What are cholecystitis and pancreatitis?
Cholecystitis is an inflammation of the gallbladder caused by the development of cholestasis. The cause of the latter is complete/partial blockage of the bile ducts. The development of cholecystitis can be triggered by the following factors: regular overeating, addiction to fatty meats, spicy foods.
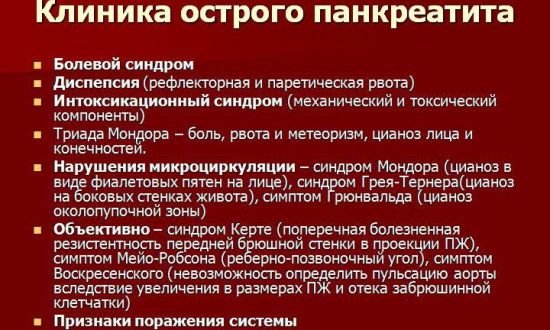
Potential signs of an acute form of pathology are:
- nausea, vomiting;
- yellowing of the skin;
- bitter taste of saliva;
- increase in general body temperature;
- pain in the right hypochondrium.
Exacerbation can be caused by drinking alcohol and eating too fatty/spicy foods. The cause of acute pancreatitis is inflammation of the gland, caused by a violation of the outflow of pancreatic juice. As a result, pancreas cells begin to digest themselves, which causes the development of the pathological process.
Typical signs of pancreatitis are:
- severe pain in the left hypochondrium, sometimes of a girdling nature;
- nausea, vomiting;
- diarrhea;
- increased gas formation;
- significant increase in body temperature.
The diseases are closely interrelated. Cholecystitis can provoke a violation of the outflow of pancreatic juice, causing the development of pancreatitis. Conversely, the reflux of digestive enzymes of the pancreas into the lumen of the bile duct causes the formation of cholecystitis.
Diet for pancreatitis, cholecystitis and gastritis
When prescribing one type of nutrition or another, a nutritionist must always take into account other concomitant diseases that occur against the background of the underlying pathology. Gastritis, which occurs against the background of inflammation of the gallbladder and pancreas, requires a review of dietary nutrition with an emphasis on the degree of acidity of gastric juice.
Features of the diet for pancreatitis, cholecystitis and gastritis may be applicable to other diseases of the digestive tract. This includes small and moderate meals, the absence of long intervals between meals, and adherence to a daily nutritional routine. It is important to avoid overeating, eating on the run and dry food, not drinking alcohol and not smoking, since tobacco smoke and tars swallowed with saliva also negatively affect the composition of gastric juice and irritate the walls of the stomach.
The simultaneous course of inflammatory processes in the pancreas, stomach and gall bladder is a forced signal from your body, indicating major problems and nutritional disorders that cannot be ignored. If you don't start watching what and how you eat, there may be no hope of recovery.
Dietary recommendations must be followed during drug therapy prescribed by the therapist. Only complex treatment will maximize the speed of recovery of damaged organs and prevent the re-development of the inflammatory process. By the way, to prevent relapse, you will have to follow the rules of proper nutrition for as long as possible.
[13], [14], [15], [16], [17], [18]
Basic rules of dietary nutrition
Dietary nutrition for cholecystitis and pancreatitis is especially important during exacerbation of diseases. Restricting food takes the load off the inflamed organs and helps the body recover in a shorter time. During the first three days from the onset of the attack, the patient must completely refuse food. Only boiled water and a little Borjomi (no more than 200 ml) will be allowed.
After the pain subsides, the patient’s menu expands. He will be allowed unsweetened warm tea, homemade crackers, protein steamed omelet, rice porridge cooked with diluted milk, and pureed vegetable soups. After 7 days, you can add low-fat cottage cheese and stewed vegetables to your diet. Only cabbage is prohibited because it causes gas.
If the reaction of the gastrointestinal tract (GIT) remains normal - the person does not have nausea, vomiting, diarrhea or pain - then you can include dishes such as:
- souffle;
- steamed fish;
- steamed chicken breast or turkey cutlets;
- buckwheat and semolina.
Combined inflammation of both organs is called cholecystopancreatitis. In this case, the patient is prescribed diet No. 5. Its basic principles:
- fractional diet - up to 6 times a day;
- small portions;
- food should be warm;
- the basis of the diet is proteins;
- Only steam cooking, baking in foil and classic cooking are allowed;
- It is allowed to use vegetable or skimmed broths for preparing soups;
- complete avoidance of fried foods, marinades, and caffeine-containing drinks.
Features of the diet for cholecystitis and pancreatitis: menu for every day
19.12.
2017
A diet for cholecystitis and pancreatitis is not just part of the treatment process for these diseases, but a lifestyle that excludes certain foods that can lead to exacerbation.
With proper organization of the dietary regimen, long-term remission is possible. Moreover, the patient’s quality of life is significantly improved, and the person may not feel a lack of preferred food.
General principles of diet for cholecystitis and pancreatitis
Since the digestive organs are inextricably linked anatomically and functionally, a diet for cholecystopancreatitis is recommended taking into account the general severity of inflammation that affects both the pancreas and gall bladder.
Each disease has its own characteristics, moreover, their common etiology (cause) and pathogenesis (disease development) lead to the fact that diet is part of a comprehensive treatment in any period of illness.
Therefore, general principles are used in prescribing a diet for inflammation of the pancreas and gallbladder.
It is based on a power system developed by Professor M.I. Pevzner several decades ago, but is still actively in demand now. It takes into account all types of existing diseases. It takes into account foods that are useful and harmful for each pathology, the nature of their processing and the frequency of food intake.
Nutrition recommendations for cholecystitis and pancreatitis for each day take into account the general condition of the patient and the stage of the disease. At the initial stage, dietary table No. 5p according to Pevzner is prescribed.
Its main goal and principles are to restore the digestive organs after acute inflammatory processes or operations on organs after severe complications and to prevent relapses of diseases.
The diet number depends on the phase of the disease: in the acute period, table No. 5p is prescribed, then the patient is transferred to table No. 5, then No. 1. Which dietary table is used in each time period is determined by the doctor.
Diet can be part of therapy when the patient continues to take prescribed medications, or be an independent method of treatment and prevention. In the latter case, it is especially important in the stage of unstable remission, when the patient’s well-being and condition depend on proper nutrition.
Basic principles of the diet:
- low calorie content;
- limiting fat;
- exclusion of certain products;
- the use of foods containing many vitamins and minerals.
Excluded:
- fatty, fried;
- products that cause flatulence;
- food containing coarse fiber;
- food that has a juice-containing effect increases the production of gastric and pancreatic juice.
In case of exacerbation of cholecystitopancreatitis, it is recommended:
- eating pureed foods;
- The temperature of the food should be comfortably warm;
- portions of each dish are small;
- food intake is distributed 6–8 times a day;
- processed exclusively using gentle methods: stewing, boiling, steaming.
List of products, chemical composition, calorie content of dishes
There is a detailed list of products that are recommended for use in cholecystopancreatitis. When preparing any dish for these diseases, a table is used that contains all the information about the calorie content of foods and their chemical composition.
For pancreatitis and cholecystitis, fats are limited to a minimum and carbohydrate intake is reduced.
This is due to the endocrine function of the pancreas: it produces insulin to break down carbohydrates, so when their content is increased, the load on it increases.
What should you not eat if you have cholecystopancreatitis?
Limiting fats is associated with their high functional load on affected organs and the liver.
To break down fatty acids, a large number of enzymes are required, which increases the functional load on the affected organ. During an exacerbation, only refined oil is allowed to be used in cooking.
You need to know or have on hand when preparing a diet an approximate list of where you can find any prohibited product.
It includes:
- fried, pickled, smoked, spicy food;
- canned and sausage products;
- fatty broth with a high content of extractive substances that have a juice effect;
- fresh vegetables and fruits;
- eggs (yolk is strictly contraindicated);
- strong coffee, tea, desserts with rich cream, chocolate, cocoa, ice cream;
- carbonated drinks;
- buns, cakes, freshly baked bread.
You should not eat legumes; dairy products, including fresh whole milk, are also excluded. At no stage of the disease should you drink alcohol or low-alcohol drinks. They are the main risk factor and cause exacerbation.
Any spicy product can cause severe pain, and chronic gastritis will worsen. This leads to an even greater deterioration of the condition: the secretion of gastric juice increases, its high acidity provokes the secretion of pancreatic enzymes, which in large quantities affect the condition of nearby organs.
Existing gallstone cholecystitis is caused by biliary pancreatitis - a secondary disease that affects an adult, more often a woman (in 60% of cases). This is explained by a higher incidence of stone formation in women than in men, and the development of cholelithiasis (GSD) in them.
This is due to poor nutrition - eating large amounts of fatty and fried foods. This pathology is not observed in the child. Stones interfere with the flow of bile into the bile ducts, or it backflows into the pancreatic ducts.
This causes severe inflammation of the pancreas due to the proteolytic components present in the bile. The symptoms of the disease are similar to the clinical manifestations of other diseases of the digestive system, such as gastroduodenitis and colitis.
The disease progresses rapidly, weight loss is observed - a sign of deep digestive disorders, fat processing and lack of vitamins.
Removal of the gallbladder for cholelithiasis or strict adherence to a diet is part of the treatment of this pathology.
In many cases, a removed gallbladder provokes increased inflammation and swelling of the pancreas, so strict adherence to proper nutrition is required.
They may prohibit sugar and sweets if diabetes is detected, fresh wheat baked goods, black bread, and limit salt to 10 g per day.
Pregnancy significantly complicates cholecystopancreatitis, especially in the first trimester. Due to early toxicosis, it is difficult to differentiate digestive pathology. But the fetus is not at risk if the diet is followed.
During this period, you need to be careful about changing taste preferences: shrimp or other exotic seafood can suddenly worsen the condition and increase nausea and vomiting.
Before starting to use new products, you need to anticipate possible complications and start taking them in small quantities.
Cholecystitis and exacerbation of pancreatitis: what can you eat?
Exacerbation of cholecystitis and pancreatitis is accompanied by pain and dyspeptic symptoms. During this period, active drug therapy is carried out, and fasting and rest are recommended for the first days. Eating restrictions, depending on the severity of the patient’s condition, may be prescribed for 3 to 5 days. Treatment is carried out in a hospital, and if vomiting and diarrhea are moderate, drinking is prescribed:
- non-carbonated alkaline mineral water (Borjomi, Smirnovskaya, Slavyanovskaya);
- rosehip decoction;
- fruit compote;
- jelly;
- Not strong brewed tea.
Nutrition is carried out parenterally - intravenous administration of nutrient solutions, which are selected for each patient individually.
From the 5th day, it is allowed to eat a small amount of food within the limits of table No. 5p - pureed option: all food must be grated until it has the consistency of a puree or a mushy appearance.
The essence of the diet: minimize the irritating chemical, mechanical and thermal effects of food on the gastric mucosa and affected organs.
The menu includes: permitted vegetable, pureed millet soup, porridge (rice, buckwheat, oatmeal and semolina). Vegetables are recommended boiled, in small portions:
- beet;
- zucchini;
- carrot;
- potato.
Gradually the diet expands, allowing:
- lean meat and fish;
- egg whites;
- low-fat fermented milk products.
Goat cheese - feta cheese is especially useful: a minimum of fat, soft consistency, two-month aging, and easy digestion make it a useful dietary product for cholecystopancreatitis.
It does not cause increased production of gastric juice, which is important for patients with this pathology.
A good review from nutritionists allows it to be widely used in the menu: the elderly or children are not an exception.
Diet during remission of the disease
During the period of remission of cholecystopancreatitis, table No. 5B is prescribed - it is considered as a type of diet No. 5p. Designed for:
- for patients in remission of the disease;
- to prevent relapses and progression of the inflammatory process;
- correction of emerging nutritional disorders.
The principle remains:
- grinding food;
- temperature regime (food – warm, comfortable temperature);
- fractional intake (often in small portions);
- gentle cooking - stewing in steam, water.
Table 5B is considered a diet of increased energy value. It increases the content:
- proteins (up to 110 g);
- fats - the allowed amount is brought to the lower limit of the norm (20% of them should be vegetable), introduced gradually;
- carbohydrates - 350–400 g, but simple carbohydrates are still limited to 30 g per day.
Allowed:
- pureed vegetable and milk soups with the addition of cream and milk;
- yesterday's wheat bread and biscuits;
- lean meat;
- lactic acid products, low-fat or low-fat, milk due to poor tolerance is added to dishes - cereals, soups, omelettes;
- vegetables - boiled;
- apples - baked, jam, jelly.
Contraindicated:
- spicy seasonings;
- extractives;
- strong broths;
- smoked meats;
- salo;
- fresh white cabbage;
- alcohol, coffee, chocolate, strong tea.
Permitted and prohibited products are specified using special tables.
Sample menu for the week
When compiling a diet, the whole week is planned out: the presence and amount of proteins, fats and carbohydrates in the menu are calculated using special tables. Meals are provided six times a day, including snacks - second breakfast and afternoon snack.
Sample menu for one day:
- Breakfast: oatmeal on water with jam, crackers, weak tea.
- Second breakfast: apple baked with cottage cheese, compote.
- Lunch: rice soup, boiled chicken breast, boiled beets in the form of a salad, seasoned with vegetable oil, rosehip infusion.
- Afternoon snack: a portion of noodles with cheese, dried fruit compote.
- Dinner: a glass of kefir.
The menu for the week is prepared in a similar way, using recommended products. Tables indicating caloric value and a list of permitted foods are used.
Recipes for dishes with joint diseases
There are various recipes from that small list of approved products that can be used for cholecystopancreatitis.
Potato cutlet recipe
To 7 grated potatoes add 200 g of finely chopped milk sausage, 200 g of low-fat cheese, grated on a fine grater. The mass is thoroughly mixed with the addition of 3 raw eggs, 2 tablespoons of flour, salt and green onions to taste. Cutlets are formed from the resulting homogeneous mass. Prepared in a double boiler.
Vegetable soup recipe with cheese meatballs
Mixable:
- 100 g grated cheese;
- butter;
- 100 g flour;
- 1 raw egg.
The resulting mass is kept in the cold for 30 minutes.
Bouillon:
- 1 grated carrot;
- 1 chopped bell pepper;
- 5 chopped potatoes;
- 1 onion, diced.
Boil for 15 minutes in 2.5 liters of water.
Bean-sized meatballs are formed from the cheese mass and thrown into the resulting broth.
Potato omelette recipe
- 200 g boiled potatoes;
- 4 beaten eggs with added salt;
- 100 ml milk;
- 50 g hard cheese.
Grated boiled potatoes are placed on film on the bottom of a double boiler, poured with beaten eggs and milk, sprinkled with cheese, and cooked for 30 minutes.
Nutritional habits should be discussed with your doctor. Diet is always a factor in the stability of good condition in cholecystitis and pancreatitis.
- Liir G. Important triad: liver, bile ducts, pancreas. All about research, treatment, optimal nutrition. M. publishing house UnicumPress, publishing house "INFRA-M" 2003
- Ivashkin V.T., Shevchenko V.P. Nutrition for diseases of the digestive system: Scientific publication. M. GOETAR-Media, 2005
- Samsonov M. A. Criteria for assessing the differentiated use of diet therapy. Bulletin of the AMN. 1986 No. 11 pp. 42–49.
- Fomina L.S. The influence of the nature of nutrition on the secretory activity of the pancreas. Nutrition Issues 1966 No. 5 pp. 22–23.
Source: https://pankcreatit03.ru/dieta-pri-holetsistopankreatite.html
List of permitted products
Products that can be safely included in the menu for cholecystitis and pancreatitis should contain a high percentage of proteins and a minimum of fat.

Dietary food developers recommend:
- Lean meats. Meat is the main source of protein. It is allowed to eat beef, veal, chicken (the skin is first removed), turkey and rabbit. It is boiled or steamed. Adding salt to dishes is allowed, but in moderation.
- Low-fat fish. It is allowed to be served in the form of a soufflé, aspic, boiled or steamed.
- Slightly stale bread. It is allowed to serve crackers, toast, and yesterday's bread. It is allowed to cook pies with fish or cottage cheese, but baking is not used during the dough kneading process.
- Fermented milk, dairy products. The menu may include low-fat cottage cheese, low-fat yogurt, kefir, sour cream (limited).
- Eggs. Served as a steam omelette or cooked soft-boiled.
- Cereal products. Buckwheat, oatmeal, rice and semolina are allowed. Served as a separate dish or as a side dish.
- Soups. Prepared in vegetable and second meat broths.
- Vegetables. You can eat it in the form of steamed or simply boiled dishes.
- Vegetables and fruits with a sweet taste. It is good to bake apples and pears in the oven. You can serve dried fruits.
- Soufflé, marshmallows, caramels. Honey and jam are allowed in small quantities.
- Oil. Creamy and vegetable products are allowed, but in limited quantities.
What diet is needed for pancreatitis and cholecystitis
Diet for cholecystitis and pancreatitis is the most important component of therapy. Requires strict adherence to the principles of dietary nutrition, as well as the rules of cooking, menu planning and eating. Without this, the recovery of patients is impossible.
Table No. 5 - basic principles
Diet number 5 for cholecystitis and pancreatitis prescribes compliance with specific rules when creating a menu for the week, preparing and eating food. Patients need to adhere to certain principles:
- Eat meals regularly to ensure adequate nutrition. There should be 3 main meals and 2 snacks per day.
- Don't overeat.
- Not to starve.
- Exclude from the menu foods that are difficult to digest and create a burden on the gastrointestinal tract, for example, mushrooms.
- Do not eat foods that contain too much coarse fiber and dietary fiber.
- Eat small portions. The volume of one should be no more than 250 g.
- Eat exclusively warm food, the temperature of which does not exceed 50 degrees.
- Prepare dishes by boiling, stewing, steaming.
- Stop drinking alcoholic beverages.
- Limit your coffee consumption.
In essence, these are the basic principles of nutrition that all patients must follow in order to avoid exacerbations of pathologies.
Permitted and prohibited products
Patients with chronic or acute cholecystitis or pancreatitis will have to stop eating certain foods. Even if you eat something from the list of prohibited foods just once, the negative consequences will not take long to appear. There is a list of products allowed for consumption.
What to remove from your diet
Patients need to remove the following from the diet menu:
- semi-finished products;
- porridges, instant soups, which are simply brewed with boiling water;
- fast food;
- fatty, spicy, salty foods;
- fried foods;
- sharp and salty varieties of cheese;
- dairy products with a high proportion of fat;
- baked goods, puff pastries;
- rich broths;
- sour berries, fruits, vegetables;
- ice cream;
- chocolate;
- confectionery;
- smoked meats;
- mushrooms;
- canned food;
- onion garlic;
- legumes;
- salo;
- alcoholic and carbonated drinks.
All of these products require complete rejection. Even a minimal amount can provoke unpleasant consequences, exacerbation of cholecystitis and pancreatitis.
What can be included in the menu
During nutrition for cholecystitis and pancreatitis, you can consume:
- porridge cooked with low-fat milk;
- vegetable first and second courses;
- lean varieties of fish and meat;
- fermented milk products with a low percentage of fat;
- steam omelette or baked in the oven;
- pasta;
- vegetables, fruits, berries, but not sour;
- biscuits, crackers without salt;
- Rye bread;
- green or herbal tea.
All of the above can be safely included in your daily therapeutic diet and not be afraid of the consequences.
Features of the use of certain products
When choosing meat and fish, you need to pay attention only to low-fat varieties. These products are mandatory, they are necessary for the human body.
Among vegetables, choose broccoli, cauliflower, zucchini. Other types are available if the body tolerates them normally. Carrots should be grated before adding to dishes.
The number of eggs should be limited; it is enough to eat no more than 2 eggs per week. At the same time, it is better to prepare a steam omelet from them; there is no need to use them hard-boiled.
Eat pasta well boiled and add it to casseroles and soups. It is advisable to eat potatoes mashed. You can eat semolina, but not as an independent dish, but put it, for example, in a cottage cheese casserole.
Sweets should not be consumed, but this restriction leads to the fact that a person constantly feels some kind of lack of nutrition, as if something is missing. To prevent this, doctors advise including berry jellies, jelly, and compotes in the menu.
You can eat honey, but in minimal doses - 2 tsp. per day, dissolving them in warm water or rosehip decoction. Then it will benefit the patient’s body, provoke the production of enzymes necessary for digestion, and normalize the functioning of the gallbladder and pancreas. In addition, the bee product can suppress inflammation.
How to eat in case of exacerbation?
When a person experiences a period of exacerbation, he begins to suffer from severe pain. General weakness appears, lack of desire to eat, and health worsens. Therefore, doctors prohibit eating for 3-5 days, only drinking water.
Fasting is practiced, due to which the production of pancreatic enzymes, which occurs in large quantities in the first few days of the acute period, is reduced.
After the exacerbation subsides, the patient is gradually transferred to a diet. First, you need to drink more; weak or herbal tea, rosehip decoction, and jelly are recommended.
When the pain completely subsides, they begin to eat, introducing soups into the diet. And only after 2 months the attending doctor prescribes the patient to follow diet No. 5.
Recipes of allowed dishes
You can include the following dishes in the menu for pancreatitis and cholecystitis.
Pumpkin dessert
To prepare, cut the vegetable pulp into cubes and place them in a double boiler. If desired, you can add a little sugar and cinnamon. Then cook for 20 minutes, then pass the pumpkin through a blender to obtain a mushy consistency.
Vegetable soup
To prepare, prepare the following ingredients:
- 500 ml water;
- half a carrot;
- half an onion;
- 4 potatoes;
- greenery;
- a pinch of salt.
Cut the potatoes into cubes, put them in water and put them on the stove to cook. At this time, chop the carrots, after 5 minutes add to the potatoes. Chop the onion, fry a little in vegetable oil, then add it to the broth when the vegetables are cooked.
Finally, throw in a pinch of salt and herbs.
Omelette
Ingredients for preparation:
- 200 g boiled potatoes;
- 4 eggs;
- 100 ml low-fat milk;
- a little bit of cheese;
- greenery;
- a pinch of salt.
Grate potatoes and cheese. In a separate bowl, beat eggs with milk, add salt. Cover the steamer with film, lay out a layer of grated potatoes, and pour in the milk-egg mixture. Sprinkle cheese on top and cook for 25 minutes.
Oatmeal jelly
The drink is very simple to prepare, but it has enormous benefits for the body. You need to take 3 tbsp. oatmeal, pour 2 glasses of water, put on the stove and cook until the consistency of the liquid resembles thick jelly.
Consequences of not following the diet
Diet is an essential component of the treatment of cholecystitis and pancreatitis. Without it, it is impossible to normalize their functioning and get rid of unpleasant manifestations.
Even if the patient strictly follows the medication regimen, but eats prohibited foods, the chance of recovery will decrease significantly. Violation of the dietary regime will lead to an exacerbation of diseases, the patient will suffer from symptoms.
Thus, diet in the event of cholecystitis and pancreatitis in adults is the most important component of treatment, without which no patient can do. It’s hard to give up your favorite food, but this is the only way to have a chance of recovery.
Source: https://puzyr.info/kakaya-nuzhna-dieta-pri-holetsistite-i-pankreatite/
List of foods to exclude
What you can eat for these diseases is now known. But what is it forbidden to eat? The list of products that are prohibited is represented by the following items: strong brewed black tea, coffee, drinks with gases, alcohol (it can become a provoking factor for exacerbations of any of the pathologies).
Lard and fatty meats are also prohibited. The latter includes pork. The animal fats contained in the product make the digestive organs work harder, stimulating the production of bile and pancreatic juice. Limited to:
- Fresh baked goods.
- Rich meat broths.
- Mushrooms. Broths made from them are completely prohibited, as are the mushrooms themselves.
- Vegetables that irritate the gastric mucosa. These are onions, garlic, sorrel, radishes.
- Chocolate and cream.
- Sauces, seasonings with a spicy taste.
- Smoked and salty. They have an irritating effect on the mucous membranes of the stomach, are difficult for the body to absorb, and cause indigestion.
Grocery list
For cholecystitis and pancreatitis, foods that are rich in protein and contain a minimum of fat are selected. Food for cholecystitis and pancreatitis should be as soft and gentle as possible for the body.
Permission

Kefir for pancreatitis and cholecystitis is a source of protein. Doctors recommend drinking at least a cup of this drink daily. The main supplier of protein to the body is meat. It cannot be excluded from the diet. You can choose only low-fat varieties:
- beef;
- skinned chicken;
- rabbit meat;
- turkey.
It can be consumed boiled or in the form of minced meat cutlets cooked in a double boiler. No condiments, sauces or spices! You can just add a little salt.
Dairy products allowed, in addition to kefir, are a little sour cream and low-fat yogurt. Eat low-fat cottage cheese. At the same time, cheese, fermented baked milk, full-fat milk, and cream are excluded from the diet.
Lean fish is also allowed. It is steamed, boiled, made into aspic or soufflé. You will have to exclude salted, smoked and grilled fish. Canned food in oil should also not be eaten.
You can eat bread - but only stale bread (for example, yesterday's bread), and also in the form of toast and crackers. You can sometimes treat yourself to a savory pie with cottage cheese or fish filling.
Eggs are allowed, but only soft-boiled or in an omelet - no more than a couple of yolks per day. The following are acceptable cereals:
- oatmeal;
- rice;
- buckwheat;
- semolina.
All this is in the form of side dishes or porridges. You can also eat soups with vegetable broth. However, frying in oil will have to be excluded.
Almost any vegetables are eaten, but only baked without spices or steamed. The amount of fresh vegetables will have to be reduced.
Your doctor will tell you what fruits you can eat. Basically, any non-acidic fruits (as well as berries) are allowed, in particular baked pears and apples, as well as compotes and dried fruits. It is advisable to remove fresh fruits from the diet, at least during an exacerbation.
Some of the sweets are acceptable in moderate quantities:
- jam;
- honey;
- sugar;
- marshmallows;
- caramel;
- souffle.
Vegetable oil or butter is allowed, but in very moderate quantities.
Prohibition
For pancreatitis and cholecystitis, foods that complicate digestion and aggravate these diseases are prohibited. For example, alcohol provokes exacerbation of inflammation. Having a negative effect on the body as a whole, it, among other things, disrupts the activity of the pancreas and intestines.

Any fatty foods, for example, specific types of meat and lard, complicate digestion. Because of them, the body produces more pancreatic juice and bile. And this is very harmful. Any fresh baked goods are a serious test for the gallbladder and pancreas.
You should not drink strong coffee if you have cholecystitis and pancreatitis.
It is generally accepted that chicken broth is healing for any disease. It should strengthen and give strength. But it is not so. Rich broth with any meat is harmful to the pancreas. You will have to completely abandon fatty broths.
Fungi in these diseases is a controversial issue. Some experts consider them dietary, while others consider them absolutely harmful to digestion. It is recommended to eat only mushroom caps. It is better to avoid mushroom soups.
It is not recommended to eat sour vegetables, as well as those that irritate the mucous membrane in the stomach:
- green onions;
- sorrel;
- radishes and so on.
Sweets such as cream and chocolate have a bad effect on the gallbladder and pancreas. Most other sweets are also harmful. You can tell whether a particular food is prohibited by the characteristic nausea after eating even a small amount.
Hot sauces with seasonings, as well as any smoked foods and pickles are strictly prohibited. They often provoke severe pain. Poorly digested, these products lead to indigestion and disruption of the pancreas and intestines.
Diet for acute pancreatitis
During the period of exacerbation of the pathology, the patient develops severe pain and has no desire to eat. The patient's health deteriorates significantly. During the first 3–5 days, therapeutic fasting is recommended. During this period, the patient can only drink. It should be water without gas.
After the pain subsides, the menu can include vegetables crushed to a puree, soups thickened with cereals - they need to be cooked only in water, vegetable broths without salt and spices. When cooking soups, you can use oatmeal or buckwheat. During an exacerbation, you should not eat millet, egg and corn grits. In chronic diseases, these types of cereals should be limited as much as possible.
As the condition stabilizes, the menu can be expanded to include boiled veal and chicken. The patient begins to be served oatmeal cooked in water and mashed potatoes. Before serving, it is diluted with broth to form a puree soup. Salting and adding milk to these dishes is strictly prohibited.
After 14 days from the onset of the attack, the diet may include low-fat dairy products. The best choice would be milk or kefir. Cottage cheese is allowed, but in limited quantities. Porridge can now be cooked with milk diluted with water. You can eat steamed vegetables. A decoction of rose hips is served as a drink.
If unpleasant symptoms appear - nausea, vomiting, pain - you must immediately exclude the foods that caused the disease to worsen. 2 months after the exacerbation, the patient is prescribed a special dietary food - table No. 5P. It is typically low in fat and carbohydrates. Meals should be fractional up to 6 times a day.
Diet for cholecystitis and pancreatitis is part of the treatment of these serious diseases. If you don't follow a diet, forget about the effectiveness of medications. And this is understandable, because the pancreas, together with the gallbladder, play one of the main roles in the digestion of food. In view of this, treatment of cholecystitis and pancreatitis must necessarily be accompanied by dietary restrictions.
And for this purpose, a special diet has been created, containing a list of foods allowed for consumption and those that are prohibited. But it differs at different stages of pancreatic disease. If it is acute pancreatitis, certain approaches are needed, but if it is chronic, completely different ones are needed.
Diet for cholecystopancreatitis involves
Most likely, a diet for pancreatitis and cholecystitis will never cure these diseases - it would be foolish to delude yourself. But it is definitely capable of easing a person’s daily condition, preventing the development of the disease and deterioration of well-being. It’s not for nothing that they say, “We are what we eat.” While we eat unimportant food of poor quality, artificial, heavy, we feel unwell, and when we switch to a healthy diet, our own health improves and strengthens.
A diet for cholecystitis and pancreatitis will greatly help those who suffer from these diseases. Cholecystitis, or inflammation of the gallbladder, most often occurs when there are stones in the gallbladder. As a rule, this happens due to the fact that the outflow of bile is disrupted. This is facilitated by poor nutrition, namely its irregularity, frequent overeating, and constant constipation. Cholecystitis also occurs in people with a sedentary lifestyle, having an infection, or in pregnant women.
Pancreatitis, that is, inflammation of the pancreas, occurs in people who are under constant stress, who do not follow a diet, and especially in people who eat a lot of meat and fatty foods. What do you need to know when following a diet for cholecystitis and pancreatitis? So: meals for pancreatitis and cholecystitis should be fractional and frequent once a day; the total daily weight of food consumed should not exceed .5 kg; daily rate of water consumption - .5 l; We focus on protein foods, and the amount of fats and carbohydrates should be kept to a minimum; Take food only in boiled and steamed form, exclude marinated, smoked, fried and salted foods; replace rich soups based on fatty meat and fish broths with lean soups made with water; You can eat lean meat, poultry, low-fat dairy products, scrambled eggs, soft-boiled eggs no more than 2 pieces per week, vegetables, sweet fruits and berries, pure unheated vegetable oil, flour products excluding butter dough, stale bread, no more g per day of butter, no more than 70 g of sugar per day, including in any dishes; You should forget about such products as legumes, mushrooms, fatty meats, chocolate, cocoa, pastry, canned food, spices.
All kinds of cereals, stewed vegetables, and low-fat fermented milk products are perfectly digestible. But it is better to avoid dishes made from cabbage and eggplant, especially during an exacerbation period. A complete replacement for fatty soups would be light vegetable soups with cereals, zucchini, cauliflower, seasoned with sour cream or cream. Breakfast: steam omelette, but only from proteins alone, buckwheat porridge in any form, simply boiled or with milk, but always pureed, tea with lemon or with the addition of milk.
Nutrition for diseases such as cholecystitis or pancreatitis should a priori be healthy! This means that, at a minimum, this diet should be dominated by fresh vegetables, as well as low-fat meat and dairy products, and cereals. Diet for cholecystitis and pancreatitis: basic principles A diet for cholecystitis and pancreatitis will greatly help those who suffer from these diseases.
Diet for cholecystitis and pancreatitis: one-day menu For example, we can give this schedule for one day of the diet for cholecystitis and pancreatitis. Afternoon snack: apples, baked and preferably without added sugar. Dinner: cottage cheese soufflé, tea with lemon, it calms the pancreas well. At night: jelly from juice or low-fat kefir.
During exacerbation
The principles of nutrition for cholecystitis and pancreatitis when an exacerbation occurs are aimed at bringing the organ to a state of rest, in which it can recover as quickly as possible. For cholecystopancreatitis, the diet is strict and even involves some fasting. Her principles of what is not allowed and what is allowed:
- Nutrition in acute pancreatitis of the pancreas is completely excluded in the first 3 days. The patient can only drink plain still water after preliminary boiling.
- After 3 days, if stomach pain does not bother you, take some dishes in small portions. This will be pureed vegetable soup without frying, croutons, steamed egg white omelet, oatmeal, rice porridge with a mixture of milk and water.
- On the seventh day, the diet for exacerbation of pancreatitis is made even more varied. You can already eat stewed vegetable dishes and low-fat cottage cheese.
Monitor the condition of the body during such a diet. If the pain does not intensify, new symptoms are not added, steamed fish or meat cutlet, soufflé, lean fish, buckwheat, semolina are included in the diet.
Such restrictions last 1-2 months, after which they switch to the 5p table, which is observed for at least a year.
Due to the fact that during exacerbation of pancreatitis with cholecystitis, severe pain, deterioration of health, nausea, and weakness are observed, it is recommended to start fasting. But it is important to do it correctly. The main recommendations for treatment are as follows:
- It is recommended to eat fractionally, dividing into 6 meals;
- during exacerbation of pancreatitis, it is better to use products for cooking. which are easy to puree;
- reduce the intake of lipids from food and increase the protein content;
- exclude the consumption of fatty, salty, fried foods;
- Not only do you need a diet for cholecystitis and pancreatitis, as well as drinking plenty of fluids - still water and rosehip decoction are better suited for this.
Cholecystitis and exacerbation of pancreatitis: what can you eat?
Exacerbation of cholecystitis and pancreatitis is accompanied by pain and dyspeptic symptoms. During this period, active drug therapy is carried out, and fasting and rest are recommended for the first days. Eating restrictions, depending on the severity of the patient’s condition, may be prescribed for 3 to 5 days. Treatment is carried out in a hospital, and if vomiting and diarrhea are moderate, drinking is prescribed:
- non-carbonated alkaline mineral water (Borjomi, Smirnovskaya, Slavyanovskaya),
- rosehip decoction,
- fruit compote,
- jelly,
- Not strong brewed tea.
Nutrition is carried out parenterally - intravenous administration of nutrient solutions, which are selected for each patient individually.
From the 5th day, it is allowed to eat a small amount of food within the limits of table No. 5p - pureed option: all food must be grated until it has the consistency of a puree or a mushy appearance. The essence of the diet: minimize the irritating chemical, mechanical and thermal effects of food on the gastric mucosa and affected organs. The menu includes: permitted vegetable, pureed millet soup, porridge (rice, buckwheat, oatmeal and semolina). Vegetables are recommended boiled, in small portions:
Gradually the diet expands, allowing:
- lean meat and fish,
- egg whites,
- low-fat fermented milk products.
Goat cheese - feta cheese is especially useful: a minimum of fat, soft consistency, two-month aging, and easy digestion make it a useful dietary product for cholecystopancreatitis. It does not cause increased production of gastric juice, which is important for patients with this pathology. A good review from nutritionists allows it to be widely used in the menu: the elderly or children are not an exception.

In case of chronic course
The diet for pancreatitis and chronic cholecystitis is also called “table 5p.” A special feature is the increased protein content, minimum carbohydrates and fats. What you can eat for cholecystitis and pancreatitis should generally have the following characteristics:
- daily calorie intake does not exceed 2800 kcal;
- carbohydrates will be up to 400 g, proteins - 120 g, and fats - up to 80 g;
- A diet for chronic cholecystopancreatitis involves consuming up to 1 tbsp. spoons of sugar;
- replace sucrose with sorbitol or xylitol;
- It is recommended to drink 2.5 liters of water per day;
- It is allowed to consume up to 250 g of day-old white bread.
Diet for pancreatitis: creating a sample menu
Diet for cholecystopancreatitis suggests. Test question: Nursing Accreditation question. The causes of diabetes are all except. Modifiable factors in the development of atherosclerosis include all except. Non-modifiable factors contributing to the development of prostate adenoma are: Diabetes mellitus in the human body. In Russia, with the active promotion of a healthy lifestyle, it is expected by the year.
Most likely, a diet for pancreatitis and cholecystitis will never cure these diseases - it would be foolish to delude yourself.
WATCH THE VIDEO ON THE TOPIC: DIET FOR PANCREATITIS. DETAILS ABOUT DISHES AND PRODUCTS. MENU AND RECIPES. #healthy_help #healthy_help
Principles of the 5p table.
The diet for cholecystitis and pancreatitis or the 5p table involves something more than the above principles. Let's consider additional rules:
- The food is warm. Recommended temperature is 40 degrees.
- The diet for every day should be such that the total weight of food is up to 3 kg.
- Avoid pickled foods, fried and salty foods. For pancreatitis, eat only dietary foods.
- Vegetables cannot be eaten raw. It is recommended to steam it.
- For drinks, it is recommended to drink chicory infusions.
- Eat eggs 2 times a week boiled or scrambled.
- Prepare vegetable soups using dietary broths.
When planning your diet, it is recommended to include foods containing fiber. It is also recommended to use low-fat natural yogurt or kefir.
When choosing a method for processing food during the cooking process, it is recommended to steam, stew, or bake. Avoid frying completely. As for what fruits you can eat with pancreatitis, these will be baked apples, pears and other light foods that are not raw. It is recommended to sharply reduce the amount of sweets in your diet and not consume salt.
Do's and Don'ts
Of course, for pancreatitis and cholecystitis, the diet is strict, but it presupposes the possibility of consuming many foods. The list of food products is as follows:
- yesterday's dry white bread;
- beet;
- zucchini;
- potato soup and other vegetarian soups;
- lean chicken meat (for example, boiled chicken breast);
- steamed egg white omelettes;
- buckwheat, semolina, oatmeal, rice porridge;
- potatoes, green peas, carrots;
- heat-treated mixture of pumpkin and apples;
- boiled vermicelli;
- non-sour fruits in grated form;
- compotes;
- rosehip green tea, compotes;
- refined vegetable oil - up to 1 tbsp. spoons (for example, a decoction of vegetables in the form of soup with sunflower oil);
- cottage cheese, kefir;
- You can also use sauerkraut for pancreatitis, if it is not sour;
- greens, etc.
What not to eat if you have pancreatitis:
- Rye bread;
- alcohol;
- puff pastry;
- baking;
- fresh bread;
- meat and fish broths;
- milk soups (fresh milk is contraindicated for pancreatitis);
- fresh cucumbers, cucumber and tomato salad;
- smoked meats, fatty foods;
- borscht, okroshka; millet, corn, wheat porridge;
- legumes;
- cabbage;
- radishes, onions, garlic;
- bell pepper, eggplant;
- dried fruits;
- spinach, sorrel;
- spices;
- mushrooms;
- cocoa, coffee, etc.
Of course, the list is far from complete. For example, some are interested in using honey for pancreatitis, others are trying to understand whether it is possible to eat bananas, persimmons, nuts and other foods.
Let's look at some controversial points:
- As for whether bananas are ok for pancreatitis and cholecystitis, most doctors allow this product. But it is recommended to consume 1 piece per day or less. For example, when making low-fat yogurt, pie or casserole, you can add this fruit there. It is also recommended to drink banana juice in small quantities.
- Can you eat nuts if you have pancreatitis? Due to the fact that this is a source of omega fatty acids, which are essential, these products are worth consuming, but only after the exacerbation has been relieved. Nuts protect pancreatic tissue from destruction and replenish the daily fat requirement. But you can take up to 15 g per day even if you are not allergic to them.
- Is it possible to eat honey for pancreatitis and cholecystitis? Yes, this product is allowed if the patient does not additionally suffer from diabetes. For cholecystitis, honey helps get rid of excess bile. But it is recommended to use it in the morning and no more than a tablespoon.
- Also, many people are interested in whether it is possible to eat persimmons with pancreatitis. This product is not recommended, especially during an exacerbation.
Diet for acute and chronic forms of the disease

In advanced forms of pancreatitis and cholecystitis (acute, chronic), a person must learn to consciously exclude certain foods from the diet. These include:
- meat, mushroom broth;
- fried potatoes;
- porridge (yachka, millet, corn, pearl barley);
- radishes, cabbage;
- raspberries, strawberries, other acid-containing berries, fruits, vegetables;
- freshly prepared bread, pastries;
- alcoholic drinks, strong tea, coffee, cocoa;
- spicy seasonings, ketchups.
If you have pancreatitis or cholecystitis, you should not completely give up foods, but reasonable measures are required in your diet. If the disease has transitioned from a chronic to an acute stage, then the above list of products should not be consumed! As your health condition normalizes, during remission of pancreatitis, you can consume a little of your favorite product.
Table No. 5

To slow the progression of cholecystitis and pancreatitis, follow a diet called table No. 5. Your organs have lost their natural ability to work together, but you can eliminate pain by balancing your diet. The diet for chronic pancreatitis and cholecystitis consists of unloading the gallbladder and pancreas. The diet is divided into many parts. All products are baked or boiled and steamed until cooked.
The main thing in the treatment of pancreatitis or cholecystitis is a balanced diet with minimizing fats, carbohydrates, and increasing the amount of protein. For digestive diseases, according to table No. 5, it is useful to use:
- porridge (rice, buckwheat, oats, semolina, others);
- yesterday's bread, unsweetened pastries;
- vegetables in the form of stew or puree (broccoli, potatoes, green peas, pumpkin);
- baked fruits (pear, apple);
- a small amount of dried fruits;
- boiled meat, lean fish;
- soft-boiled egg or without yolk;
- low-fat fermented milk products;
- salt no more than ten grams per day;
- butter 30 grams;
- vegetable oil 15 grams;
- rosehip decoctions, weak tea, non-acidic berry and fruit mousses.
Delicious recipes
Due to large restrictions, it is necessary to completely review your menu for pancreatitis or cholecystitis. This means that you will need to search for new recipes with approved products.
It is recommended to look for recipes for various dishes for pancreatitis and cholecystitis so that the diet is varied and contains a variety of products:
Potato cutlets. To prepare, you need to peel 7 potatoes, boil them and grate them. The resulting mass is mixed with milk sausage and hard cheese (250 g each) in crushed form. And also add 3 eggs, herbs, salt to taste and a little flour. Form a mass from which cutlets are made. They are steamed in a double boiler.
Vegetable soup and cheese meatballs. To prepare the dish, make 2.5 liters of vegetable broth and set it to warm up. At this time, grate cheese (about 100 g), mix with a small amount of butter, 100 g of flour and one egg. Also add a little herbs and salt. Mix all this and put it in the refrigerator for half an hour. At the same time, cut 5 potatoes into cubes, 1 pepper into strips and grate the carrots. Vegetables are boiled for 15 minutes in water, after which the meatballs are placed in the soup until cooked.
It is useful to make pumpkin dishes. They will be varied, and with pancreatitis this is a big advantage. Consider a recipe for casserole with apples and pumpkin. To do this, peel 600 g of pumpkin and grate it. The same steps are repeated with 200 g of apples. After this, place 10 g of butter in a frying pan and simmer the pumpkin and apples. Make a puree from the mixture, add 100 ml of milk and put it on the fire until it boils. Next, pour 60 g of semolina there and hold for another 8 minutes. Remove the product from the heat, cool to 60 degrees, then add one egg and tbsp. spoon of sugar. The resulting mass is placed on a baking sheet, which is previously greased and filled with breadcrumbs, and then baked.
So, even with a huge number of restrictions, the diet for pancreatitis turns out to be quite varied.
Both pancreatitis and cholecystitis are serious diseases of the gastrointestinal tract. In the first case, we are talking about damage to the pancreas, and in the second, to the gallbladder. Diseases are provoked by the same reasons, they can aggravate each other. Sometimes they are called in one word - cholecystopancreatitis. When such a diagnosis is made, the patient is prescribed a diet. With cholecystopancreatitis, the diet fundamentally determines the patient's condition.
Basic rules of nutrition for cholecystitis and pancreatitis

If you have diseases of the gallbladder (cholecystitis) or pancreas (pancreatitis), then to maintain optimal health you need to adhere to basic nutritional rules to prevent the progression of diseases. The famous therapist M.I. Pevzner advises sticking to a diet that excludes:
- binge eating;
- roast;
- spicy;
- smoked;
- pickled;
- acid-containing substances in products;
- meat broths;
- hot or cold food;
- consumption of alcoholic and carbonated drinks.
If you have pancreatitis or cholecystitis, eat in small portions, if possible, more often than usual. If the dish is pieces, chew them thoroughly. To better digest food during pancreatitis, use steamed, boiled or baked food, but without a rough crust. For cholecystitis or pancreatitis, limit the intake of fats and carbohydrates, and the use of proteins is encouraged. It is advisable to eat about three kilograms of food per day and drink up to 2.5 liters of liquid.
Causes
The causes of such ailments lie in poor nutrition. People who regularly consume fatty, smoked, and spicy foods are at risk. Also at risk are those who eat irregularly - with long breaks. Therefore, a diet is required for chronic cholecystopancreatitis.

However, sometimes this disease also occurs due to gallstones. But their appearance is also provoked by improper nutrition. In addition, an unbalanced diet leads to calculous cholecystitis. It is noteworthy that exacerbations of pancreatitis occur against the background of chronic alcoholism very often, while the gallbladder does not become inflamed for this reason.
Nutrition during a fading exacerbation
The diet for chronic pancreatitis during the attenuation of the exacerbation stage pursues the goal of biochemical and mechanical sparing of the mucous membrane. Therapeutic nutrition includes:
- control of the level of carbohydrates, lipids, proteins;
- exclusion of spices, smoked meats, spicy foods;
- consumption of water-soluble vitamins;
- exclusion of seasonings;
- use of fat-soluble vitamins.
The diet for the attenuation of exacerbation of chronic pancreatitis allows the consumption of small pieces of food. The temperature of the food should not exceed 60 degrees. It is advisable to eat no more than 6 times a day.
The content of a daily serving of protein varies from 40 to 90 g, fat - from 30 to 80 g, carbohydrates - from 60 to 300 g. Calorie content should not exceed 2.5 thousand kcal.
During the attenuation of the exacerbation, it is allowed to eat vegetable puddings. It is permissible to drink juices and tea with a small amount of sugar. Before lights out, you can drink a little low-fat kefir, fermented baked milk or yogurt.
The diet for the attenuation of exacerbation of pancreatitis is followed for 12 months. Errors in nutrition should not be allowed.
Manifestations
Both of these diseases manifest themselves in pain in the upper abdominal cavity. They become even brighter after a person eats fatty, smoked and spicy foods. But with pancreatitis, the pain becomes girdling. Cholecystitis manifests itself in certain areas of the hypochondrium.
As a rule, the diet for acute cholecystopancreatitis is designed to cope with severe symptoms - bloating, a feeling of heaviness, problems with stool. Often, exacerbations of cholecystitis are accompanied by signs of jaundice. In this case, the skin and mucous membrane become yellowish. Sometimes the stool turns white and the urine darkens.
Pancreatitis is not accompanied by such symptoms.
Treatment
When planning to treat such ailments, you need to consult a doctor. The diet menu for cholecystopancreatitis is compiled individually by a specialist. You need to contact a therapist or gastroenterologist. The diet during an exacerbation of chronic cholecystopancreatitis and during a calm course of the disease will be different.
If there is an exacerbation, it is necessary to eat soft foods. Thus, the diet for exacerbation of cholecystopancreatitis is based on crushed products that are boiled. We are talking about cereals, potatoes, and meat purees. You cannot fry food, smoke it, or preserve it. It is not recommended to add spices, pepper, salt.
To get rid of pain, you need to use antispasmodic medications. At the same time, only a specialist can distinguish between the symptoms of pancreatitis and cholecystitis. The medications in this case will also be different. If cholecystitis is eliminated, you need to choose drugs that provoke the production of bile. Choleretic agents are also needed. Therapy is determined by the characteristics of the disease.
Compliance with diet
Any error in the diet when treating cholecystopancreatitis with a diet can lead to unpleasant consequences. Exacerbations of several interrelated ailments may begin at once. At the same time, diet is the most important part of therapy.
A diet is used for cholecystopancreatitis during the period of exacerbation, as well as for the chronic course of the disease. For people suffering from such diseases, a special diet No. 5 has been developed. It is recommended for those suffering from cholecystitis. Diet No. 5 is also suitable for those who suffer from pancreatitis. The diet and calorie content of these diets are similar.
General principles
When introducing a diet for cholecystopancreatitis during an exacerbation, fasting must be observed during the first days. After this, the menu range is gradually expanded.

It is necessary to introduce a fractional diet. In this case, food is consumed five to six times a day. Thorough chewing of food plays an important role in the diet for cholecystopancreatitis for an elderly person. It is best to eat food at the same time each day. It is important that the dishes are not excessively cold or hot - their temperature should reach 37-40 degrees.
When following a diet for cholecystopancreatitis by an elderly person, as well as at any other age, preference should be given to steaming or baking in the oven. You can also cook food. Fried and spicy foods, marinades, pickles and spicy foods should be limited, as they provoke the secretion of pancreatic juices and bile.
For the same reason, you should avoid products that take a long time to digest. The ban applies to products that lead to increased gas formation and constipation.
The diet for cholecystopancreatitis always includes a lot of protein foods. For the most part it must be of animal origin. It is worth limiting your intake of fats and carbohydrates.
What can you eat
On a diet for cholecystopancreatitis, consumption of lean meat products is allowed. White dried bread is suitable for it. It is recommended to choose one with grains and bran, and it is better if it is yesterday's. The diet for cholecystopancreatitis includes non-acidic dairy products, which have a reduced fat content. We are talking about mild cheeses, dry cottage cheese, and yogurt. Milk should not have a fat content of more than 3.5%.
The diet for cholecystopancreatitis is often based on vegetarian soups without frying. Milk soup is also worth consuming. Soup with meat broth is allowed once or twice a week.
Meat products should not be fatty - you should choose rabbit, turkey, beef and skinless chicken. Seafood, ham, and boiled sausage are suitable. Be sure to include vegetable oil in your diet, but you should not add more than one or two spoons per day to your food. It is worth eating cereals and small pasta. The consumption of millet cereals and pearl barley is rarely allowed. Vegetables and greens are eaten after thermally treating them.
The menu includes non-acidic fruits and berries. It is best to pre-heat them. Dried fruits are also useful for patients with cholecystopancreatitis.
As a rule, doctors advise eating one egg per day in the form of an omelet.
Marshmallows, marshmallows, caramel products and honey are recommended in small dosages. Rosehip infusions and herbal infusions will be useful. If the patient drinks tea, it should not be strong. It is best to mix coffee and tea with milk, and compote, jelly, juice with water.
Diet for chronic pancreatitis
It is called “table 5p”, and is characterized as “gentle, with a reduced amount of carbohydrates (mainly sugar) and extremely low fat content”:
- daily calorie content is 2,600 – 2,800 kcal;
- proteins about 120 g/day (no more than 60% animal proteins);
- vegetable fats – about 15 g/day, animal fats – 65 g/day;
- carbohydrates – no more than 400 g;
- sugar – only 1 tablespoon/day;
- instead of sucrose - 20-30 g of sorbitol or xylitol per day;
- salt – no more than 10 g;
- liquids - 2.5 liters, without gas;
- white bread (yesterday's) - no more than 250 g/day.
Principles of the 5p table
To improve digestion in diseased organs, you need to follow the following nutritional principles:
- meals – 5-6 times a day, in small portions;
- the temperature of food taken is about 40 degrees;
- the total weight of food per day should not exceed 3 kg;
- the basis of the diet is protein foods;
- fried, salted and pickled foods should be excluded;
- vegetables should be boiled or steamed;
- soups - either vegetable or meat broth;
- drink drinks based on chicory flowers;
- Eat chicken eggs (or better yet, only whites) 2-3 times a week in the form of omelettes and boiled eggs.
Advice! The diet should contain a sufficient amount of fiber foods. In addition, you need to consume at least 1 glass of kefir and several pears daily.
What you can and cannot eat

Dishes for pancreatitis and cholecystitis should not be fried
Which foods are allowed for pancreatitis and cholecystitis and which are not, see the table:
| Can | It is forbidden |
| Rusks and yesterday's white bread | Alcohol |
| Vegetarian soups | Rye bread |
| Beetroot | Puff pastry |
| Zucchini | Fresh bread |
| Boiled lean meat and fish (you need to cook without skin) | Baking |
| Steamed egg white omelettes | Broths: meat, fish |
| Porridge: buckwheat, semolina, rice, oatmeal | Borsch |
| Carrot | By-products |
| Potato | Okroshka |
| Green pea | Milk soups |
| Pumpkin for cholecystitis and pancreatitis | Smoked products |
| Boiled vermicelli | Full fat dairy products |
| Ripe, non-acidic fruits that need to be ground | Porridge: millet, wheat, corn |
| Baked apples | Legumes |
| Sugar-free juices from non-acidic fruits and berries | Fried foods |
| Compotes | Cabbage |
| Jelly with xylitol or sorbitol | Radish |
| Low-fat fermented milk products | Radish |
| Vegetable oil – refined, up to 15 g/day | Onion and garlic |
| Tea with milk and lemon | Eggplant |
| Rose hip decoction | Sorrel |
| Butter – only for prepared foods (per day – no more than 30 g) | Spinach |
| Savory pies with cottage cheese | Bell pepper |
| Oatmeal jelly | Animal fats |
| Greenery | Spices |
| Sometimes - high-quality boiled sausage without fat | Raw fruits |
| Sauerkraut, if it is not sour | Figs |
| Dates | |
| Grape | |
| Snacks | |
| Mushrooms and mushroom broths | |
| Salo | |
| Mustard, horseradish | |
| Ice cream | |
| Products with pastry cream | |
| Coffee, cocoa |
Let's look at some individual “controversial” products:
- Bananas for pancreatitis and cholecystitis are allowed, but in small quantities (no more than 1 piece per day), as they contain. It is advisable to use them to add additional flavor to low-fat yogurt, casserole, pie based on low-fat yogurt and dry cookies. You can also drink banana juice, but also in small quantities.
- Sources of essential omega-3 fatty acids, nuts, are allowed for cholecystitis and pancreatitis if the disease is in the chronic stage. This product is good for snacking. It stops inflammation of pancreatic tissue, protects tissue from destruction. But nuts are a fatty food, so you should eat no more than 15 grams of them (any) and only if you are not allergic to them.
- Honey for pancreatitis and cholecystitis is allowed only if the inflammation has not affected the endocrine apparatus of the pancreas and diabetes has not developed. In this case, the product is useful - it helps to “expel” bile that has stagnated in the gallbladder.
Advice! For these diseases, you need to consume honey not whenever you want, but in the morning, on an empty stomach, dissolving a tablespoon of the product in 100 ml of water.
- Persimmon is not recommended for consumption for cholecystitis and pancreatitis. If you really want to eat it, then this can only be done outside of an exacerbation, and only if there is no diabetes.
You can get additional information about nutrition for the pathologies under consideration from the article: 100 approved foods for pancreatitis.
What not to eat
You cannot add fresh bread, pastries, or confectionery to your diet. Strong meat or fish broths, mushroom soup, sour cabbage soup, and okroshka will have a negative impact on your health. Meat and poultry of fatty varieties - goose or duck - are not recommended. By-products can significantly worsen the patient’s condition, as can lard and animal fat.
You cannot eat caviar, fatty fish, or canned food.
Anything spicy, smoked, or pickled is strictly prohibited, as are fast food and other snacks. Fresh vegetables with coarse fibers (radish, white cabbage) can provoke an exacerbation of the disease.
Sour berries and fruits and all foods with a high sugar content have a negative effect on the patient's condition. Preservatives and chocolate can lead to problems. Alcoholic beverages are strictly prohibited on a diet for cholecystopancreatitis.

It is important to remember that all these requirements must be strictly followed. Thanks to this, exacerbations of pancreatitis and cholecystitis will be avoided.
What you can and cannot eat for cholecystitis and pancreatitis: food tables
Recommended nutrition for pancreatitis and cholecystitis can be compiled based on the tables of ingredients.
It is allowed to include in the diet only components that do not increase the load on the digestive organs.
| Allowed ingredients and dishes | In what form are they recommended? |
| Bread | Bran, dried white, grain |
| Cookies, biscuit | Without layers of cream and jam |
| Pies | Exclusively baked, filled with cottage cheese, fish, minced meat |
| Dairy | Milk up to 3.5% and mild cheeses are allowed on the menu. Sometimes use a little sour cream or butter |
| Vegetable/milk soups | 1–2 times a week, without frying individual components |
| Meat | Turkey and rabbit, beef, chicken breast. The skin of the bird is first removed. Sausages, ham, boiled homemade sausages made from these types of meat are allowed |
| Fish, seafood | Steamed, boiled, baked, low-fat |
| Vegetable oils | 1-2 tbsp per day. l. For cholecystitis, refined ones are better |
| Cereals | Semolina, oats, rice, buckwheat are recommended. Barley, barley, corn, millet are occasionally allowed |
| Vegetables, greens | Heat treated |
| Fruits and berries, dried fruits | Sweet varieties. Heat treatment required |
| Eggs | Protein is used for steam omelette. No more than 1 piece. in a day |
| Dessert | Meringues, lozenges, caramel, natural honey, jam made from sweet berries and fruits. It is advisable not to get carried away with sweets, eat a little |
| Beverages | Decoctions of chamomile inflorescences, mint leaves, rose hips, weak tea, weak coffee with milk. Jelly and compotes are prepared from sweet berries. But it is advisable to dilute them with drinking water. Low-fat fermented milk – kefir, liquid yogurt |
In case of cholecystitis and a diseased pancreas, it is necessary to exclude components that provoke increased secretion of enzymes, are poorly digestible, are rich in fiber, and are excessively fatty.
| Prohibited | In what form is it prohibited? |
| Bread | Freshly baked, baked goods |
| Meat | Duck, pork, lamb, goose |
| Fish | Fish broth, caviar, fatty varieties |
| Soups | Sour cabbage soup, okroshka, meat broths |
| Mushrooms | In any form, including mushroom broths |
| Canned food | All pates and marinades, as well as pickles, smoked meats |
| Spices | Horseradish, spicy seasonings, mustard |
| Vegetables | Fresh. In particular, radish and white cabbage, all legumes, sorrel, turnips, radishes and rhubarb, garlic, rutabaga, onions, green peas |
| Fruits and berries | Sour, fresh |
| Fast food | Chips, saltine crackers, ready-made snacks |
| Confectionery | Flavored with creams containing food coloring and flavorings. It is undesirable to consume ice cream and chocolates, sweets |
| Beverages | Alcohol, sweet and mineral soda, strong tea or coffee |
There are “controversial” ingredients:
- You can eat bananas for pancreatitis, but not more than 1 per day. It is better to use as an additional ingredient for pie, dry cookies, casseroles.
- Nuts are allowed to be consumed if the disease is chronic; do not use if there is a risk of exacerbation of cholecystitis and accompanying pancreatitis. Up to 15 g of nuts are allowed daily.
- Natural honey is eaten little by little to eliminate bile stagnation in the absence of pancreatitis/diabetes mellitus.
- The sweet persimmon fruit is useful for cholecystitis, but it is rarely eaten - it causes an exacerbation of pancreatitis, and is completely prohibited for diabetes.
General principles of diet
When the diet becomes more varied, and this happens on the 6-10th day, it is necessary to act gradually. The calorie content of the diet is increased gradually, as is the volume of dishes. It is important to gradually move from enteral nutrition to therapeutic nutrition (the first replaces one meal). Enteral formula remains in the diet for a long time. As a result, the load on the pancreas does not immediately increase.
As a rule, after two to three weeks the patient is transferred to a gentle diet. It must be adhered to throughout the entire time the disease enters the remission stage - this is about three to eight weeks.
Diet therapy tactics
In the case when the patient does not need parenteral and enteral nutrition, and this is determined only by the doctor, nutrition is carried out in accordance with the principle of “hunger, cold and rest.” For one to three days, depending on the person’s condition, the patient fasts. Nutrition is sharply limited to ensure complete rest for an organ in a pathological state.
Competent drinking regime plays an important role. You need to drink at least 1.5 liters of water per day. Recommended 200 ml 6 times a day. Mineral water without gas will be useful. It is better to include rosehip decoction and weak tea in the diet for cholecystopancreatitis. Starting from the third day of illness, a gentle diet is introduced for those whose disease is in the acute stage. After this, elements of a high-protein diet are included.











