement of organs.
4. Duplication of the gallbladder
- there are several forms:
A) The gallbladder is bilobed - there is a common neck for 2 separate chambers. Drainage can be through a single or double cystic duct.
B) “ductular” gallbladder – true duplication of the gallbladder. At the same time, there are 2 fully formed organs; the cystic ducts independently open into the common bile duct or hepatic ducts.
C) Triplication of the gallbladder - all three organs are located in a common fossa and have a common serous cover.
Studopedia. ru He is not the author of the materials posted. But it provides free use. Is there a copyright violation? Write to us
Laboratory signs of cholestasis:
• increased concentration of conjugated bilirubin in blood serum;
• increased activity of alkaline phosphatase in the blood serum (especially the hepatic isoenzyme);
• increased activity of γ-glutamyl transpeptidase (γ-GTP) in blood serum;
• increased leucine aminopeptidase (LAP) activity in blood serum;
• increased activity of 5#8242;-nucleosidase in blood serum;
• increased concentration of cholesterol in blood serum;
• increased concentration of bile acids in blood serum;
• increased concentration of copper in blood serum;
• increased concentration of urobilinogen in urine. The severity of symptoms can vary significantly across different diseases, from minimal to extremely severe. An additional sign of cholestasis is the presence of thick bile (biliary sludge) in the lumen of the gallbladder. The presence of cholestasis can be reliably confirmed using hepatobiliary scintigraphy: a slowdown in the entry of the radiopharmaceutical into the duodenum is recorded.
In everyday practice, pediatricians most often encounter kinks and constrictions of the gallbladder, which may not have any clinical significance or cause disturbances in the passage of bile. Of particular importance are combinations of kinks that form the so-called S-shaped gallbladder and lead to its dysfunction. Functions of the gallbladder:
• cumulative - accumulation of bile during the interdigestive period;
• concentration - absorption of water;
• reabsorption - reabsorption of amino acids, albumin, inorganic substances;
• contractile - movement of bile along the biliary tract;
• secretory - secretion of mucus, enzymes, electrolytes and
• enzymatic – acceleration of the action of pancreatic lipase;
• hormonal - release of anticholecystokinin;
• regulatory - maintaining a sufficient level of bile components during digestion.
Dysfunctional disorders of the gallbladder and biliary tract in children are a common cause of the development of inflammatory diseases of the biliary system.
Symptoms of abnormal forms of gall bladder in children
The course of the disease can proceed with different priorities of the influence of a certain type of nervous system - parasympathetic or sympathetic, and this changes the signs of the disease and its symptoms.
Experts distinguish two types of disease:
- Hypertonic-hyperkinetic . With this course of the disease, the child complains of paroxysmal severe pain localized in the right hypochondrium. As a rule, they appear as a result of a violation of the diet (overeating), non-compliance with the diet (eating food with a pronounced pungent, sour taste, high level of fat content). Intense and regular physical activity can also cause exacerbation.
- Hypotonic-hypokinetic . During this course, children experience prolonged attacks of mild aching pain, also localized in the right hypochondrium. This condition is accompanied by poor appetite, a bitter taste may appear in the mouth after a night's sleep, belching with an unpleasant taste and nausea may appear.
Regardless of how the disease progresses, during its exacerbation, general symptoms characteristic of intoxication of the body appear:
- weakness;
- nausea;
- increased body temperature;
- body aches;
- less often - vomiting.
The appearance of such symptoms cannot be ignored; it is important to seek help from specialists in a timely manner.
Gallbladder: symptoms of disease
The gallbladder is a pear-shaped organ designed to store bile.
This is a kind of reservoir for the bitter yellow-green liquid that is produced by the liver. The dimensions of the organ are small, the length of the bladder in an adult is approximately 8 cm, and the capacity varies from 40 to 60 cubic meters. see. In children and adults, the gallbladder normally lies on the surface of the liver, in the lower part of the organ, between the right and quadrate lobes. The gallbladder is mobile and can twist, which often leads to necrosis (cessation of the vital activity of cells).
The organ can be doubled; there are also cases of its dystopia, when the bladder takes an unnatural position in the abdominal cavity. There are known cases of intrahepatic location of the gallbladder.
Signs of gallbladder dysfunction are often nonspecific. The patient may experience weakness and general malaise, minor pain in the right side of the chest, nausea, and even a slight increase in body temperature.
People with such symptoms, unfortunately, rarely go to the doctor for help, trying to endure the discomfort in the hope that everything will soon go away on its own. As for the pronounced symptoms of gallbladder diseases, we can distinguish:
- pain;
- signs of digestive disorders;
- rich color of urine;
- clarified feces;
- nausea;
- bitterness in the mouth;
- yellowish color of the skin and sclera;
- decreased appetite.
Main causes and mechanism of disease development
Diseases associated with the gallbladder have different mechanisms of development. And the causes of diseases are most often different.
So cholecystitis is diagnosed as inflammation caused by a variety of microorganisms and a violation of the outflow of bile. The cause may also be helminthic infestation.
Treatment of abnormal forms of the gallbladder in children
Treatment of abnormal forms of gallstones in children, in most cases, is medicinal in nature with parallel adherence to the regimen and diet prescribed by the doctor. Surgical intervention becomes relevant only in rare – very severe cases.
The main goal of doctors is to normalize the processes of bile outflow, relieve pain syndromes and relieve inflammatory processes. An important condition for a speedy recovery is compliance with bed rest.
As symptoms disappear, the child should drink more fluid (with the exception of carbonated drinks and juices in tetra packs). And the food should be strictly dietary in nature, the list of specific products is prescribed by the attending physician (this could be dairy products, cottage cheese, certain fruits, low-fat broths, natural dried fruit compotes, steamed cutlets, etc.).
If pain symptoms recur, the child should take painkillers prescribed by the doctor during meals. It is important to note that in the process of treating gallstone deformation in children and especially newborns, it is not recommended to take antibiotics, choleretic drugs, vitamins of groups C, B, A and E. If they are prescribed, then strictly as prescribed by the attending physician.
Anomaly in the shape of the gallbladder in a child: ICD-10 code, signs, diagnosis and treatment
In approximately a quarter of cases of biliary pathologies, patients exhibit abnormal changes in the biliary tract.
In accordance with the standard classification of this pathology, a special form of anomaly is identified, which is acquired during the process of intrauterine development - underdevelopment or complete absence of an organ. What are gallstone anomalies, why are they dangerous and is it possible to somehow cure them?
Disease code according to ICD-10
In the international classification of diseases, gallbladder anomalies are assigned code Q44.
Classification
In fact, the gallbladder is a hollow, pear-shaped organic structure located just below the right hepatic lobe. The gallbladder is firmly attached to the liver by the upper hepatic surface.
In healthy adult patients, the bile duct usually measures 2.5x7-10 cm. This organ contains about 35 ml of bile juice, but if there is a blockage of the bile ducts, then its amount can be 300 ml.
Gallbladder anomalies are conventionally classified into quantitative, anomalies of shape, size and location. Each classification has its own varieties and characteristics, therefore they must be analyzed separately.
Quantitative
Anomalies of a quantitative nature are divided into conditions in which the gall bladder may be absent, underdeveloped, or instead of one organ, the child will have two or even more gall bladders.
In addition, anomalies include various kinds of constrictions, kinks and diverticula, dwarf or giant sizes or abnormal location of the organ.
Absence
In congenital absence, several anomalies may occur:
- Aplasia - when there is only a non-functional bile primordium, although there are fully functional bile ducts;
- Agnesia – when extrahepatic channels are completely absent, and the bladder itself is not formed.
In approximately a quarter to half of cases, the consequence of such an anomaly is the formation of stones, overload of the smooth muscle tissue of the duodenal papilla, or pathological expansion of the bile duct, which connects the duodenum to the bile duct.
Underdevelopment
Underdevelopment of the bladder is accompanied by weak peristaltic functions, which provoke the rapid formation of stones. Underdevelopment manifests itself in various forms - aplasia, agnesia or hypoplasia, which were described above.
Doubling
Gallbladder duplication is usually accompanied by underdevelopment of the organ, because it is quite small in size. Functional weakness provokes frequent gallbladder diseases such as dropsy, stone-forming or inflammatory processes.
There are different variations of doubling:
- Bilobedity – this condition is the presence of a common cervical canal in two separate gall bladder chambers;
- Multi-chamber - when there is a complete or partial separation of the bladder from its main body.
A large number of
Such anomalies can also manifest themselves in several forms:
- Triplication - involves the formation of three organs, completely independent, located in a single cavity and having one serous membrane. Treatment involves drainage with the insertion of a bile drainage tube in the formed ductal canals;
- Ductularity - with such an anomaly, a true doubling of the bladder is observed, when there are two fully functioning bile ducts with working ducts, which independently enter the common hepatic and bile canal.
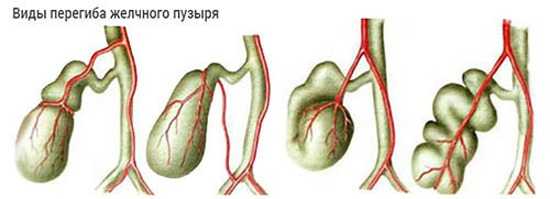
Abnormalities in the shape of the gallbladder
Anomalies of shape are formed due to diverticulum, constrictions or kinks of the neck and/or body of the gallbladder, which causes deformation of the organ.
Kinks
When kinked, a disruption of functionality occurs along the longitudinal axis, in which the bile duct is formed in the form of a cochlea, and all its functioning parts are secured by adhesions to the duodenum. Various options for securing the organ are possible; sometimes it is attached to the colon with adhesive fibers.
Inflections are formed in different types - true or functional. In the true form, therapeutic intervention is required, but in the functional form, the problem is eliminated on its own.
When constriction occurs, there is a narrowing of the bile body along its entire circumference or in some areas. Congenital anomalies of this kind are formed against the background of disproportionate development of the organ and its bed.
This form of anomaly causes disruption of bile outflow in the system, which provokes the development of stagnation. Such disruptions cause dystrophic changes in the walls of the gallbladder and also disrupt contractile functions such as hypotension.
If the anomalies are of genetic origin, then the shape anomaly cannot be changed. If the constriction was caused by inflammation of the serous membrane, then the gall bladder can still straighten out.
Diverticulum
Diverticulum is characterized by a protrusion of the wall of the gallbladder in the form of a bag, since the organ does not have an elastic frame. An anomaly is formed in the bubble due to the lack of its general performance.
Characteristic signs of diverticulum are acute, severe pain caused by bile stasis.
Also, diverticulum is often accompanied by stone-forming and inflammatory processes. In addition, with abnormalities, the gall bladder can take on a spherical or s-shaped shape or the appearance of a boomerang.
Provisions
Positional anomalies include dystopia, in which the bubble can be localized to the left of the liver, behind it, inside the hepatic parenchyma, or wandering around the abdominal space.
If gallstone fixation is completely absent, the risk of kinks or volvulus increases as much as possible. In such a situation, emergency surgical intervention is extremely important, otherwise death is almost inevitable.
Sizes
Anomalies in size suggest abnormally large or, conversely, reduced size of the organ. This includes conditions such as dwarf and giant, as well as hypoplastic gallbladder.
Giant
This anomaly is characterized by a uniform increase in all parts of the bile duct, except for the ducts. The internal fluid is homogeneous and additional thickening of the walls of the bladder is not required.
Dwarf
With an anomaly such as a dwarf gallbladder, a uniform decrease in the size of the organ is observed, while its functionality and structural structure are completely preserved.
Hypoplasia
With hypoplasia, the gall bladder is excessively reduced in size or simply underdeveloped. Such an anomaly can affect the entire organ or some of its parts.
Typically, dwarf or giant gallstones do not require surgical intervention, however, with a hyperplastic anomaly, which often causes inflammatory complications, surgery is necessary.
Various gallbladder abnormalities often disrupt bile flow, inhibiting the main functions of the organ.
Bile stagnation provokes the development of dystrophic changes in the walls of the organ, which begins to increase in size, and its contractile abilities deteriorate. Stagnation of bile also provokes the development of cholecystitis and stone formation.
Diagnosis of pathologies
Typically diagnosis includes:
If necessary, the patient is referred to specialized specialists, and at the same time, family history and other pathological factors are determined.
Treatment
Therapy for biliary anomalies, as a rule, is a complex of measures, including diet therapy, drug treatment, physiotherapeutic procedures and surgery.
- Drug therapy involves taking drugs from the group of antispasmodics (Baralgin, Spazmalgon, No-Shpa, etc.), which eliminate the main symptoms, as well as a six-month course of choleretic drugs like Flamin, Hofitol, Alochol or Holiver; if cholecystitis develops, then antibiotic therapy is indicated.
- Diet therapy is based on the principles of fractional nutrition; any stress on the gastrointestinal tract is contraindicated, so the diet should be gentle. A fifth table is recommended.
- Sometimes you can use folk remedies like wormwood decoction, etc. Rosehip and corn silk, tansy and immortelle, calendula and St. John's wort also have choleretic properties.
- Physiotherapy involves sessions of electrophoresis or paraffin applications.
- In case of dysfunction, chronic inflammation, biliary polyposis or the formation of sediment in the bladder, the patient undergoes surgery .
Gallbladder abnormalities should be treated if they increase the risk of complications or interfere with the patient's ability to live a normal life. Removal of the gallbladder is carried out only in extreme cases, when conservative therapeutic measures do not give the desired result, or there is a real threat to the patient’s life.
Source: https://gidmed.com/gastroenterologiya/zabolevaniya-gastro/zhelchnyj-puzyr-i-zhelchevyvodyashhie-puti/anomaliya-zhelchnogo-puzyrya.html
Gallbladder is normal
In a healthy person, this organ is usually pear-shaped or funnel-shaped. In young children, the gallbladder is shaped like a spindle. The shape gradually changes according to age. The structure of the gallbladder is divided into: bottom, body and neck.
The main function of the organ is the accumulation of bile. When there is a need to break down fatty foods, the walls of the bladder contract. Through the bile duct system, bile enters the duodenum through the sphincter of Oddi, located in its wall.
How are gallbladder abnormalities diagnosed?
The most accurate method for diagnosing pathological changes in the structure and shape of this organ of the digestive system is ultrasound, which allows you to obtain data on the condition, structural features and functionality of the walls and ducts. Ultrasound can be general or with stress, when data is taken after patients consume a choleretic breakfast. If the system with ducts is not clearly visualized on ultrasound, patients undergo CT and MRI.
Agenesis and aplasia are diagnosed by cholegraphy, radiocholecystography and dynamic scintigraphy to analyze the ability to accumulate bile. The laparoscopic method is used in rare cases. It is usually used to diagnose other pathologies in nearby organs or concomitant diseases with bladder abnormalities.
Types of deformation
A bend in the gallbladder in children may not be limited only to the area of the organ, but also affect the system of excretory ducts. Areas where kinks occur:
- Bottom;
- Body;
- Neck:
- Cystic duct.
Deformation can affect one anatomical area or several at once. For example, a child may have a double bend in the gallbladder. In such cases, the organ takes on an S-shape. More than two kinks are extremely rare.
Among the relatively commonly found deformities is the U-shaped gallbladder. The shape resembles a boomerang. Another option is the “Phrygian cap” configuration. It occurs when the fundus bends toward the body of the gallbladder.
The condition may be transient. Labile bending of the gallbladder in a child is characterized by reversibility and a possible change in location. If a persistent change in the shape of the bubble is observed, they speak of a fixed inflection. A transient form can become permanent over time.

Causes
A child may have kinks in the gallbladder of a congenital or acquired nature. Often the etiology is combined. For example, when a bend occurs in a child who is initially predisposed to it due to the action of external factors. The patient’s management tactics depend on the reason for the change in organ configuration.
Congenital deformities
The pathological substrate is often “failures” in development at the 5th week of embryogenesis. During this period, the formation of the organs of the biliary system occurs: the liver, gall bladder and duct system. Provoking factors are numerous and not fully understood. Most often, gross congenital deformities are fixed and combined with other anatomical anomalies.
Functional inflections in healthy children
A bent gallbladder in a baby is not always a sign of an abnormality in intrauterine development. This anatomical feature can occur in children during the period of active growth and is even considered a type of normal. It is caused by a change in the location of organs relative to each other, an increase in the workload on the gallbladder. This is especially often observed when switching from breastfeeding to eating rougher food.
Functional bending of the gallbladder in a small child is characterized by lability. It can repeatedly change location depending on the position of the body, and disappear temporarily (for example, if the child stands up). With age, this bend usually disappears completely and does not lead to gallbladder diseases.
Acquired bends of the gallbladder
They are of a secondary nature. They arise under the influence of external factors. Among them:
- Errors in nutrition. Both overeating and fasting have the same negative effects.
- Obesity. The accumulation of fat around the abdominal organs leads to their displacement relative to each other. The position of the gallbladder also changes.
- Physical inactivity. For example, if a child often spends time sitting at the computer. The bend is functional in nature and disappears when the body position changes.
- Excessive physical activity. We are talking about excessive sports training, lifting loads whose weight does not correspond to age.
- Compression by other organs. For example, in pathologies accompanied by a pronounced enlargement of the liver or right kidney.
- Diseases of the biliary system. For example, adhesions during chronic inflammation are one of the causes of constrictions on the gallbladder in a child, narrowing the lumen of the organ.
- Prolapse of internal organs. According to a similar mechanism, functional excesses of the gallbladder occur in children who have suddenly and significantly lost weight.
What is gallbladder hypoplasia
AGENESIS, APLASIA AND HYPOPLASIA OF THE GALL BLADDER AND BIL DUCT are malformations of embryonic development, manifested in the complete absence or underdevelopment of the gallbladder and bile ducts.
Agenesis and aplasia of the gallbladder are an extremely rare developmental anomaly (occurs 1 time in 500,000 births) and is a pathology incompatible with life (although the literature describes a case of the formation of a gallbladder in a newborn child in the case of normal development of the bile ducts). Much more common is hypoplasia of the gallbladder with complete or partial absence of bile ducts - atresia or their aplasia. The development of this defect is due to the characteristics of embryonic development. Violation of the fusion and process of recanalization of the ducts leads to the development of aplasia and atresia of the biliary system. Intrauterine pathological processes in the liver (congenital hepatitis, etc.) may have a certain significance.
Manifestations of gallbladder hypoplasia and bile duct atresia are typical. A child is born with jaundice, or it develops in the first 2-3 days after birth. Characterized by a gradual increase in jaundice. The stool has been discolored since birth. The urine is the color of dark beer. After 2-3 weeks from birth, an enlargement of the liver and then the spleen is noted. Noteworthy is the increase in the size of the abdomen, the expansion of the network of saphenous veins of the abdominal wall, later hemorrhagic manifestations occur, and ascites develops. children die from biliary cirrhosis 6-9 months after birth.
Diagnosis of congenital anomalies of the biliary system presents significant difficulties due to the identity of the clinical manifestations of a number of diseases accompanied by prolonged jaundice. Differential diagnosis is carried out with prolonged physiological jaundice of the newborn, conflict hemolytic jaundice, generalized cytomegaly, toxoplasmosis. syphilis. blockage of the bile ducts by mucus plugs, congenital giant cell hepatitis. With prolonged physiological jaundice of a newborn, the stool is usually excessively colored, the urine is dark, the jaundice tends to decrease, the free fraction of bilirubin predominates in the blood (with atresia, jaundice increases, the bound direct fraction of bilirubin predominates).
In conflict hemolytic jaundice, as in physiological jaundice, free bilirubin predominates; as a rule, there is a Rh conflict or a conflict in the ABO system.
The diagnosis of congenital syphilis, toxoplasmosis and cytomegaly is rejected or confirmed using serological reactions and special tests. If blockage of the bile ducts is suspected, antispasmodics are prescribed; under their influence, the bile ducts expand, the plugs come out, the jaundice quickly passes, and the child recovers.
Differential diagnosis with congenital giant cell hepatitis is possible only by using special research methods - laparoscopy and liver puncture biopsy.
An important role for making a correct diagnosis is played by: biochemical blood testing (total direct and indirect bilirubin is determined) and ultrasound examination.
An operation aimed at restoring the patency of the bile ducts is indicated. In case of total atresia and hypoplasia of the gallbladder, in order to partially divert bile into the intestines and prolong the life of the child, the thoracic lymphatic duct is transplanted into the esophagus.
The results of the operation are directly dependent on the form and degree of the developmental anomaly and the timing of the intervention. The best results can be obtained in the first 2 months of a child’s life.
Symptoms
Functional bending rarely causes complaints in a child. As long as normal bile flow is maintained, there is no negative effect on the body. This anatomical feature becomes an accidental ultrasound finding.
Symptoms will develop only with severe stagnation of bile. This usually occurs not with an isolated small bend, but when it is combined with another significant pathology or against the background of a gross congenital developmental anomaly. In other words, the appearance of complaints will indicate not the deformation itself, but a disruption of the biliary system. Signs that should alert you:
- Feeling of heaviness, pain in the right hypochondrium;
- Nausea, vomiting after eating;
- Skin itching;
- Yellowing of the skin and sclera;
- Darkening of urine, lightening of stool;
- Tendency to form gas.
A number of sources indicate symptoms that differ depending on the area of inflection of the gallbladder. They are not entirely correct. If the bend does not interfere with the functioning of the biliary system, its localization can only be determined by ultrasound. In acute situations, the clinic will depend on the underlying pathology that caused the complaints. If the child’s health condition worsens, it is necessary to seek qualified medical help in a timely manner, and not waste time on possibly erroneous self-diagnosis and self-medication.
Gallbladder diverticulum
- Diagnosis of adenomyomatosis
- Treatment of gallbladder disease
One type of gallbladder disease is adenomyomatosis or gallbladder diverticula. This type of protrusion is the so-called acquired type and is characterized by a thickening of the muscular layer of the gallbladder with the formation of characteristic diverticula. These diverticula are often called Rokitansky-Aschoff sinuses. Although the use of this term is well known in everyday practice, in fact it does not quite apply correctly to this case, since these sinuses are actually small passages of the surface epithelium in the wall of a given organ. Only when they are abnormally deep and associated with thickening of the gallbladder walls, the term adenomyomatosis or gallbladder diverticulum becomes relevant.
Depending on the patients, adenomyomatosis from 1 to 8.7% causes an acute complication that leads to cholecystectomy (surgery to remove the gallbladder).
The prevalence of this gallbladder disease largely depends on the criteria used in the diagnosis of resected gallbladders or autopsy specimens.
In more than 10,000 cholecystectomy specimens, only 103 cases of adenomyomatosis were found, giving an average prevalence of 1%.
This type of disease is more common in women than men with a ratio of 3:1, and its prevalence increases with age. This type of disease may involve the entire gallbladder (diffuse or generalized) or, more generally, may be localized at the bottom of this organ, in which case the protrusion is often called adenomyoma.
In rare cases, the process may be limited to an annular segment of the wall of the sac-like organ (segmental adenomyomatosis) and can lead to narrowing of the lumen. In any case, part of the wall of this organ thickens to 10 mm or more, and the muscle layer exceeds the norm by three to five times its normal state.
During the disease of the saccular organ, hyperplasia of the muscular layer (an increase in the structural elements of tissues through their excessive new formation) is invariably present, and the epithelial linings sometimes undergo intestinal metaplasia (the ability of tissues to change their appearance).
In this case, mild chronic inflammation is almost always present.
Adenomyomatosis usually does not cause any symptoms and can be discovered incidentally at autopsy or surgical resection. In rare cases, gallbladder adenocarcinomas (malignancies) are found in association with adenomyomatosis, but the malignancies are often located far from the localized area of adenomyomatosis.
Diagnosis of adenomyomatosis
As noted earlier, adenomyomatosis is often diagnosed only after resection and direct examination of the sac-like organ, however, several specific radiological and ultrasound studies can determine its presence and allow the diagnosis to be made immediately before surgery.
To determine the presence of protrusions in this part of the body, an oral cholecystography procedure is performed, which is an X-ray examination of the bladder using a contrast agent.
After taking this substance, it is absorbed in the small intestine, then enters the liver, from where it enters the bile and accumulates in the gallbladder.
After 12-14 hours have passed after taking the contrast, x-rays are taken to identify the features of the bladder, as well as for visual diagnosis to identify diverticula.
This procedure is not recommended after examinations using barium, since its residues can damage the clarity of x-rays, thereby complicating an accurate diagnosis.
Ultrasound (ultrasound diagnostics) can largely replace the procedure of oral cholecystography to assess the condition of the sac-like part of the body, but ultrasound diagnostics in the case of adenomyomatosis is less effective.
Carefully performed work, in which radiographic and ultrasound findings show that diffuse or segmental thickening of the walls of the saccular organ is present, in combination with a focal diverticulum, accurately predicts the formation of saccular organ disease.
Treatment of gallbladder disease
In the absence of symptoms of biliary tract disease, diverticulum in most cases does not require treatment.
If the patient has biliary pain and X-ray or ultrasound diagnostics indicate the presence of stones, then cholecystectomy (removal of the entire organ) is mandatory.
Cholecystectomy is also performed in cases of cholecystitis and gallbladder polyps.
Source: https://stopnikotin.ru/gryzhi/zhelchnogo-puzyrya
Diagnostics
One of the main and safe methods for detecting bends of the gallbladder in children is ultrasound of the abdominal organs. It allows you to visualize not only this feature, but also to exclude other pathologies that interfere with the normal functioning of the biliary system.
Thanks to some techniques, you can distinguish a functional bend from a fixed one. The study for this purpose is first carried out on an empty stomach. If an excess is detected, the child is given a choleretic breakfast (egg yolks or full-fat sour cream). Repeated examinations are performed at intervals of 15 minutes. If the kink is functional, it will disappear. The fixed deformation will remain unchanged.
Changes in the biochemical blood test can indirectly indicate congestion in the biliary system. In particular, the level of bilirubin increases due to the direct fraction.

Treatment methods
Treatment of gallbladder deformity in children is carried out comprehensively, in conjunction with diet, exercise therapy and taking into account the type of disorder. Children with chronic manifestations of the disease are advised to undergo physical therapy - electrophoresis and ultrasound. During an exacerbation, it is recommended to maintain bed rest and provide the child with plenty of fluids.
Painkillers and antispasmodics (Baralgin, Drotaverine or No-shpa, Atropine, Tramadol) are used intramuscularly. To treat the infection, Ampiox, Augmentin, and cephalosporins are prescribed while taking probiotics.
Choleretic drugs are prescribed taking into account the type of JVP and outside the period of exacerbation. To strengthen the body, the doctor prescribes vitamins: A, E, C, group B. Physiotherapy and herbal therapy are carried out taking into account the type of JVP during remission of the disease.
Treatment
If a curved gallbladder in a child does not lead to disruption of the outflow of bile and does not cause complaints, then we limit ourselves to observational tactics. Therapy in such situations, when the functional inflection is often a variant of the age norm, is inappropriate.
Treatment is carried out if there are disturbances in the functioning of the biliary system. For example, they resort to surgical elimination of a gross congenital anomaly that cannot be compensated conservatively. But such cases are extremely rare.
If gallbladder function is impaired, a more detailed examination is performed. More often, complaints arise not because of the bend itself, but against the background, for example, of biliary dyskinesia. Therapeutic tactics are based on eliminating the underlying pathology. In particular, for dyskinesia, choleretic drugs and antispasmodics are used (depending on the type of dyskinesia).
Important! It is impossible to take choleretic drugs (including herbal infusions) “just for prevention” if the child’s gallbladder is bent. They can only be used after a doctor's permission. Unreasonable intervention, on the contrary, can induce disturbances in the functioning of the biliary system.
Diet
If there is a bend in the gallbladder, it is necessary to adhere to the basics of proper nutrition. Principles:
- Regular meals. You need to eat 4-6 times a day in small portions. It is important to eat food at the same time. Overeating or, conversely, starvation should not be allowed.
- Preference for boiled and steamed foods. The diet should include porridge and low-fat soups.
- Balanced composition. The content of proteins, fats, and carbohydrates should be age appropriate.
- Maintaining temperature conditions. Food that is too cold or hot should be avoided.
- Exclusion of some products. It is necessary to minimize the consumption of foods with preservatives, dyes, flavor enhancers, and trans fats. For example, chips, fast food, and carbonated drinks are subject to restrictions.
Gallbladder diverticulum what is it treatment
The gallbladder is a pear-shaped organ designed to store bile.
This is a kind of reservoir for the bitter yellow-green liquid that is produced by the liver. The dimensions of the organ are small, the length of the bladder in an adult is approximately 8 cm, and the capacity varies from 40 to 60 cubic meters. see. In children and adults, the gallbladder normally lies on the surface of the liver, in the lower part of the organ, between the right and quadrate lobes. The gallbladder is mobile and can twist, which often leads to necrosis (cessation of the vital activity of cells).
The organ can be doubled; there are also cases of its dystopia, when the bladder takes an unnatural position in the abdominal cavity. There are known cases of intrahepatic location of the gallbladder.
Signs of gallbladder dysfunction are often nonspecific. The patient may experience weakness and general malaise, minor pain in the right side of the chest, nausea, and even a slight increase in body temperature.
People with such symptoms, unfortunately, rarely go to the doctor for help, trying to endure the discomfort in the hope that everything will soon go away on its own. As for the pronounced symptoms of gallbladder diseases, we can distinguish:
- pain;
- signs of digestive disorders;
- rich color of urine;
- clarified feces;
- nausea;
- bitterness in the mouth;
- yellowish color of the skin and sclera;
- decreased appetite.
Main causes and mechanism of disease development
Diseases associated with the gallbladder have different mechanisms of development. And the causes of diseases are most often different.
So cholecystitis is diagnosed as inflammation caused by a variety of microorganisms and a violation of the outflow of bile. The cause may also be helminthic infestation.
Diagnosis of gallbladder diseases
Regardless of the shape of the gallbladder, it is almost impossible to identify its anomalies from one clinical picture.
Irregularities in the functioning of the gallbladder are determined through comprehensive diagnostics. Only after a thorough examination of the patient is treatment prescribed.
A set of measures aimed at identifying abnormalities in the functioning of the organ will depend on the patient’s age, his complaints and the presence of chronic concomitant pathologies. The attending physician may prescribe ultrasound, CT, diagnostic laparoscopy, cholecystography, retrograde cholangiopancreatography, fine-needle biopsy, etc.
Ultrasound of the gallbladder
Ultrasound diagnostics are the most informative. It is this type of study that allows us to identify pathological changes in organ tissue, small stones, fluid accumulations, deformations, thickening, etc. Ultrasound of the gallbladder is the first and main diagnosis that a gastroenterologist should prescribe in cases where the patient complains of pain in the right hypochondrium .
Ultrasound of the gallbladder can be prescribed not only for the initial detection of diseases, but also as an observation of the dynamics of various pathological processes.
lab tests
As for laboratory tests, already at the first appointment with a gastroenterologist, the doctor may prescribe an ultrasound of the gallbladder and blood tests (general and biochemical). Additionally, the following may be recommended: liver tests, helminth analysis.
A clinical blood test will help identify inflammation, in which case the results will indicate an increased number of leukocytes and ESR.
drug treatment
No conservative method of therapy can eliminate a violation of the shape of the gallbladder, regardless of whether it is congenital or acquired. All non-surgical techniques are aimed at relieving symptoms.
For this purpose, use:
- Following a diet with limited consumption of fatty, fried and spicy foods, and alcoholic beverages.
- Choleretic drugs (Alohol, Holiver, Hofitol).
- Antispasmodics (No-shpa, Baralgin).
- With the development of acute cholecystitis - antibacterial agents.
People with gallbladder pathology benefit greatly from normalizing and maintaining a healthy weight through proper nutrition and moderate exercise.
Therapy for gallbladder diseases should always be comprehensive. It is selected individually, taking into account many nuances, namely the type of disease, its stage, the patient’s age, the presence of chronic pathologies, etc.
For diseases of the gallbladder, doctors advise excluding fatty meats and rich broths from the diet. You cannot smoke or fry foods; it is better to use steam and stewing for cooking.
In case of gallbladder diseases, it is necessary to take into account not only the menu, but also the food consumption schedule. It is advisable to eat at least 5-6 times a day. Portions should be small. A few hours before bedtime, it is better to refuse food altogether.
- To remove the cause of the disease, doctors prescribe etiotropic treatment.
This may include antibiotics and/or surgery (depending on the type of disease).
- To restore normal functioning of the gallbladder, pathogenetic treatment is prescribed.
Depending on the problem, these may be antispasmodics and/or enzymatic agents like Mezim.
- To reduce the intensity or completely eliminate the symptoms of diseases, anti-inflammatory drugs, painkillers and antispasmodics are prescribed.
This could be No-shpa, Ketanov, Paracetamol and other medications.
Diverticula: surgery and indications for its implementation
With the help of properly selected medications, you can get rid of inflammation. However, removal of the diverticulum is sometimes necessary. The operation can be planned (it is performed 2-4 months after successful drug treatment of inflammation in order to prevent relapses) and emergency (in the presence of intestinal bleeding, the risk of diverticulum rupture).
If we talk about emergency surgical intervention, then the indications for it are:
- rupture of the diverticulum and release of its contents into the abdominal cavity with further development of peritonitis;
- acute intestinal obstruction;
- the appearance of infiltration in the protrusion cavity;
- tissue suppuration;
- bleeding that cannot be controlled with medication;
- risk of malignant degeneration of diverticulum cells;
- fistula formation.
Excision of a protrusion of the intestinal wall is not performed on elderly patients or pregnant women. Contraindications include severe pathologies of the cardiovascular system (there is a risk of a reaction to anesthesia), chronic diseases during exacerbation, as well as any acute inflammatory or infectious diseases.
Consequences of abnormalities in the shape of the gallbladder
Sometimes various anomalies and deformations of the bladder can disrupt the outflow of bile from it, preventing the main function of the organ from being performed. The resulting stagnation of bile leads to the appearance of dystrophic changes in the walls of the gallbladder, it increases in size, and its contractile function worsens. Bile sludge promotes the formation of stones and the development of cholecystitis.
Source: https://giwot.ru/divertikul-zhelchnogo-puzyrya/