Diagnosis of the disease
At the first symptoms, the patient should seek medical help. After a general examination and tests, further examination will be required. Often in such cases, the study is carried out using ultrasound diagnostics. This is a painless and affordable examination method that allows you to conduct research on the pathology of the pancreas before detecting cancer in the early stages.
In what cases is an ultrasound scan of the pancreas performed?
The procedure is carried out to confirm the diagnosis - the accuracy of the determination of the method is high. Sometimes ultrasonography of the pancreas is performed with such features:
- persistent pain in the form of spasms in the left side of the stomach;
- possible suspicion of jaundice;
- formations discovered during examination (cyst, tumor);
- rapid weight loss without effort;
- stool instability;
- the presence of pain during examination of the source of the malaise;
- when examining other internal organs, detecting possible changes in the pancreas.
Examination of the pancreas using ultrasound is carried out for pancreatitis and possible diseases. If the symptoms coincide, there is a high probability of inaccuracy in diagnosis, resulting in inaccurate treatment.
Preparing for an ultrasound scan for pancreatitis
To carry out the procedure correctly, you should be thoroughly prepared. If we are talking about an emergency operational situation, ultrasound is performed without preparation. The accuracy will be much lower, visible results are not guaranteed. For a routine ultrasound, the patient must be explained how to prepare for the examination. Let's take a closer look at the procedure:
- Ultrasound is often prescribed in the morning, on an empty stomach; at this time, little air has accumulated in the digestive system.
- If time permits, 2 days before the procedure, remove foods that cause gas formation (fruits, vegetables, dairy products, soda) from your diet.
- To reduce flatulence, you can take activated carbon or espumizan.
- The last meal should take place at least 12 hours before the ultrasound, otherwise the result will be distorted.
- It is recommended to do an enema before the study.
- It is undesirable to use medications, alcohol, or smoking before the upcoming process.
A complete picture of the disease will require accurate data. Compliance with the listed preparation rules will allow you to obtain them.
The necessary conditions
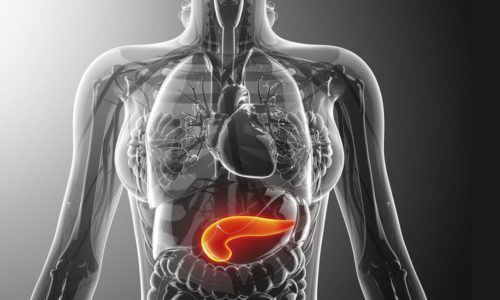
An ultrasound examination of the pancreas is designed to identify abnormalities in this area associated with disruption of the stomach, liver, spleen, intestines, and gall bladder.
Ultrasonography determines the contours of structures inside the organ, their size, shape, foreign formations and areas with different echogenic density, which is a sign of possible pathology.
The pancreas is normal on ultrasound examination
Gases in the intestine can seriously interfere with test results.
To avoid their occurrence, you must follow the preparation rules:
- it is prohibited to conduct a gastrological examination before performing a pancreatic examination;
- To avoid distortion of results, smoking and drinking alcoholic beverages are prohibited before ultrasound;
- if stool is abnormal, a cleansing enema must be performed before the examination;
- the night before the ultrasound, it is recommended to take 4 tablets of activated carbon (for more details on the use of the drug before the procedure, read the article...);
- to minimize the impact on test results, it is recommended not to eat food 10 hours before the ultrasound;
- 2 days before the examination, it is necessary to exclude from eating foods that cause gas formation: vegetables, fruits, lactic acid products, carbonated water.
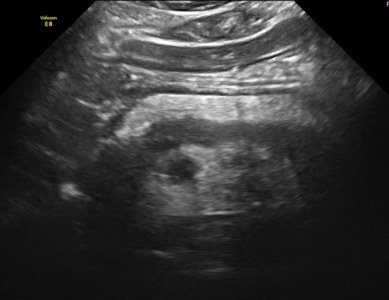
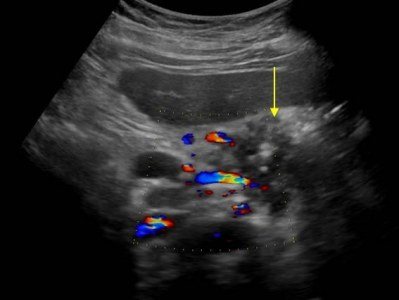
Dilated pancreatic duct
Ultrasound of the pancreas may not show a complete picture of the disease due to the low severity of symptoms in chronic pancreatitis and the presence of areas of uneven distribution of echo density. To obtain high-quality research results, in addition to ultrasound diagnostics, endoscopic retrograde cholangiopancreatography and computed tomography of the pancreas can be performed.
The use of several research methods shows the most complete information about the condition of the organ and allows us to determine a more effective method of treating reactive and chronic pancreatitis.
Healthy pancreas results
During the examination, ultrasound will show the overall picture using medical indicators that are unclear to the patient. The main numbers by which it is possible to guess the existence of pathology are the parameters of the pancreas - shape and size. The information is available for comparison to any patient. Then ultrasound reveals other points characteristic of the diagnosis of pancreatitis.
When the pancreas is scanned with the machine, the components of the organ are clearly visible: the body, tail and head. For an adult, the following sizes are considered normal:
- body up to 21 mm;
- tail up to 35 mm;
- head up to 32 mm;
- The width of the duct is no more than 2 mm, the walls are smooth.
The silhouette of the pancreas itself is outlined with a clear line, the structure is uniform. An important indicator is the echogenicity of the organ, which determines the ability of the gland to increase or absorb the signal from the device’s sensor. The screen is identified by image parameters, brightness and clarity. The normal value coincides with the data for the liver and spleen.
Let's take a closer look at the indicators determined for pancreatitis. For different types of pancreatitis, an individual picture is displayed on the screen.
Where to do an ultrasound of the pancreas?
Ultrasound examinations are carried out in specialized private clinics, or in those public medical institutions where there are special ultrasound machines that make it possible to scan and visualize this organ. The procedure requires certain preparation from the patient. Detailed advice regarding this can be obtained by making an appointment for an ultrasound scan. It is recommended to conduct the study in the first half of the day.
What does an ultrasound of the pancreas show, what are the normal values?
As a rule, ultrasound diagnostics of the pancreas is not done separately, but in conjunction with the examination of all abdominal organs. During the scan, the specialist looks at the liver and gallbladder. Also studies the condition of the intestines and spleen. In some cases and indications, the doctor even examines the stomach.
If the pancreas is completely healthy, its structure is homogeneous. However, sometimes small inclusions may appear. If the device provides a black and white image, the echogenicity of the organ tissue will be identical to the liver and spleen.
In addition to the organ itself, the doctor performing the procedure also checks the pancreatic duct. This part of the ultrasound examination is especially important when diagnosing pancreatitis or a tumor of the head.
Description of how to check the pancreas using ultrasound?
It is recommended to check the pancreas using ultrasound on an empty stomach. The last meal should be 12 hours before the scheduled procedure. Ultrasound diagnostics is carried out in this way - the patient lies down on the couch. The specialist applies a special gel to the skin and points the device at the area that needs to be visualized. In order to view the tail of the organ, the patient is turned on his side. Accordingly, the location of the sensor is also changed. In order to check the body and head of the gland, the patient will need to stand up.
The diagnosis of chronic pancreatitis is made on the basis of an ultrasound scan. However, ultrasound results alone are not sufficient to diagnose this disease 100%. The diagnostic capabilities of ultrasound are somewhat limited compared to the diagnosis of the acute form of the disease. This is due to the main echo signs of the chronic form of the disease.
What does acute pancreatitis look like?
A number of forms of acute pancreatitis are known; pathology implies mild and severe course of the disease. In the first case, the organ is slightly damaged; when the symptom is first removed, it becomes difficult to identify the seriousness of the situation. The severe form manifests itself in the form of certain indicators.
Indicators of acute pancreatitis
The general picture of signs of acute pancreatitis on ultrasound comes down to the following:
- the overall size of the organ is increased;
- the boundaries of the pancreas have an unclear contour, with curvatures;
- increased echogenicity in sources of inflammation;
- the structure is heterogeneous;
- the duct is much wider than normal;
- liquid conditions are detected in the organ area, changes in neighboring organs;
- in severe cases, cysts, areas of decay, and other uncharacteristic changes may be detected.
Changes in the abdominal cavity indicate acute pancreatitis. Along with laboratory tests, analyzing each symptom along with an ultrasound examination, confirmation of the diagnosis of acute pancreatitis will be reliable.
Ultrasound results

A gastroenterologist will not be able to make an accurate diagnosis solely on the basis of a survey of the patient and his examination. He needs additional tests and examinations to obtain additional data.
Conclusion Ultrasound for pancreatitis gives doctors a lot of information. This technique, however, is less reliable than magnetic resonance imaging and computed tomography, which can provide one hundred percent accurate diagnosis. It is especially difficult to find anything at the initial stage of the disease.
However, in most cases, an ultrasound examination, correctly performed and correctly deciphered by an experienced specialist doctor, allows one to identify pathology, as well as find the localization of areas with tumors and necrosis.
By conducting an ultrasound examination, the doctor tries to identify the presence or absence of:
- inhomogeneities;
- reducing echo density;
- thinning, softness of the parenchyma;
- enlargement of the pancreatic ducts.
All this allows him to assume the presence of pancreatitis. Currently, a couple of ultrasound diagnostic techniques are actively used:
- the classic, familiar option;
- EUS, or endoscopic ultrasonography.
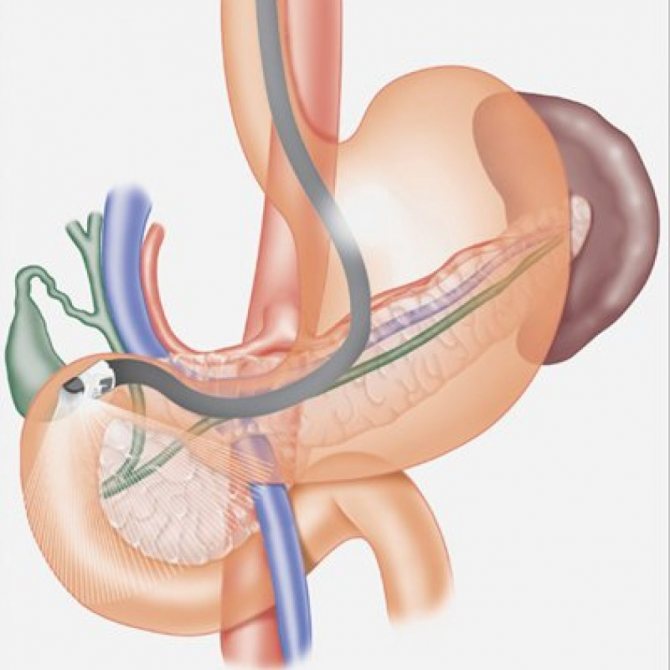
Endoscopic ultrasonography is considered more informative than the classic version. However, this examination causes more discomfort to the patient. The fact is that in this case, a sensor that makes it possible to study the pancreas is inserted through the gastric cavity. This way it can be brought as close as possible to the organ being examined. As a result, greater detection accuracy is achieved:
- size and structure of the pancreas;
- condition of the lymph nodes;
- the absence or presence of pathologies in the biliary system.
The greatest effectiveness of the endoscopic ultrasonography method is achieved when identifying the biliary variant of pancreatitis. It is also quite accurate in determining localization:
- areas of pancreatic necrosis;
- cyst;
- tumors.
This diagnosis is successfully used in the treatment of many types of neoplasms. It helps to drain pseudocysts, as well as administer medications to the area adjacent to the pancreas.
The main disadvantage of this technique is the risk of injury and, as a result, infection. Therefore, endoscopic ultrasonography is used only if there are sufficient indications.
Pancreatitis in its classic version is not so clearly visible on ultrasound. However, this method complements well the interview and examination of the patient, as well as other examinations and tests. With the help of ultrasound it is quite possible to:
- identify signs of chronic disease;
- identify the presence or absence of neoplasms;
- carry out differential diagnosis.
Whatever method doctors choose and no matter how much data they receive as a result, they try to supplement it with information provided by other diagnostic methods. Only then do they have a fairly clear picture.
For a healthy pancreas

During a scan of the pancreas with pancreatitis, as well as without it, the doctor tries to see the contours and sizes of all its parts:
- bodies;
- heads;
- tail
If the gland is healthy, these components are clearly visible. The body size is no more than 21 millimeters, the head is no more than 32 millimeters, the tail is no more than 35 millimeters. In the pancreatic duct, the diameter reaches a maximum of two millimeters. Its walls are normal – smooth. The contour of the pancreas itself should be smooth and clear.
If it is healthy, then its structure is homogeneous. In some cases, it is permissible to have separate areas where the echogenicity is reduced or increased - from one and a half to three millimeters. It is important to understand that echogenicity is the ability of an organ to absorb or amplify the ultrasound signal coming from the sensor. On the device screen it corresponds to the brightness and intensity of the picture. If everything is in order, then in the pancreas this indicator should not differ from the echogenicity of the spleen and liver.
For acute pancreatitis

When a doctor does an ultrasound for acute pancreatitis, he notes that the pancreas is enlarged. He can also see how its echogenicity has increased in the foci of inflammation. The gland has fuzzy, uneven contours.
Acute pancreatitis can be seen on ultrasound using such an indicator as the expansion of the Wirsung duct by more than two millimeters, while its wall is visualized unevenly and unclearly. At the stage of pancreatic necrosis, the following are often noticeable:
- areas of decay;
- pseudocysts;
- abscess formation of the pancreas and organs located nearby.
The latter manifests itself in the form of an increase in size and swelling of the affected areas. If pancreatic necrosis is complicated, fluid is sometimes found in the abdominal cavity, and pockets of pus are found in the omentum and abdominal wall. It is important to focus on certain points mentioned above.
For chronic pancreatitis
Ultrasound for chronic pancreatitis gives a slightly different picture. The duct of Wirsung is steadily dilated. The contours of the pancreas are covered with small bumps, jagged in some places.
In chronic pancreatitis, ultrasound reveals reduced echogenicity against the background of an increase in the size of the affected organ. If the disease progresses, echogenicity increases due to atrophy and fibrosis of the gland. The fact is that in this case its tissues become sclerotic.
Connective tissue, which is denser, replaces the glandular structure. The size of the organ becomes smaller, but the duct remains expanded. Sometimes an ultrasound examination reveals signs of chronic pancreatitis, but does not provide the necessary amount of data. In such cases, the patient is advised to undergo computed tomography and magnetic resonance imaging.
Indicators of chronic pancreatitis
The ultrasound screen shows individual changes characteristic of chronic pancreatitis. Features of manifestation:
- constant expansion of the duct over 2 mm;
- the boundaries of the organ reveal a jagged membrane, sometimes with small tubercles;
- in addition to increased size, echogenicity will be less;
- sometimes pseudocysts are found in advanced disease, in such a case the echogenicity will be higher;
- as the disease progresses, the monitor screen shows how visually the pancreas becomes smaller compared to the enlarged duct, due to atrophy;
- if there is a suspicion of stone formation in an organ, you will see a circle-shaped spot with an echogenic trace;
- the structure of the organ is heterogeneous, with diffuse errors.
The effectiveness of ultrasound in pancreatitis
Using ultrasound, they examine the general visual picture of the condition of the organ, regarding the size, shape, and silhouette of the object. When changes occur, there is a reason to concentrate attention on this point. The use of ultrasonography is considered a mandatory method for diagnosing pancreatitis in any form of manifestation. The use of an examination method helps in making a diagnosis, prescribing the correct treatment for a complex disease, and allows for periodic analysis of the condition of internal organs.
Thanks to ultrasound, the initial stage of the disease is detected, and it is easy to monitor organs. For the doctor and the patient, it is easier to prevent an impending threat than to fight it later.
Ultrasound for pancreatitis plays an important role in detecting pathological changes in the pancreas characteristic of this disease. However, based on the results of this procedure alone, it is impossible to make an accurate diagnosis; the ultrasound method is combined with other hardware and laboratory techniques.

Indications and contraindications
Indications for ultrasound of the pancreas:
- severe pain and spasms in the epigastric region;
- the appearance of signs of obstructive jaundice;
- tumors detected by palpation;
- rapid weight loss with the usual diet;
- constipation followed by diarrhea.
Ultrasound is not used in the diagnosis of pancreatitis:
- for infectious diseases and skin damage;
- in severe general condition of the patient;
- for grade 3 obesity;
- with diverticulosis of the esophagus;
- with recent surgical interventions in the upper parts of the digestive system;
- if there are signs of peritonitis;
- in acute heart failure;
- with aortic aneurysm (pathological change in the walls of the vessel, promoting the expansion of some of its sections);
- with inflammatory processes in the upper respiratory tract and lungs;
- with increased blood pressure;
- with curvature of the cervicothoracic spine;
- with exacerbation of chronic coronary insufficiency;
- with a perforated stomach ulcer.
Preparation
Proper preparation helps to obtain reliable research results. Before undergoing an ultrasound, the following rules must be observed:
- Avoid eating and drinking for 12 hours before the procedure.
- Cleanse the intestines the day before the ultrasound. Taking adsorbents and laxatives and performing an enema will help with this.
- Following a special diet. A week before the examination, foods that contribute to fermentation processes in the intestines are excluded from the diet: legumes, cabbage, rich bakery products, carbonated drinks, sweet fruits.
- Taking carminative drugs that reduce the intensity of gas formation.
- Refusal to take medications on the day of the ultrasound. Carried out with the permission of the attending physician.
Preparing for diagnosis

Before going through an ultrasound scan of the pancreas for pancreatitis, doctors recommend carefully preparing. It is advisable not to eat anything at all for twelve hours before visiting the doctor. It is also advisable to cleanse the intestines well on the morning of the examination.
For three days before this, foods that promote the formation of gases and fermentation in the gastrointestinal tract are prohibited from consumption:
- cabbage;
- any legumes;
- pears;
- grape;
- rich yeast baked goods;
- carbonated drinks and so on.
To reduce flatulence, doctors allow you to take a drug like espumisan. But in the morning before the ultrasound examination, you should not take medications, smoke or drink.
Whether an ultrasound will show the presence of pancreatitis, and how accurately this will be done, depends on the quality of following the specified preparation rules. In emergency cases, patients are examined without preparatory manipulations, but the accuracy of the results is greatly reduced.
Procedure
The ultrasound scan of the pancreas includes the following steps:
- Taking the correct position. The patient is asked to lie on the couch on his back, the stomach is freed from clothing.
- Installing the sensor in its original position. Before this, a special gel is applied to the skin to facilitate the sliding of the device.
- Examination of the organ. The ultrasound transducer is slowly moved toward the upper left quadrant while applying gentle pressure to the patient's abdomen. After this, the patient is asked to turn on his right side. Taking a semi-sitting position helps to facilitate visualization of the head and body of the pancreas.
- Assessment of organ parameters using a special program. Based on the data received, the specialist writes a conclusion, which is then sent to the attending physician.
- Obtaining images of the organ. Some machines make it possible to take a photo that will be used when planning a biopsy or surgery.
Analysis of results
Decoding the examination results using this method gives the gastroenterologist the opportunity to establish a diagnosis of pancreatitis, determine its form and identify complications.

To do this, the doctor carefully studies the data specified in the ultrasound protocol.
Normal indicators
The following indicators are typical for a healthy gland:
- smooth, clear contours;
- the presence of three sections: head, body and tail;
- body size no more than 20 mm, head - 30 mm, tail - 35 mm;
- homogeneous structure;
- the presence of small areas of increased or decreased echogenicity, indicating different tissue abilities to absorb ultrasonic waves;
- smooth contours of the walls and normal diameter of the lumen of the pancreatic duct;
- absence of anechoic inclusions.
Fungi with pancreatitis have a negative effect on the organ.
Are yoghurts good for pancreatitis?
Deviations from the norm
The nature of the deviations depends on the form and duration of the disease.
Diagnosing acute pancreatitis using ultrasound is easier than chronic pancreatitis. The protocol in this case reflects the following changes:
- pronounced enlargement of the pancreas;
- blurred contours;
- expansion of the pancreatic duct, changes in the boundaries of its walls;
- swelling and enlargement of nearby organs;
- the presence of fluid in the abdominal cavity;
- the appearance of large areas with altered echogenicity, representing abscesses and fistulas.
Chronic inflammation has slightly different echo signs:
- Change in gland size. With a long course of pathology, the size of the organ decreases, which is associated with the presence of atrophic and fibrotic changes. Enlargement of the pancreas is detected in the acute phase.
- Enlargement of one department. This sign indicates the presence of complications of chronic pancreatitis (pseudocysts, benign and malignant tumors).
- Heterogeneity of the organ structure. Multiple hyperechoic inclusions appear in the tissues, representing foci of fibrosis.
- Changes in the contours of the pancreas. The outer parts of the organ are retracted, which contributes to its deformation.
- Dilatation of the pancreatic duct up to 3 mm or more, the presence of narrowed and dilated areas.
What does an ultrasound show?
Ultrasound diagnostics is prescribed for suspected pancreatic pathology in order to establish an accurate diagnosis as soon as possible and prescribe effective treatment. An ultrasound scan of the pancreas must determine:
- position;
- shape;
- contours;
- presence of liquid;
- echogenicity;
- presence of volumetric formations.
Normally the dimensions should be:
- pancreas length – 12–15 cm;
- head – up to 30 mm;
- body – up to 24mm;
- tail – up to 25 mm.
In most cases, the gland is located correctly. Sometimes anomalies and defects (ring-shaped, transposition of organs) of the pancreas are detected.
To determine the degree of changes in the pancreas, the Cambridge classification is used:
| Changes | Indicators |
| norm | sizes within normal limits; the contours are clear; main pancreatic duct (MPD) = 2mm; homogeneous parenchyma. |
| questionable changes | at least one of the following signs is present: gland is slightly enlarged; GPP 2–4mm; heterogeneous parenchyma. |
| soft changes | GLP – 2–4 mm; The pancreas is enlarged; parenchyma is heterogeneous; the edges of the pancreas are blurred. |
| moderate changes | cysts up to 10 mm; uneven GPP; there is necrosis; echogenicity is increased; uneven contours. |
| significant changes | In addition to the enlargement of the pancreas, heterogeneity of the contours is visualized: cysts over 10 mm; GLP pathologies; stones or pancreatic calcification; ingrowth into neighboring organs. |
An ultrasound of the pancreas is often prescribed for pancreatitis in order to determine how the disease progresses. If it decreases, then the swelling decreases and the patient recovers.
When diagnosing pancreatic diseases, the unevenness, blurriness and jaggedness of contours, the presence of fluid and calcifications, and the size of the ducts are important. For an accurate diagnosis, all indicators must be taken into account. For example:
- Enlarged pancreas, changes in contours and diffuse echogenicity may indicate the presence of a tumor, autoimmune pancreatitis, tuberculosis, syphilis, or parasitic organ damage.
- The presence of fluid in the lesser omentum bursa indicates chronic pancreatitis. During exacerbation of the disease, ultrasound shows the presence of large hypoechoic areas against the background of increased echogenicity of the parenchyma, blurred contours.
- If a cyst is found with homogeneous contents and dense, calcified walls, then this indicates a parasitic origin.
- A decrease in the echogenicity of the parenchyma and blurred contours are observed with hemorrhagic pancreatic necrosis, and an increase is observed with fatty necrosis.
It is important to know! Uniform echogenicity of the pancreas is the norm for people over 50 years of age and is interpreted as an age-related change. But in some cases, this may indicate serious pathologies, especially in combination with other signs. Therefore, only a doctor can make an accurate diagnosis based on ultrasound results.
A doctor may make an incorrect diagnosis based on ultrasound of the pancreas if the patient does not prepare for the procedure in advance. In the case when an emergency examination is required, the specialist knows that there are factors that distort the clinical picture, and he must take them into account.
Pancreatic cysts on ultrasound
Single small simple cysts occur as incidental findings in the healthy pancreas. In chronic pancreatitis, small simple cysts are quite common. If a cyst is suspected, note the enhancement of the contour of the far wall and the effect of signal enhancement in the tissue behind. Simple cysts are isolated from the parenchyma by a smooth thin wall. There should be no partitions or wall irregularities inside; the contents of the cyst are anechoic. Simple cysts are always benign. But, if the cyst is not obviously “simple”, further investigation is required.
| Photo. Simple pancreatic cysts on ultrasound. A, B — Single simple cysts in the area of the body (A) and neck (B) of the pancreas with a thin smooth wall and anechoic contents. B - Classic signs of chronic pancreatitis: the main pancreatic duct is dilated against the background of parenchymal atrophy, the contour of the gland is uneven with notches, there is calcification and small cysts in the parenchyma. | ||
|
| |
Important. Simple pancreatic cysts are common, but don't forget about cystic tumors. Cancer is the most dangerous disease of the pancreas.
There are two types of pancreatic cystic tumors: benign microcystic adenoma and malignant macrocystic adenoma. Microcystic adenoma consists of many small cysts and appears as a dense formation on ultrasound. Macrocystic adenoma usually includes fewer than five cysts larger than 20 mm. Sometimes polypoid formations can be seen in such cysts.
| Photo. A, B - Benign microcystic adenoma of the pancreas: a large cystic formation in the head of the pancreas. B - Pancreatic adenoma with macro- and microcystic components. | ||
|
|
|
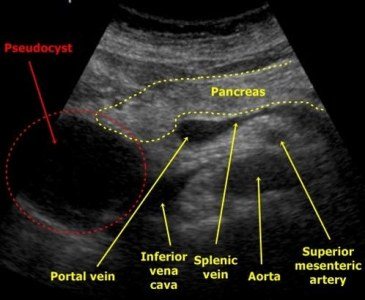
With pancreatitis, pancreatic secretions digest surrounding tissue and pseudocysts form. Pseudocysts from the abdominal cavity can extend into the chest and mediastinum. Pseudocysts are often found in patients who have suffered acute pancreatitis (see below).
As a result of pronounced dilation of the pancreatic duct, retention pseudocysts may form distal to the site of obstruction.
What can be determined using ultrasound
All patients with inflammation of the pancreas are prescribed an ultrasound examination. It is carried out for both acute and chronic pancreatitis, and if the disease is suspected.
An ultrasound will show the condition of the contours and tissues of the gland:
- if the contour is blurry, it means that inflammatory changes are occurring in the pancreas and swelling has begun. But it may also be evidence of a disease of the stomach or duodenum;
- the contour is convex, but at the same time smooth - a cyst has formed on the gland;
- uneven outlines are characteristic of pancreatitis and neoplasms;
- lumpy, blurry edges indicate cancerous formations.
An ultrasound examination also demonstrates the condition of the pancreatic tissue. In a healthy person it is of medium density. If the density is increased, it means that the connective tissue has grown. This condition is typical for chronic pancreatitis, but may be evidence of age-related changes. There are white areas on the screen.
If the fabric density is reduced, the image on the screen will be black. This condition is typical for the acute form of pancreatitis.
At each stage of the disease, the contours of the pancreas and its structure change. In the first stage of the acute form of the disease, the contours of the pancreas are blurred and uneven, the density is reduced, and the duct is dilated.
At the second stage, a cyst or abscess may appear. The contour will be rounded, the density of the tissues will decrease.
With chronic pancreatitis, the contours become unclear. If stones appear in the gland, the contour will become rounded, and the density in this place will increase.
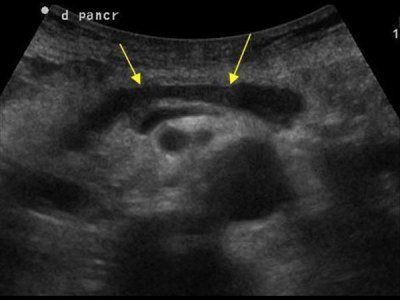
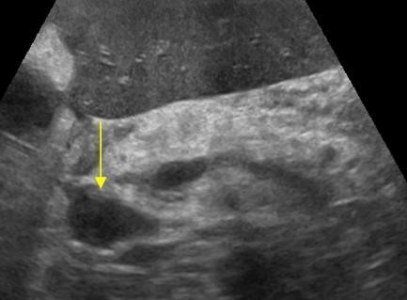
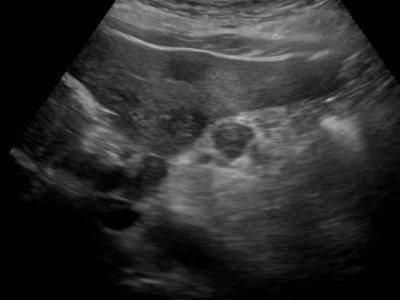
Acute pancreatitis on ultrasound
Acute pancreatitis is a severe complication of gallstone disease or a consequence of toxic effects, such as alcohol.
Mild pancreatitis is not visible on ultrasound (CT is a more sensitive method). Severe pancreatitis is easily detected by ultrasound. When an unusually clear and contrasting pancreas stands out from the surrounding tissue, edema of the parenchyma and surrounding fatty tissue can be assumed. If a thin layer of free fluid is visible around the pancreas, along the stomach, at the hilum of the liver and spleen, pancreatitis can be confidently diagnosed.
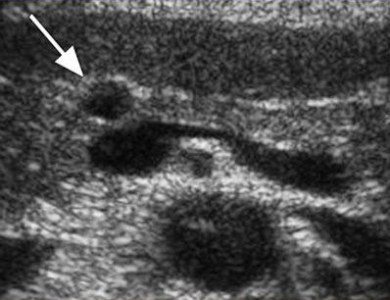
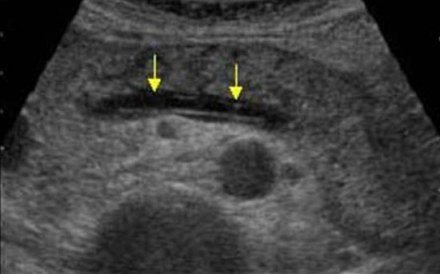
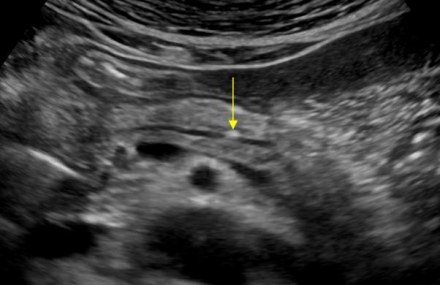
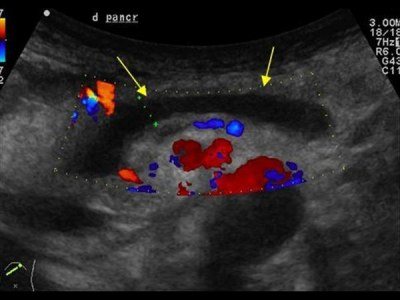
| Photo. Acute pancreatitis on ultrasound: A - Swelling of the pancreatic parenchyma (p), the contour of the pancreas is unusually clear, a small accumulation of fluid along the border (arrows). B, C - Accumulation of fluid along the contour of the body of the pancreas, a thin rim of fluid along the splenic vein (arrows), the parenchyma is heterogeneous, the surrounding tissue is hyperechoic - swelling and inflammation, the common bile duct is dilated (B). In this case, gallstone disease must be excluded. | ||
|
|
|
Almost all pancreatic tumors are hypoechoic compared to the normal pancreas. It is impossible to distinguish between focal pancreatitis and pancreatic tumor using ultrasound alone. A tumor and pancreatitis can be combined.
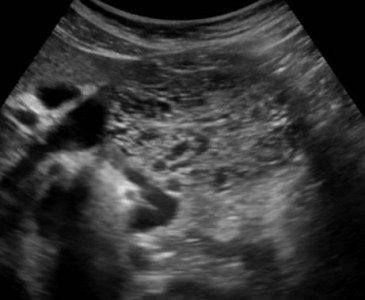
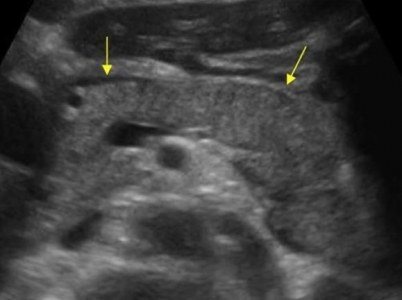
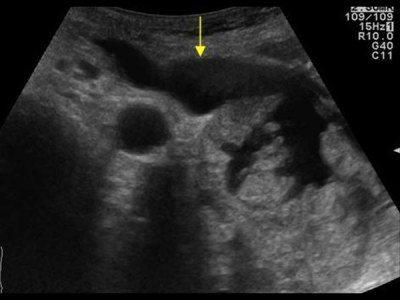
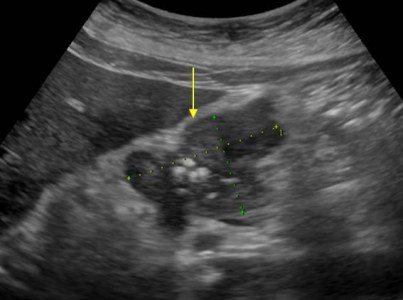
| Photo. Acute pancreatitis on ultrasound: The pancreas is unusually contrasted against the background of hyperechoic surrounding tissues, a thin strip of fluid along the contour (A), a hypoechoic focus in the tail (B), fluid in the hilum of the spleen (C). A hypoechoic tail can be mistaken for a tumor. | ||
|
|
|
In severe cases of pancreatitis, pancreatic fluid digests surrounding tissue, forming pseudocysts. Such cysts can be single or multiple. They may increase in size and rupture.
On ultrasound, pseudocysts are defined as oval or round hypoechoic formations with clear contours. In the early phases of cyst formation, it is a semi-liquid formation and has a complex echostructure with internal reflections and unclear contours. Later, due to autolytic processes and sedimentation of a suspension from blood and pus, clear signs of liquid contents appear and a false capsule with smooth walls is formed. Infection of pseudocysts often occurs, then internal echo structures or thin delicate septa can be detected. When a cyst is detected, it is important to trace the connection of the cyst with the duct, as this is important for determining treatment tactics. When a pseudocyst is more than 10 cm in size, difficulties arise in determining its source.
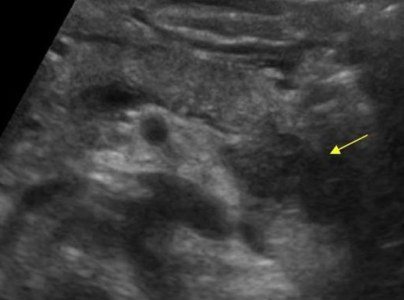
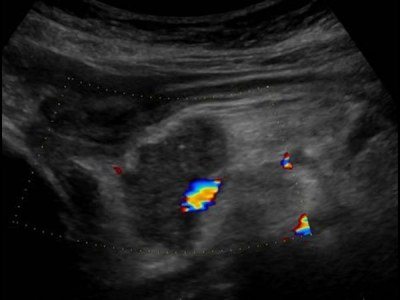
| Photo. A - Large pseudocyst between the head of the pancreas and the liver after pancreatitis. B, C - Severe necrotizing pancreatitis longitudinal (B) and transverse (C) sections: extensive necrosis, melting of the surrounding fat in the tail area, accumulation of fluid around the gland. | ||
|
|
|
When does such a change in an organ occur?
Normally, the pancreatic margin and the parenchyma of the organ itself are clearly visualized on ultrasound.
But under some circumstances and diseases, a wavy area, scalloped angle and other changes in echogenicity may be visualized.
Changes can be local or diffuse.
These are important diagnostic criteria for establishing the prevalence of the process.
A diffuse process occurs in the following pathologies:
- Swelling or anasarca. Swelling of internal organs occurs when they are directly affected or due to secondary damage in the case of pathology of another organ. Primary edema occurs in the case of pancreatitis. In this case, swelling is an indication for immediate treatment. Anasarca is swelling of all organs and tissues of the body, including the pancreas. This condition develops due to severe damage to the cardiovascular system or renal filter.
- Autolysis or necrosis of pancreatic tissue. This is an extremely severe surgical pathology, which is a consequence of acute pancreatitis. In this case, all functional active cells of the organ die, and the pancreas is not clearly differentiated. Autolysis is accompanied by the release of a large number of enzymes into the bloodstream. During a blood test, the doctor notes how the enzyme activity of the blood increases.
- Fatty degeneration of pancreatic tissue. In this case, active cells are replaced by inactive adipose tissue. The process is chronic and is not accompanied by severe symptoms.
- Type 1 diabetes mellitus, despite its hormonal nature, has a pathological focus. In the first type of disease, death occurs by the islet of Langerhans diffusely throughout the organ and this is noticeable on ultrasound.
- Tumor process of an organ or metastatic lesion. To exclude cancer, a number of other studies should be performed, such as MRI, CT and biopsy.
- Polycystic lesions or multiple cysts of the organ. Such pathological foci have a clear appearance and a smooth edge; phenomena are characteristic of a disease such as cystic fibrosis.
Additionally, the occurrence of a diffuse process is observed with fibrosis of the organ. This disease is characterized not only by high echogenicity, but also by a decrease in the organ itself.
Click on pictures to enlarge.
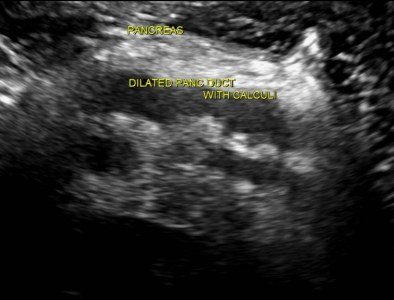
Calcifications in the pancreas on ultrasound
Important. If there is dilatation of the pancreatic duct, you should look for stones in the pancreatic duct and in the common bile duct.
Calcifications inside the pancreas can give an acoustic shadow, but if they are small, they appear as a separate bright echostructure without an acoustic shadow. In chronic pancreatitis, calcifications are distributed diffusely throughout the pancreas. Stones in the duct are located along the duct. Gallstones in the distal common bile duct may be mistaken for calcifications in the pancreas. Calcifications are clearly visible on CT, and for non-calcified stones, MRI or ultrasound is preferable.
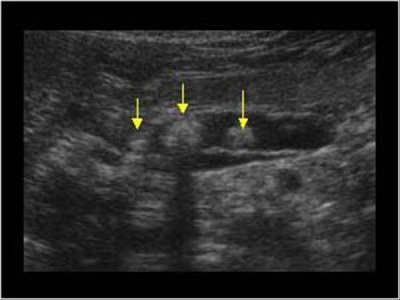
| Photo. A - There is a small stone in the dilated duct. B - In the dilated pancreatic duct there is a row of several stones with shadowing behind. B — A patient with chronic pancreatitis has huge stones in the dilated duct. Note the intense shading behind. | ||
|
|
|
| Photo. A, B — Calcifications in the pancreatic parenchyma in patients with chronic pancreatitis. Some calcifications have a shadow. B — A 5-year-old boy with chronic hereditary pancreatitis: calcifications (small arrows) and dilatation of the pancreatic duct (large arrow). C - confluence of the superior mesenteric and splenic veins. | ||
|
| |
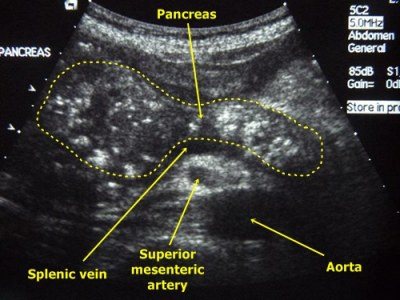
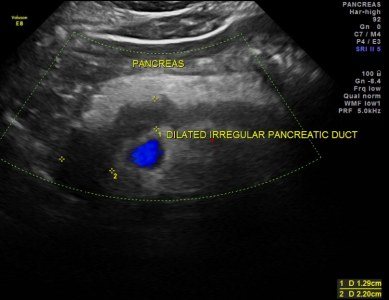
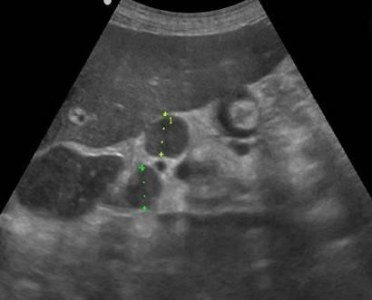
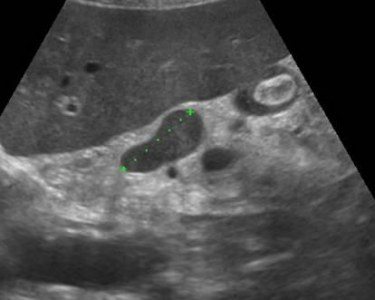
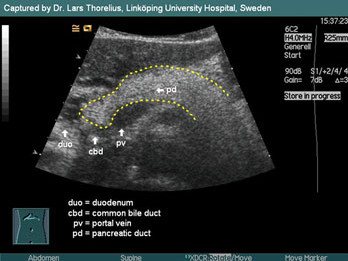
Dilated pancreatic duct on ultrasound
The internal diameter of the normal pancreatic duct is less than 3 mm. The duct is better visualized with transverse scanning in the middle third of the body of the pancreas. In order to make sure that you have found the duct, you need to see the pancreatic tissue on both sides of it. The splenic vein posteriorly or the gastric wall anteriorly may be falsely interpreted as the pancreatic duct.
The walls of the pancreatic duct should be smooth and the lumen should be clean. When the duct is dilated, the walls become uneven; scan not only the head of the pancreas, but also the entire biliary tract.
The main causes of dilatation of the pancreatic duct: tumor of the head of the pancreas or ampulla of Vater's papilla (combined with jaundice and dilatation of the biliary tract); stones of the common bile or pancreatic duct; chronic pancreatitis; postoperative adhesions.
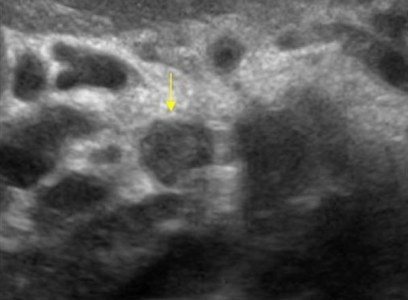
| Photo. A man with insulin-dependent diabetes mellitus complains of weight loss and abdominal pain for several months. Ultrasound shows an enlarged common pancreatic duct with an uneven wall. Upon further examination, calcifications with a shadow behind them are clearly visible in the duct (B). | ||
|
|
|
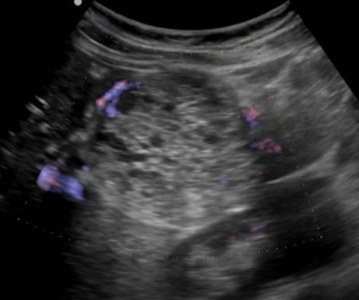
| Photo. A patient with acute pancreatitis: a large pseudocyst has formed at the level of the tail (see above), the dilated pancreatic duct opens into a pseudocyst. | ||
|
|
|
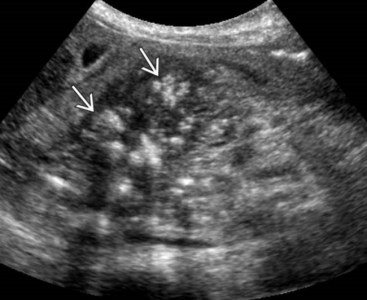
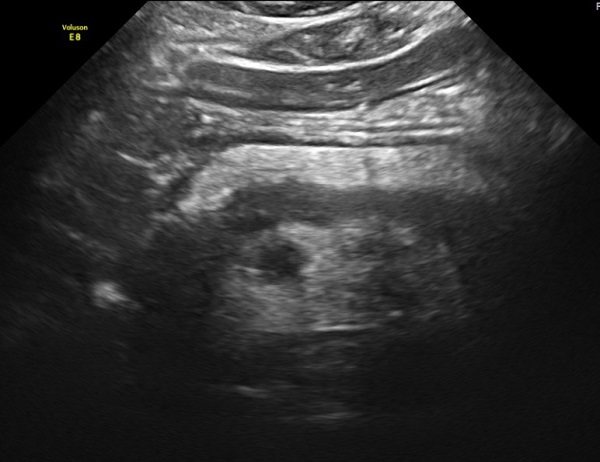
Pancreatic tumors on ultrasound
In most (50-80%) cases, the tumor affects the head of the pancreas. Tumors of the head compress the common bile duct. In cancer of the pancreas, the contour of the pancreas is unclear; local enlargement or bulging of the gland is characteristic, sometimes penetrating into the surrounding tissue in the form of tongues or pseudopodia.
In most cases, a pancreatic tumor is a hypoechoic formation, almost devoid of internal echo structures. However, there are tumors with diffusely scattered echo signals and with high-intensity echo signals in the center and their absence in the periphery. Despite the fact that the boundary between the tumor and the rest of the parenchyma of the gland is unclear, it can always be approximately drawn due to the difference in the echogenicity of normal tissue and the tumor focus.
Although the hypoechoic structure of the tumor, especially in the absence of small areas of increased density in it, resembles that of cysts, the absence of the effect of distal enhancement allows us to exclude the liquid nature of the formation. In addition, cysts are characterized by a much smoother and clearer border.
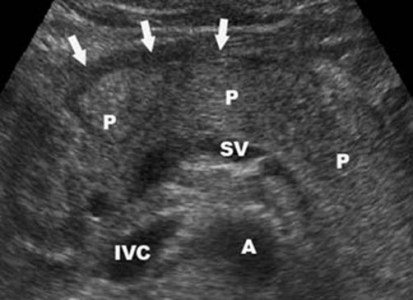
| Photo. Carcinoma of the head of the pancreas (arrow): the common bile duct (A) and pancreatic duct (B) are dilated, and a hypoechoic tumor surrounds the superior mesenteric vein (C). | ||
|
|
|
With tumors of the head of the pancreas, the common bile and pancreatic duct is often dilated, unlike chronic pancreatitis, its walls are smooth and not compacted.
Important. Visualization of the main pancreatic duct within the hypoechoic zone is in favor of local edema and against tumor.
Sometimes, with pancreatic cancer, typical signs of chronic pancreatitis are revealed, as well as pseudocysts distal to the site of tumor obstruction. This is a consequence of obstruction. Intrahepatic metastases, enlarged celiac, periportal and retroperitoneal lymph nodes indicate cancer.
| Photo. Carcinoma of the head of the pancreas: the contour of the head is uneven due to a volumetric hypoechoic formation, the parenchyma of the body is very thin (atrophy), the pancreatic (A) and common bile (B) ducts are dilated, and there is a large round lymph node (C) at the porta hepatis. | ||
|
|
|
| Photo. A large lymph node (arrow) next to the pancreas may be mistaken for a tumor of the head. Enlarged mesenteric lymph nodes are round in shape, hypoechoic and without a central scar, which indicates their malignancy. | ||
|
|
|
| Photo. Large neuroendocrine tumor(arrows) of the pancreas with calcification and liver metastases (B). | ||
|
|
|
Take care of yourself, Your Diagnosticer !
What is pancreatic cancer
Pancreatic cancer is a malignant tumor that develops from epithelial cells. In 10% of cases the disease is hereditary, the remaining 90% are classified as sporadic cases.

Etiological risk factors:
- abuse of fatty and meat foods;
- excess intake of easily digestible carbohydrates (sugar, cakes, sweets, baked goods);
- vitamin D3 deficiency;
- alcoholism and smoking;
- lipid and carbohydrate metabolism disorders: diabetes mellitus, metabolic syndrome, obesity;
- decreased physical activity;
- chronic pancreatitis;
- occupational hazard – work associated with contact with chemicals: asbestos, formaldehyde, toluene.
Symptoms in the early stages of cancer development are scant and do not differ in specificity, therefore periodic preventive screening studies using abdominal ultrasound are extremely important among people at risk.
Clinical manifestations depend on the location of the tumor.
If the head of the pancreas, which is in contact with the hepatobiliary system, is affected, then icteric coloration of the mucous membranes and skin occurs, itching, urine darkens, feces are discolored, and pain like biliary colic occurs.
In 95% of cases, when the body and tail are involved in the pathological process, severe back pain, obstruction and obstruction of the duodenum occur.
Common features are:
- Loss of body weight is associated both with the oncological process itself, leading to an increase in basal metabolism, and with indigestion and absorption of nutrients due to a deficiency of pancreatic enzymes.
- Dyspepsia: loss of appetite, nausea, vomiting, alternating diarrhea with constipation - occurs due to enzyme dysfunction of the gland and cholestasis.
- Weakness develops with malnutrition and anemia.
- The increase in temperature is caused by a secondary inflammatory process in the bile ducts or the effect on the thermoregulation centers of toxic decay products of a cancerous tumor.
- Ascites appears with damage to the peritoneum, compression of the portal vein, metastases in the liver and hypoproteinemia.