Classification of acute paraproctitis
The following types of paraproctitis are distinguished:
- by etiology: specific, post-traumatic and banal;
- by the nature of inflammation: chronic, acute and infiltrative;
- by localization of leaks and ulcers: submucosal, subcutaneous, ischiorectal, retrorectal, pelviorectal;
- according to the location of the fistula in the intestine: posterior, lateral and anterior;
- by localization of the pathological process: deep and superficial;
- in relation to the fistula tract and the sphincter: transsphincteric, intrasphincteric, extrasphincteric.
Risk factors for the development of paraproctitis
The main reasons for the appearance and development of paraproctitis are:
- decreased immunity;
- various chronic diseases;
- exhaustion;
- digestive tract infections;
- stool disorders, as well as proctological diseases such as papillitis, cryptitis, hemorrhoids, anal fissure, proctitis.
However, the leading place in the etiology of the disease is still given to the penetration of infection into the perirectal tissue. The main routes of penetration of such an infection are: anal glands, intestinal mucosa, neighboring organs affected by inflammation, lymphogenous and hematogenous routes.
Some researchers also believe that paraprotctitis is one of the complications of Crohn's disease and ulcerative colitis. In addition, the spread of purulent inflammation throughout the rectum is observed in diseases such as spinal tuberculosis, osteomyelitis of the pelvic bones, diseases of the urethra and prostate gland.
Symptoms of acute paraproctitis
The disease often begins very acutely. Immediately after a short period of malaise, headache and weakness, patients begin to feel increasing pain in the rectum, pelvis and perineum, which is accompanied by chills and fever. The patient’s health status and the complexity of the manifestation of symptoms of the disease depend mainly on the location of the pathology, its nature and prevalence. For example, if the abscess is localized in the subcutaneous tissue, then the symptoms of the disease appear quite acutely, which forces the patient to seek help from a doctor.
The most severe symptoms of paraproctitis manifest themselves in the pelviorectal form of the disease, when the abscess is localized in the pelvis. At first, general symptoms such as chills, pain in the pelvis and joints, and headache predominate. The period of manifestation of such symptoms can vary between 10-12 days. After this time, more pronounced symptoms appear: stool retention, severe pain in the rectum and pelvis, severe intoxication. In some cases, patients experience a breakthrough of pus into the rectum.
Purulent paraproctitis: causes, symptoms, treatment
Since acute purulent paraproctitis is inflammatory in nature, the cause of the disease is pathogenic microorganisms:
- staphylococcus;
- coli;
- streptococcus;
- anaerobic microorganisms.
Fiber damage occurs through inflammation of the rectum and various injuries to the anus. It is also possible for pathogenic microorganisms to penetrate through the bloodstream from other foci of infection (inflamed tonsils, purulent wounds, boils).
In addition to infection, the following factors contribute to the development of the disease:
- hemorrhoids and cones, anal fissures;
- impaired bowel movement;
- diseases of the vascular network (atherosclerosis);
- diseases of the endocrine system;
- general exhaustion of the body that occurs with frequent infectious processes, adherence to diets, alcoholism or drug addiction.
How to recognize purulent paraproctitis
The symptoms of this pathology directly depend on the severity of the disease and the location of the lesion:
- Purulent paraproctitis is characterized by a wave-like course, where the periods of formation of a new focus and recovery are clearly defined.
- Lack of treatment leads to the formation of a fistula. Through its course, there is a constant release of feces mixed with blood and pus.
In addition to general symptoms, the focus of inflammation is accompanied by general signs of intoxication:
- loss of appetite, development of weakness and drowsiness, impaired performance;
- hyperthermia (with the formation of an abscess, the temperature may rise above 38 degrees, and with an uncomplicated process, it does not exceed 38 degrees);
- hyperemia in superficial forms;
- pain in the area of the abscess (the closer the source of the process is located to the surface, the more pronounced they are).
Diagnostics
Only a specialist can make a diagnosis of “acute paraproctitis”. At the first suspicion of an illness in the rectal area, you need to go to the nearest inpatient department, or perhaps a surgical one.
Based on the examination (digital examination of the rectum), a diagnosis is made, and to clarify the localization, depth, extent and location of the abscess, X-rays with a contrast agent and ultrasound diagnostics are used.
In addition to the nature of the abscess itself, the presence of fistulas and other foci of inflammation is established. In case of severe pain, the examination is carried out using local anesthesia. After all the examinations, the specialist determines the method of opening the abscess, as well as further treatment of paraproctitis.
Treatment of purulent paraproctitis
Treatment of this pathology is not limited to drug therapy; urgent surgical intervention is required to get rid of the purulent focus. If this does not happen, the abscess may rupture and spread to surrounding tissues, including the rectum, vagina and prostate gland.
For acute paraproctitis, several types of surgical intervention are used:
1) One-step. Surgically, the abscess is opened, pus, glands and the inflamed anal crypt are removed.
2) Multi-moment. At the first stage, the opening of the abscess and drainage of the abscess, the second stage includes the removal of the glands and affected anal sinuses, as well as the fistulous tract.
The choice of surgical intervention depends on several factors: the accuracy of the diagnosis, the general condition of the patient and the involvement of surrounding tissues in the process.
A one-step technique is possible only if the size of the abscess, the location of the abscess, the anal crypt are known exactly, and if the surrounding tissues are intact (no inflammatory process).
In all other cases, a two-stage operation is recommended. Its second stage occurs approximately a week after the first.
For the treatment of paraproctitis in chronic form, there are other methods, which most often involve opening the abscess, draining the abscess and excision of the fistula.
Postoperative treatment
Treatment of purulent paraproctitis requires careful attention to health and patience. The operation does not always guarantee a complete recovery, however, if it is successful, the process does not relapse. During the rehabilitation period it is recommended:
- take antibacterial drugs, monitor the condition of the rectal area;
- follow a diet that ensures stable bowel function and the complete absence of constipation;
- after each bowel movement and sleep, perform a thorough toilet, use baths prescribed by your doctor;
- during the recovery period, perform exercises that improve blood circulation in the pelvic organs.
If a complication or repeated inflammation occurs, specialists prescribe an examination and perform a second operation to remove the abscess and cleanse the cavity. In case of repetitions of the pathological process, the patient is prescribed immunomodulatory therapy.
Conservative methods
At an early stage of the disease and a mild focus of inflammation, conservative treatment is often prescribed. It includes taking various antibacterial and anti-inflammatory drugs, baths with analgesic and anti-inflammatory effects, as well as physiotherapy procedures.
However, even timely treatment does not guarantee complete recovery. If conservative methods are not effective, the specialist will prescribe surgery, which includes opening and cleansing the purulent formation after the formation of an abscess. Often, infection of the tissue leads to the formation of an abscess (paraproctitis), and in the absence of adequate treatment, a fistula is formed.
Important! Self-medication of purulent paraproctitis in any form is not acceptable. Conservative therapy is possible in a hospital setting and should be carried out under the supervision of a specialist.
Traditional methods
Effective folk methods for treating purulent paraproctitis are recommended to be used in the preparatory period before surgical intervention for chronic paraproctitis. This technique is prescribed by a specialist to reduce inflammation of the affected area.
- Calendula decoction or tincture. The tincture is taken 30 drops several times a day. The decoction is used for oral administration and sitz baths: 1 tsp. Infuse herbs with a glass of boiling water. Take three times a day;
- Baths with mumiyo. Shilajit has an antibacterial and anti-inflammatory effect. Dissolve five tablets in 5 liters of water.
- Baths with salt. For baths, sea salt is used, for this you need 2 tbsp. Dissolve spoons in 5 liters of water.
Important! In case of inflammatory reactions, the use of high-temperature baths is not permissible, since heating the purulent fluid promotes its breakthrough and spread, which is one of the reasons for the formation of a fistula.
Possible complications of paraproctitis
The lack of comprehensive treatment for purulent paraproctitis can cause serious harm to health, especially when the pathology develops against the background of disorders of the immune system.
Failure to surgically open the lesion can lead to the formation of a fistula (if spontaneous opening is performed) or an even more serious complication - phlegmon.
The most dangerous to health are deep-lying foci of inflammation, which can be complicated by peritonitis and pose a high danger to the patient’s life.
A fistula that occurs after purulent paraproctitis is prone to a recurrent process, since constant contamination with feces and infection of the fistula cavity leads to inflammation, which is complicated by the formation of scars. In special cases, severe deformation of the involved tissues occurs - this leads to fecal incontinence.
Against the background of concomitant diseases of internal organs or pathology of the endocrine system, sepsis (blood poisoning) is possible, which is characterized by lightning-fast development with a severe outcome.
Important! Paraproctitis is a serious pathology that requires surgical intervention. If symptoms occur, you should contact a proctologist surgeon or the emergency room of the nearest hospital.
Conclusion
The prognosis of the disease depends entirely on the location of the abscess and the stage of the disease. With early and competent treatment of uncomplicated purulent paraproctitis, the disease ends in complete recovery. Complicated, advanced and chronic forms of this pathology tend to recur.
The severe course of the disease requires enormous effort and patience. Often such treatment can be quite lengthy and last several years. It can end in complete recovery or the formation of complications that can disrupt the patient’s quality of life.
You can share the article with your friends on a social network:
Source: https://proktoinfo.ru/proktit-i-paraproktit/gnojnyj-paraproktit-prichiny-simptomy-lechenie
Symptoms of chronic paraproctitis
Since chronic paraproctitis is a consequence of an untreated acute form of the disease, its symptoms are the same, but are less severe. Chronic paraproctitis is characterized by the occurrence of fistulas, which are manifested by copious discharge into the perineum. Moreover, such discharge causes discomfort and itching. Often there is no pain syndrome. However, pain may occur during bowel movements and then gradually fade away. Symptoms of chronic paraproctitis appear unsystematically, constantly disappearing, then returning again with exacerbation.
Diagnosis of acute paraproctitis
To make a diagnosis, the doctor will only need the data obtained during the interview, as well as a physical examination. The most characteristic clinical signs of the disease, which help to establish the diagnosis as accurately as possible, include the following: purulent inflammation, local soreness, fever. A blood test is prescribed, which, if the disease is present, will show signs of purulent inflammation: increased ESR and leukocytosis with neutrophilia. It is worth noting that some diagnostic techniques are contraindicated due to their pain. These methods include digital examination of the anus, as well as sigmoidoscopy and anoscopy.
Differential diagnosis of acute paraproctitis
For the most accurate diagnosis, additional diagnostic methods are used. Differential diagnosis of paraproctitis is used to distinguish it from other pathologies. First, you need to exclude similar diseases such as a rectal tumor, suppurating teratoma of the peri-rectal tissue, or an abscess of the pouch of Douglas.
Often acute paraproctitis occurs as a complication of a disintegrating tumor. This process can be recognized by digital examination of the rectum. During differential diagnosis, it is also worth excluding malignant processes. This can be done using research methods such as biopsy, ultrasonography, proctography, radiography of the coccyx and sacrum.
Complications of acute paraproctitis
The most severe complications of acute paraproctitis include: inflammation of the cellular space of the pelvis, purulent melting of the walls of the rectum and the entry of pus into the pararectal area, which causes the spread of infection. It is possible that pus may enter the urethra and abdominal area. Complications usually occur if the patient consults a doctor too late. For example, if a patient with a banal form of paraproctitis does not respond to its symptoms for a long time, the disease may worsen until the putrefactive process spreads. No less severe complications of acute paraproctitis are the breakthrough of pus from the affected area through the skin of the perineum or the breakthrough of an abscess into the vagina and lumen of the rectum.
How and how to treat paraproctitis - subcutaneous, chronic and purulent without surgery
Paraproctitis is a tumor - a purulent abscess, which, due to various factors, occurs in the area of pararectal tissue or other tissues located around the rectum (look at the photo: a - subcutaneous, b - ischiorectal, c - pelviorectal, d - submucosal).
The disease can occur in acute and chronic form. Acute paraproctitis is a disease that is diagnosed by a doctor for the first time. Chronic paraproctitis is a relapse of acute paraproctitis.
In the acute form of the disease, the patient may feel relief at the moment of opening the purulent abscess - in this case, unpleasant discharge (pus, ichor) will be observed from the anus. However, this entails a complication - the appearance of a hole (fistula), which requires surgical intervention.
Knowing the causes and conditions for the appearance of paraproctitis will help you avoid treatment and receive timely help. The main factor causing purulent paraproctitis is infection.
Pathogens that contribute to infectious infection of anal tissues are anaerobic flora, Escherichia coli, etc.
Basically, tissue infection occurs due to constipation and hemorrhoids, accompanied by the appearance of cracks in the walls of the rectum or wounds. Through them, the infection enters the body.
The source of infection can be the mucous membrane of the anal gland, which has crypts - depressions that become inflamed due to exposure to pathogens. Later, the infection spreads to the gland itself and to the subcutaneous tissue. Paraproctitis can also result from post-operative or accidental injuries to the anus, proctitis, and diabetes.
For more information about paraproctitis, the causes of its occurrence and operational measures to treat the disease, watch the video:
Paraproctitis. How to behave when you have an “uncomfortable” illness
Causes of the disease
The causative agents of the disease are either transformed from opportunistic intestinal flora or enter from other sources. Acute paraproctitis is classified according to the type of infection:
- Common - caused by streptococci and staphylococci, gram-negative and positive rods, often combined flora.
- Anaerobic - caused by putrefactive bacteria that produce endotoxins (clostridia, fusobacteria, peptococci, peptostreptococci, actinomycetes). The process occurs in a particularly severe form of gas phlegm, putrefactive paraproctitis, and sepsis.
- Specific - the main causes of occurrence: mycobacterium tuberculosis (tuberculous paraproctitis develops slowly), syphilis, actinomycosis.
Important! Traumatic damage to the rectal mucosa, hemorrhoidal node, cracks caused by a foreign body, coarse fecal stone, open the “gate” to any infection.
In primary paraproctitis, pathogenic microbes enter the perirectal tissue from the following:
- the gland surrounding the sphincter due to blockage of the ducts and the formation of abscesses;
- deep cracks penetrating the intestinal wall;
- ulcers due to colitis or Crohn's disease;
- inflamed hemorrhoidal structures.
Symptoms and signs
Purulent paraproctitis appears suddenly and requires immediate treatment. If you notice pathological symptoms, consult a proctologist who will help you cope with the disease. Signs of paraproctitis:
- Intoxication – high temperature, general weakness, headache, loss of appetite, muscle aches.
- The stool becomes hard, causing constipation. The patient experiences numerous unsuccessful urges to defecate and pain during it.
- The urination process is accompanied by pain.
- The patient experiences acute painful sensations in the lower abdomen, near the anus, in the pelvis.
The localization of inflammation affects the symptoms of paraproctitis. For example, subcutaneous paraproctitis is characterized by redness, pain when sitting, swelling, and hardening in the anal area.
- How to relieve inflammation of hemorrhoids quickly
- Proctitis - symptoms and treatment with folk remedies
- How to cure hemorrhoids quickly and permanently at home - drug therapy, diet and exercises
Other types are more difficult to diagnose, since the process occurs deeper, in the subcutaneous tissues.
Due to general signs of intoxication, the patient perceives his condition as flu-like and begins to treat himself, which leads to worsening of the condition and complications.
If general symptoms appear, it is important to consult a doctor who will make a diagnosis, prescribe treatment, and perform the necessary surgical intervention.
What symptoms indicate the presence of the disease?
The characteristics of the course of the disease depend on the location of the process, the reactivity of the body and the microbial flora that caused the inflammation.
The disease begins acutely, after a previous period of general malaise, which lasts about 3 days. During this period, weakness and headache are observed. Then there is an increase in temperature, pain in the perineum and pelvis, the intensity of which increases over time. At this point, the period of general phenomena ends, and the disease acquires obvious signs, depending on the location of the process.
Purulent Paraproctitis
The dynamics of the development of the inflammatory process correspond to the formation of an abscess, which lasts from 2 to 10 days. Symptoms of Paraproctitis: pain in the perineum, which intensifies and becomes pulsating.
If there is no treatment for the resulting abscess, it will spontaneously open into the rectal cavity or onto the skin of the perineum, after which the patient will feel better.
But as a result of this way of solving the problem, a relapse may occur in the future.
Complications of chronic paraproctitis
If chronic paraproctitis is not treated for a long time, the patient's health will gradually deteriorate. In particular, the chronic course of the disease can lead to the formation of scarring, as well as deformation of the rectum and anal canal. In turn, deformation of the sphincter causes leakage of intestinal contents, tonic insufficiency of the sphincters, and partial closure of the anal passage.
Another serious complication of chronic paraproctitis is the appearance of scars on the walls of the anal passage, as well as a decrease in their elasticity. Often, after opening the abscess surgically without removing the abscess tract, rectal fistulas begin to form. In some cases, a fistula does not form, but the focus of inflammation remains, which becomes the cause of relapse of the pathology.
Causes of the disease
Considering that acute paraproctitis is inflammatory in nature and is characterized by the formation of an abscess, the cause of the disease will be pathogenic microorganisms:
- coli;
- staphylococcus;
- streptococcus;
- anaerobic microorganisms.
Bacterial damage to fiber occurs through various injuries and inflammations of the rectum and anus.
It is possible for pathogenic microbes to penetrate into the bloodstream from distant foci of infection (boils, inflamed tonsils, purulent wounds).
In addition to infection, the following factors contribute to the development of acute purulent paraproctitis:
- impaired bowel movement;
- anal fissures, hemorrhoids and lumps;
- diseases of the endocrine system (DM);
- diseases of the vascular network (atherosclerosis);
- general exhaustion of the body with frequent infectious processes, alcoholism, drug addiction or adherence to diets (especially hunger strikes).
Important. Paraproctitis is always a secondary process that occurs against the background of some disease. Treatment isolated from the root cause of the disease is not effective; recovery will only be temporary. First of all, the cause must be identified and the original disease eliminated.
Treatment of paraproctitis
Treatment of acute paraproctitis using exclusively conservative methods is ineffective, so surgical techniques are used. In this case, the operation should be performed immediately after diagnosis, since it is classified as emergency. The type of anesthesia is important; effective pain relief is necessary, as well as complete relaxation. The following types of anesthesia are often used: intravenous anesthesia, sacral and epidural anesthesia. It is worth noting that local anesthesia for this diagnosis is considered inappropriate due to the risk of spreading infection and insufficient pain relief. The main tasks performed during surgery include: opening the abscess, draining it, searching for inflamed crypts and purulent tracts, as well as their elimination.
If the operation is performed in a non-specialized clinic, only opening and drainage is performed. More complex and radical operations are performed exclusively in coloproctology departments. It is strictly not recommended to perform complex operations without the necessary knowledge and skills, as this can lead to the removal of part of the external sphincter along with the purulent tract, resulting in its insufficiency. On our website you will find clinics that specialize in performing this type of surgery. The most radical operations that are used to treat acute paraproctitis include opening, draining the abscess, and also:
- excision of the inflamed crypt and dissection of the purulent passage;
- excision of the inflamed crypt and sphincterotomy;
- holding a ligature;
- moving a section of the intestinal mucosa in order to stop infection that spreads from the lumen of the rectum.
Acute paraproctitis is a serious disease, so its treatment is considered a rather difficult task and requires a lot of time and experience.
The most favorable prognosis for the patient is when treating subcutaneous inflammation, as well as the superficial location of the purulent tract. In this case, an operation is used to dissect the purulent tract into the intestinal lumen and remove the inflamed crypt. However, if the purulent tract is located high enough, which often happens with pelviorectal and ischiorectal forms of the disease, the choice of surgical technique turns out to be quite difficult.
It is worth noting that in some cases surgical intervention becomes impossible. In particular, it is not recommended to prescribe surgery if the patient’s body is weakened, a serious organ disease is detected, or he is of old age. In all these cases, it is advisable to first treat the pathology using conservative methods, improve the patient’s health, and then perform surgery. Sometimes, after paraproctitis, the patient’s fistula tracts close together, which makes the operation impossible. Therefore, surgical intervention is postponed until the fistula becomes open.
Treatment
Acute paraproctitis can only be treated surgically. Conservative methods only work in cases where paraproctitis is diagnosed at the infiltrate stage. This is possible with subcutaneous localization of paraproctitis. In this case, opening it does not give results. Broad-spectrum antibiotics are prescribed internally. The treatment strategy is watchful.
When pus appears, acute paraproctitis must be opened. The operation must be performed in a specialized department. Only in this case is it possible to carry it out in one stage. After all, the purpose of this intervention is not only to open the abscess and remove the pus. It is important to find the path of infection and eliminate it. Only then can you count on a complete recovery.
The operations are performed under anesthesia. Sometimes conduction anesthesia is used. The extent of the operation depends on the location of the abscess. When the abscess is deep and a fistula tract is formed, surgical treatment can be very difficult. It requires a lot of experience from the doctor.
The important task of the surgeon excising paraproctitis is not to damage the external sphincter of the anus. Injury to it can lead to fecal incontinence.
In the postoperative period, the patient is prescribed antibacterial drugs and dressings are performed. In the long term, physiotherapy procedures are prescribed to accelerate wound healing.
Prognosis for paraproctitis
A favorable prognosis in the treatment of acute paraproctitis is quite possible. However, this will require timely diagnosis and treatment. Therefore, it is extremely important that the patient consult a doctor immediately after identifying the first symptoms of the disease. Otherwise, if the disease is not treated for a long time, serious complications for the patient’s health may occur. In particular, ignoring the symptoms of pathology can lead to the formation of fistulas and the progression of the disease to an acute form.
After surgery, during which the fistulas were excised, the patient recovered completely. However, it is worth noting that excision of fistulas located quite high can be problematic. In some cases, fistula tracts cause the spread of purulent inflammation into hard-to-reach areas of the pelvis, which ultimately causes partial removal of the infection and, as a consequence, relapse of the disease. If during the operation the abscess was only opened without removing its connection with the intestinal lumen, complete recovery is unlikely. This is due to the fact that the patient develops a rectal fistula, after which after some time the disease relapses.
What you need to know about purulent paraproctitis
Purulent paraproctitis is a purulent-inflammatory disease of the tissues (fatty tissue) surrounding the rectum. Paraproctitis accounts for 15% to 30% of all diseases of this part of the intestine.
In terms of frequency of occurrence, this disease ranks fourth after hemorrhoids, anal fissures and colitis. Women suffer from paraproctitis less often than men, this is due to the anatomical features of the structure of the cellular spaces around the rectum.
It is worth noting that this pathology almost never occurs in children.
Causes
Paraproctitis is an infectious disease; it is caused by microflora entering the pararectal (surrounding the rectum) tissue. The leading role is played by pathogens such as E. coli and staphylococcus, but in some cases the cause may be viruses, mycoplasma, chlamydia or other microorganisms. Ways for the spread of infection can be:
- Anal glands. Through their mouths, which are located at the bottom of the anus, aggressive microflora can penetrate deeper, thereby causing an inflammatory process.
- Tears of the mucous membrane. Causes of mucosal injury: passage of excessively dense feces through the intestine, childbirth, and entry of foreign objects into the intestinal lumen.
- Morgagni's crypts are folds of the mucous membrane. Almost always one of the crypts is associated with an abscess.
- Hemorrhoids can also be the cause of a purulent process. Bleeding from hemorrhoids is accompanied by a violation of the integrity of their surface, which can lead to infection of the intestinal microflora.
- Other purulent foci in the body. With a general weakness of the body's immunity, a hematogenous route of paraproctitis may occur, when harmful microorganisms enter the peri-intestinal area through the bloodstream.
The development of purulent paraproctitis is predisposed to:
- persistent constipation;
- diabetes;
- atherosclerotic deposits;
- haemorrhoids;
- immunodeficiency.
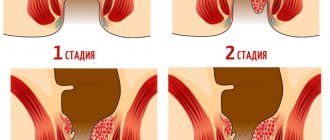
Types and symptoms of purulent paraproctitis
The course of paraproctitis can be in two forms: acute and chronic. Acute paraproctitis is characterized by the fact that it occurs for the first time and proceeds with the formation of abscesses (cavities with pus) in the fatty tissue around the rectum.
This is accompanied by pain during defecation, high fever (up to 39°C and above) and general symptoms of an inflammatory disease (weakness, body aches, headache). The contents of the abscess often break into the rectum or into the pelvic cavity.
The second option is considered less favorable, as it can lead to the spread of the purulent-inflammatory process. Depending on the location of the source of suppuration, acute paraproctitis is divided into:
- Subcutaneous - located, as the name suggests, under the skin, in the fatty tissue around the anus. This type of paraproctitis is visible to the naked eye and looks like a red swelling in the anal area. When you try to sit down or touch, a sharp pain occurs at the site of inflammation, which gradually acquires a constant pulsating character. In addition, fever, headache, and general weakness are observed. Due to pain and swelling, the passage of feces is impaired.
- Acute purulent ischiorectal paraproctitis is localized in the anatomical formation called the ischiorectal fossa, involving the levator anus muscle. It manifests itself as pain in the pelvic area, which intensifies when trying to push, when coughing, sneezing. After a few days, a red swelling appears in the anus and the temperature rises.
- Acute pelviorectal paraproctitis - involves the pelvic-rectal tissue space and is located on the border with the abdominal cavity. The purulent focus is located quite deep and has no specific external manifestations. At the onset of the disease, general symptoms occur: fever, body aches, weakness. Having reached a certain size, the abscess begins to put pressure on the surrounding organs, and problems with physiological functions may arise.
- Retrorectal – located behind the rectum. In the early stages of the disease, with this type of paraproctitis, there are also no local symptoms, only general symptoms. Pain may also be observed along the sciatic nerve.
- Submucosal paraproctitis – located under the mucous membrane of the rectum. As a rule, diagnosis is not difficult. This type is characterized by pain in the rectal area, and digital examination reveals swelling with significant pain. Most often, such an abscess breaks into the lumen of the rectum, pus comes out through a natural opening, and recovery occurs.
Chronic paraproctitis is a consequence of poorly treated acute paraproctitis, which takes a protracted course and is characterized by the formation of fistulas, that is, passages that open outward. Fistulas can be complete and incomplete, external and internal, simple and complex. Based on their location relative to the sphincter, they are distinguished:
- front;
- lateral;
- rear
A frequent manifestation of chronic paraproctitis is the discharge of pus and blood into the perineum, where the fistula usually opens, which causes an itching sensation. As a rule, a fistula that opens onto the surface of the skin does not cause pain, since the contents easily flow out and do not accumulate in the cavity of the abscess.
Painful sensations that arise or intensify during the act of defecation are characteristic of internal fistulas, since in this case there may be obstacles to the free outflow of pus.
Chronic paraproctitis occurs with periods of remissions and exacerbations; this is due to the fact that the lumen of the fistula tract is periodically clogged, and abscesses arise, which usually open on their own, which leads to an improvement in the condition.
https://gemorroi.su/www..com/watch?v=MV8QwZUiYvw
Treatment and prognosis
If it was possible to catch paraproctitis at the initial stage, then conservative (non-surgical) treatment can be used. For this, broad-spectrum antibiotics, potassium permanganate baths, and UHF therapy are used.
If there is an already formed abscess or fistulous tract, then therapy involves surgical intervention.
In case of acute paraproctitis or exacerbation of chronic paraproctitis, the main task of the operation is to open and empty the abscess, followed by washing its cavity with antiseptics.
But sometimes leaving the abscess cavity, even washed out, can lead to relapse, that is, re-occurrence of inflammation.
Therefore, complete excision of damaged tissue is often used, including fistulas that form during the transition from acute to chronic form. Usually the operation is performed under general anesthesia.
Surgical treatment is always combined with antibiotic therapy: this avoids the recurrence of a purulent lesion and the spread of infection.
https://gemorroi.su/www..com/watch?v=ko-qYQ4mcp0
With timely treatment of purulent paraproctitis, the prognosis is favorable: complete recovery occurs.
Source: https://gemorroi.su/gemorroy/lechenie/oslozhneniya/paraproktit/gnojnyj