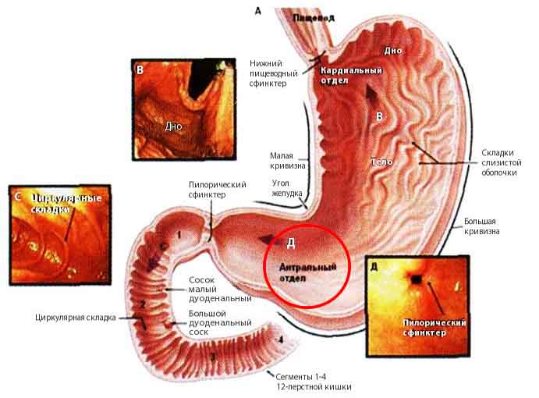
Hyperplastic gastritis is a lesion of the stomach, in which increased proliferation of the mucosal epithelium occurs, thick folds and polyps are formed. The antrum is most often affected. The pathology is of a secondary type, developing against the background of other processes. Antral gastritis with hyperplasia of the lining membranes accounts for about 5% of the total number of gastrointestinal diseases.
The structure of the stomach and the location of the antrum
Causes of the disease
In most cases, hyperplasia appears because the patient has not completed treatment for any disease, such as stomach ulcers, gastritis or other inflammations. This leads to active cell division, which contributes to the formation of polyps. The bacterium Helicobacter pillory can also provoke these changes. Sometimes pathology appears due to various infectious diseases. But these are not the only reasons for the appearance of hyperpasia; there are others:
- disruption of the patient’s hormonal levels, for example, excess estrogen;
- heredity, so if a woman has adenomatous polyposis, her daughter or granddaughter can inherit it; with this disease, polyps also form in the human stomach;
- the patient has been taking certain medications for a long time, which damage the walls of the stomach;
- carcinogens have entered the body, which also contribute to the growth of the gastric epithelium.
Endometrial hyperplasia
Or, more understandably, uterine hyperplasia. In most cases, this is a benign neoplasm, but if the disease is neglected, it degenerates into a malignant tumor.
- In the summer, when you harvest cucumbers, do not throw away the vines, but dry them. They will be useful for treatment. Fifty grams of dry crushed cucumber lashes, poured two glasses of boiling water, boil for five minutes. Cool and drink one hundred ml three times a day.
- Drink fifty milliliters of carrot and beet juice every day.
- Twice a day, eat a tablespoon of flaxseed oil before meals.
Symptoms
If the patient has an early stage of the disease, it will be very difficult to diagnose it based on symptoms, since the person does not experience any discomfort when epithelial tissue grows. Even the appearance of hyperplastic polyps, if they are small, is not felt by the patient; only large polyps can impede the passage of food and cause severe bleeding or provoke pain.
However, as the pathology progresses, the functioning of the stomach is disrupted, which causes digestive problems. This leads to the patient experiencing a number of symptoms that may indicate the appearance of hyperplasia:
- pain, it can be either temporary or constant, makes itself felt after eating or when the patient has been fasting for a long time;
- suffers from heartburn;
- the stomach is bloated, there is constipation;
- belching occurs with a long sour taste;
- in later stages, the patient may complain of nausea and vomiting;
- he loses his appetite;
- The patient complains of weakness, body aches, and suffers from dizziness.
If these and other symptoms appear, you should consult a doctor and undergo a full examination.
Gastric hyperplasia
Occurs when uncontrolled growth of cells in the stomach lining begins. Sometimes it can develop in a patient with a chronic form of gastritis.
- Drink one glass in the morning and evening of St. John's wort decoction. Pour two tablespoons of herbs into a thermos, pour in two glasses of boiling water and leave for two hours. After straining, the decoction is ready for use.
- An excellent remedy is a decoction of parsley roots. Grind the roots, pour a glass of boiling water and leave overnight. Strain and drink one spoon up to five times a day.
- Horseradish increases the production of gastric juice and destroys tumors in the stomach. Grate the horseradish and put it in a jar. Every time before meals, eat a spoonful of horseradish with the addition of a small amount of honey.
- Sea buckthorn oil will help solve stomach problems. Take a spoonful of oil half an hour before each meal.
- Massage will be effective if done regularly. Make it a rule in the morning, before getting out of bed, to massage your belly in the stomach area clockwise. At least sixty “turns of the arrows”.
Types of hyperplasia
There are many types of gastric hyperplasia, each of which manifests itself in its own way.
Focal
Focal hyperplasia of the gastric mucosa is a type of polyp, early stage. Often certain areas of the mucous membrane are affected, “foci” of the disease, with clearly defined boundaries. This lesion can be of different shapes or sizes; it looks like a small outgrowth. These lesions are usually of a different color, so they are clearly visible against the background of intact mucosa. The patient may have only one lesion, or many of them. Focal hyperplasia of the stomach appears where the patient previously had erosion or any other damage.
Lymphoid
Lymphoid hyperplasia of the stomach is an increase in the number of lymphocytes in human lymph nodes. With this pathology, the lymph nodes themselves suffer; this is not just the body’s reaction to inflammation. But an increase in the number of lymphocytes can also be associated with some kind of infection, as a response from the immune system. Lymph nodes play an important role in the body; they help cope with viruses, suppress their reproduction, and fight bacteria.
Follicular
Follicular hyperplasia of the stomach is a fairly common disease. The gastric mucosa contains cells and the lymphatic system. If they begin to divide quickly, this pathology appears.
Lymphofollicular hyperplasia occurs quite often, especially if people eat various carcinogens. The reason for its appearance may be a violation of hormonal processes, the activity of Helicobacter pylori, and regular stress, and so on. With this disease, areas with accumulations of lymphocytes, called follicles, are visible on the mucous membrane.
Integumentary pit epithelium
What is this stomach pathology? It has a name: “hyperplasia of the integumentary pitted epithelium.” This is a dangerous disease that can cause swelling. The columnar epithelium changes under the influence of unfavorable factors: both the number of epithelial cells and their structure. The cells increase in size, mucin accumulates in the cytoplasm, and the nucleus is displaced to the base. The patient develops new spur-shaped gastric pits.
Antrum
The closing, last part of the stomach is called the antrum, it is from here that food passes into the intestines. The antrum is the third part of the stomach, and is one of the most vulnerable parts of the organ, as it most often suffers from various diseases and is subject to all kinds of stress. If a patient has hyperplasia of the antrum of the stomach, then many small growths appear in this place. You can also often see wide branched ridges and elongated pits, which also indicate the presence of pathology.
Foveolar
Foveal hyperplasia of the stomach is a pathology in which the length and curvature of the folds present on the mucous membrane increase. More often, the cause of its appearance is a prolonged inflammatory process or taking anti-inflammatory drugs without a doctor’s prescription.
Oncology of the esophagus: how to recognize cancer, and what is the prognosis with timely treatment
All digestive organs are susceptible to cancer, and the esophagus is no exception. Oncology of the esophagus, the symptoms of which will be discussed in detail in the article, is a rarer phenomenon compared to other organs of the gastrointestinal tract, but this pathology is recognized as one of the most severe.
The appearance and development of a cancer tumor is influenced by both external and internal factors: genetic predisposition, deterioration of health, environmental conditions, foods consumed, age and the presence of concomitant diseases in a person.
According to oncologists, this type of cancer most often affects mature males who have reached the age of 55. At the same time, the fair half of humanity suffers from this disease 5 times less often.
Types of esophageal tumors
Any neoplasms are divided into benign (tumors) and malignant (cancer). They are formed from different layers of the esophageal wall, most often in the middle and lower esophagus. Tumors of the esophagus have their own histological classification.
- Epithelial . This type of tumor is formed from epithelial cells, mucous membranes of internal organs and skin. This type of neoplasm includes both benign tumors - papilloma and adenoma, and malignant ones - such as squamous cell carcinoma, adenocarcinoma (more details), small cell carcinoma and others.
- Non-epithelial . This group of tumors is the most numerous. Neoplasms of this type have a variety of origins: from muscle tissue (esophageal leiomyoma), from adipose tissue (lipoma), from blood vessels (hemangioma), from connective tissue (fibrosarcoma), from cartilage tissue (chondrosarcoma) and so on.
- Mixed . This type of neoplasm affects all layers of the esophageal walls and is characterized by rapid decay and the formation of ulcers at the site of decay. Mixed types of tumors include: carcinosarcoma, malignant lymphoma, carcinoid tumor and others.
How to recognize cancer?
In order to promptly diagnose this difficult disease, it is important to identify the main signs of esophageal cancer:
- Dysphagia is a disorder of the process of swallowing food. Difficulty in passing food through the esophagus into the stomach. The patient may feel imaginary retention of food in the walls of the esophagus, creating a feeling of obstruction in the throat.
- Systematic regurgitation and esophageal vomiting . This symptom appears soon after eating.
- Deterioration of appetite , rapid weight loss and anemia, against the background of general malaise, weakening of the body.
- Painful sensations in the chest area, usually a burning sensation . This symptom indicates tumor growth beyond the esophageal wall. Characteristic of the late period of the disease.
Diseases and conditions characteristic of this oncology
Hemangioma is a fairly rare form of benign neoplasm, which has a soft consistency and very vague boundaries.
Esophageal hemangioma is a nonepithelial vascular tumor that spreads along the wall of the esophagus and adjacent tissues.
Despite the benign nature of the neoplasm, hemangioma can grow to significant sizes and compress blood vessels and organs, thereby disrupting cellular nutrition processes.
Leiomyoma is one of the most common benign tumors. Leiomyoma is a submucosal formation of the esophagus. What it is has become clear, and it grows from its muscular shell. This formation has a round shape and protrudes into the esophageal lumen. Like all submucosal tumors, leimioma has a virtually asymptomatic course for a long time.
Blastoma is a general name for any tumors and neoplasms that have extremely active tissue growth. There are 2 types of blastomas: benign and malignant.
The main difference between these types is that the development of a benign tumor does not invade other tissues and does not spread metastases, unlike a cancerous tumor that grows into neighboring and distant tissues, destroying the walls of blood vessels.
Modern medicine successfully copes with the treatment of non-cancerous formations, however, malignant esophageal blastoma is considered the most complex pathology, due to the implicit initial symptoms.
Esophageal hyperplasia is a precancerous condition in which the tissue of the organ grows and its natural cellular structure is replaced by a pathological one. The main prerequisite for the appearance of esophageal hyperplasia is considered to be its systematic chemical damage, which occurs as a result of the patient having a prolonged gastroesophageal reflux pathology.
In this case, the functioning of the digestive tract is disrupted and gastric acid refluxes into the esophagus, which leads to regular chemical damage to the esophagus.
Dysplasia is a pathologically abnormal development of organs and tissues of the body at the cellular level.
Esophageal dysplasia is characterized by a structural disorder of the esophageal mucosa, in which the normal cells of the esophageal mucosa are replaced by cells of the intestinal mucosa.
This increasing process of degeneration of the cellular structure is an absolute risk factor for the development of esophageal cancer.
There is also a type of this group of diseases known as esophageal metaplasia.
This pathology occurs in 13% of patients with any diseases of the digestive system. Glycogen acanthosis of the esophagus - what is it? Its nature has not been fully studied, but experts are inclined to believe that the pathology progresses due to chronic irritation of the mucous membrane. Irritating factors include: abuse of alcoholic beverages, smoking and spicy foods.
Comprehensive diagnosis and therapy of esophageal oncology
To determine the nature of the neoplasm, the degree of damage to the esophagus and the presence of metastases, basic diagnostic procedures are prescribed:
- Biochemical blood test to identify tumor markers. Cancer cells secrete special substances that make it possible to recognize the presence of cancer. What tumor markers exist for the esophagus and stomach? There is more than one esophageal tumor marker: CYFRA 21-1, TPA, SCC. To identify a malignant tumor of the stomach in medicine, a tumor marker of the stomach is used: CA 72-4.
- X-ray with a contrast agent - barium sulfate. This method reveals the tumor lesion and its location.
- Endoscopic examination to determine the extent of the neoplasm, its nature and degree.
- Computed tomography and magnetic resonance imaging of the abdominal organs to identify the stage of tumor development and detect metastases.
- Biopsy of biological material . It is carried out by collecting pieces of tissue and organs for further study.
There are several treatment methods for patients with esophageal cancer:
- Surgery . Removal of part of the esophagus and nearby lymph nodes and tissue.
- Chemotherapy . Impact on oncology using powerful toxins and poisons.
- Radiation therapy . Kills cancer cells using ionized radiation.
- A combination of the above methods.
An incorrect lifestyle and bad habits can lead to unpleasant phenomena in the body. This can be avoided! Important tips from experienced doctors are presented in this video.
Forecast
If the malignant tumor is not subjected to active therapy, the prognosis for the patient’s survival will be very poor. Without any treatment for such a dangerous pathology, a person will live no more than 9 months.
If it is possible to detect cancer at stages 1 or 2 of development, then surgical excision of the tumor is performed, the patient’s life continues after the operation and nothing threatens it in 85% of cases.
The third and fourth stages of cancer have ambiguous prognoses, due to the spread of metastases throughout the body. In this case, modern medicine is able to slow down the processes of metastasis or stop them indefinitely. The prognosis for stage 3 esophageal cancer is very negative. The overall percentage of survivors after therapy does not exceed 15%.
Source: https://GastrituNet.online/bolezni-pishhevoda/onkologiya/onkologiya-pishhevoda.html
Diagnostics

We figured out what hyperplasia is. It would be quite difficult to make a diagnosis based only on symptoms, so the patient is sent for gastroscopy. An endoscope, which has a light source and cameras, is inserted into the patient's stomach. The doctor can examine the walls of the stomach and note any changes. The doctor also performs a biopsy of the stomach walls. Histology helps to make an accurate diagnosis, exclude oncology, and also helps to identify the type of hyperplasia and the cause of its occurrence.
Diagnosis of gastric hyperplasia
The diagnosis of gastric hyperplasia is a histological diagnosis, that is, to establish it, a biopsy of the mucous membrane with further laboratory testing is necessary. To obtain a tissue sample for histological examination, an endoscopic examination is performed.
Gastroscopy is a procedure during which a thin, flexible instrument (endoscope) with a light source and a camera is inserted into the stomach. With this examination, you can detect problems with the stomach, as well as perform a biopsy of its walls. With hyperplasia, the doctor can see the presence of polyps and thickened mucosa in the stomach, deepening of the folds and their excessive tortuosity. Read more about gastroscopy→
Carrying out a histological examination of tissue obtained through biopsy not only establishes the diagnosis of hyperplasia, but also determines its type and can help determine its causes. It is believed that each gastroscopy should be accompanied by a biopsy of the gastric mucosa.
Another examination method that can help to suspect the presence of hyperplasia is contrast fluoroscopy of the stomach. During the examination, the patient drinks a solution containing a radiopaque substance (barium), after which the radiologist examines the digestive tract. Using this method, you can notice thickening of the gastric mucosa and the presence of large polyps. Contrast fluoroscopy is inferior in its diagnostic value to gastroscopy.
To identify the causes of gastric hyperplasia, tests may be performed to detect the bacteria H. pylori, which often causes these pathological changes in the mucous membrane.
- Detection of antibodies in the blood, the detection of which indicates that the patient’s body has been or remains infected with H. pylori.
- Urea breath test. The patient is given a solution containing urea, the molecules of which contain a labeled carbon atom, to drink. If he has H. pylori in his stomach, the bacteria break down the urea into water and carbon dioxide. Carbon dioxide is absorbed into the bloodstream and eliminated from the human body through the lungs. By taking a sample of exhaled air, you can detect this labeled carbon atom in it using a special scanner.
- Detection of H. pylori antigens in stool.
- Stomach biopsy with further laboratory examination of samples.
To detect possible causes of gastric hyperplasia, many patients also undergo an ultrasound examination of the abdominal organs, which can be used to diagnose various diseases of the pancreas, liver and biliary tract. Sometimes a computed tomography scan is performed to verify the diagnosis.
The choice of treatment method depends on the cause of gastric hyperplasia.
Eradication of H. pylori
If the proliferation of mucosal cells has developed due to a chronic inflammatory process due to H. pylori infection, then eradication (elimination) of these bacteria from the stomach is necessary.
For this, there are effective treatment regimens, including:
- antibiotics (Clarithromycin, Amoxicillin, Metronidazole, Tetracycline, Levofloxacin);
- proton pump inhibitors that suppress acid secretion in the stomach (Pantoprazole, Esomeprazole, Omeprazole);
- bismuth preparations, which have protective properties for the gastric mucosa, and also negatively affect the bacteria H. pylori.
The selection of the correct treatment is carried out by the doctor, based on the clinical picture of Helicobacter pylori infection and data on the resistance of bacteria to antibiotics.
The duration of the course of eradication therapy is from 7 to 14 days.
Treatment of hyperplastic polyps
If the patient has polyps, the choice of treatment method depends on their type:
- Small non-glandular polyps. May not require treatment. They usually do not cause any symptoms of the disease and rarely develop into malignant tumors. Doctors usually recommend that patients undergo periodic gastroscopy to monitor polyps. If they increase in size or begin to bother the patient, they can be removed.
- Large polyps. They may need to be removed. Most polyps can be removed endoscopically.
- Glandular polyps. They can turn into malignant tumors, so they are usually removed using endoscopy.
- Polyps associated with familial adenomatous polyposis. They need to be removed as they turn into cancer. Removal is carried out endoscopically or openly.
Diet and lifestyle changes
Symptoms of hyperplasia can be relieved with the following tips:
- You need to eat in smaller portions, but more often.
- It is necessary to avoid foods that irritate the stomach (spicy, sour, fried or fatty foods).
- Do not drink alcoholic beverages, which can irritate the gastric mucosa.
- It is necessary to stop taking non-steroidal anti-inflammatory drugs and replace them with other drugs.
- Stress, which can worsen symptoms of gastric hyperplasia, should be controlled. You can practice yoga or meditation for this purpose.
Treatment
A gastroenterologist treats gastric hyperplasia; if necessary, he can refer you to an oncologist or a surgeon, but surgical intervention is required in rare cases; conservative treatment is more often prescribed.
Drug treatment
If a patient has gastric hyperplasia, treatment is the fight against the underlying disease that caused this pathology. The doctor may prescribe either antibacterial agents if you need to fight an antibacterial infection, or gastroprotectors that protect the gastric mucosa. If the cause of the disease is increased acidity, then drugs that reduce acidity are prescribed. Hormonal medications can also help in those rare cases when the disease is caused by hormonal imbalances.
Surgery
If there are too many polyps and they have reached a significant size, the doctor may prescribe an endoscopic polypectomy, when they are removed using an endoscope. As a last resort, open surgery is performed on the stomach or part of the organ is removed.
Diet
If a person has gastric hyperplasia, the patient is prescribed dietary nutrition, that is, only foods that are safe for the gastric mucosa and do not cause irritation are allowed. The diet largely depends on the underlying disease that caused the appearance of hyperplasia. However, some nutritional rules are suitable for all patients with this pathology, for example, split meals. The patient should eat at least 5 times a day, in small portions. Among the prohibited foods:
- alcohol;
- soda, coffee, strong tea;
- spicy and fatty, fried foods;
- food too hot.
It is useful to eat foods rich in fiber, such as porridge. You shouldn’t give up meat or fish, but it’s better to choose low-fat varieties; rabbit, chicken and turkey are especially healthy. It is advisable to boil or stew everything; you can steam it. If you want to cure a disease faster, diet should become a part of your life.
ethnoscience
If the attending physician does not mind, you can also use traditional methods. But a contraindication to their use may be the presence of a particular disease. Therefore, before drinking certain infusions or decoctions, study all the contraindications for each herb that is included in this decoction, and only after that begin treatment.
Stomach diseases are well treated by chamomile, which is an excellent antiseptic. It relieves pain and muscle spasms. Ginger root also has antibacterial properties. Peppermint helps relieve heartburn and nausea.
There are other recipes that help cure hyperplasia, for example, an infusion of parsley roots. To prepare it, take 250 ml of boiling water and pour 1 tbsp. chopped roots, leave to infuse overnight. You need to take this medicine in the morning, afternoon and evening, 1 tbsp. A decoction of fireweed tea is useful. You will need 10 g of chopped herb, which is poured with 250 ml of water. The broth should be boiled for at least a quarter of an hour, then left for 1 hour. Then you need to add water to restore the original volume. You need to drink the decoction 3 times a day, 1 tablespoon, before meals.
It would be a mistake to call gastric hyperplasia a separate disease; it is rather a pathological process that accompanies many diseases (most often gastritis). If these and other symptoms appear, it is better to immediately go to the clinic, get examined and begin treatment. Cured stomach diseases are a guarantee that you will not develop hyperplasia. Proper nutrition and a healthy lifestyle also play an important role. In some cases, timely treatment can save lives, for example, prevent the occurrence of stomach cancer.
source
Inactive gastritis with foveal hyperplasia
Gastric hyperplasia is a pathology in which a person has an increase in the number of stomach cells, but these cells can be called normal, that is, this is not oncology. There are more cells than necessary, so the patient’s mucous membrane is much thicker than normal, and polyps may appear on it. Hyperplasia can affect not only the gastric mucosa, but also any organ, but today we will talk specifically about gastric hyperplasia. In most cases, hyperplasia appears because the patient has not completed treatment for any disease, such as stomach ulcers, gastritis or other inflammations. This leads to active cell division, which contributes to the formation of polyps. The bacterium Helicobacter pillory can also provoke these changes. Sometimes pathology appears due to various infectious diseases. But these are not the only reasons for the appearance of hyperpasia; there are others:
- disruption of the patient’s hormonal levels, for example, excess estrogen;
- heredity, so if a woman has adenomatous polyposis, her daughter or granddaughter can inherit it; with this disease, polyps also form in the human stomach;
- the patient has been taking certain medications for a long time, which damage the walls of the stomach;
- carcinogens have entered the body, which also contribute to the growth of the gastric epithelium.
If the patient has an early stage of the disease, it will be very difficult to diagnose it based on symptoms, since the person does not experience any discomfort when epithelial tissue grows. Even the appearance of hyperplastic polyps, if they are small, is not felt by the patient; only large polyps can impede the passage of food and cause severe bleeding or provoke pain.
However, as the pathology progresses, the functioning of the stomach is disrupted, which causes digestive problems. This leads to the patient experiencing a number of symptoms that may indicate the appearance of hyperplasia:
- pain, it can be either temporary or constant, makes itself felt after eating or when the patient has been fasting for a long time;
- suffers from heartburn;
- the stomach is bloated, there is constipation;
- belching occurs with a long sour taste;
- in later stages, the patient may complain of nausea and vomiting;
- he loses his appetite;
- The patient complains of weakness, body aches, and suffers from dizziness.
If these and other symptoms appear, you should consult a doctor and undergo a full examination.
There are many types of gastric hyperplasia, each of which manifests itself in its own way.
Focal hyperplasia of the gastric mucosa is a type of polyp, early stage. Often certain areas of the mucous membrane are affected, “foci” of the disease, with clearly defined boundaries. This lesion can be of different shapes or sizes; it looks like a small outgrowth. These lesions are usually of a different color, so they are clearly visible against the background of intact mucosa. The patient may have only one lesion, or many of them. Focal hyperplasia of the stomach appears where the patient previously had erosion or any other damage.
Lymphoid hyperplasia of the stomach is an increase in the number of lymphocytes in human lymph nodes. With this pathology, the lymph nodes themselves suffer; this is not just the body’s reaction to inflammation. But an increase in the number of lymphocytes can also be associated with some kind of infection, as a response from the immune system. Lymph nodes play an important role in the body; they help cope with viruses, suppress their reproduction, and fight bacteria.
Follicular hyperplasia of the stomach is a fairly common disease. The gastric mucosa contains cells and the lymphatic system. If they begin to divide quickly, this pathology appears.
Lymphofollicular hyperplasia occurs quite often, especially if people eat various carcinogens. The reason for its appearance may be a violation of hormonal processes, the activity of Helicobacter pylori, and regular stress, and so on. With this disease, areas with accumulations of lymphocytes, called follicles, are visible on the mucous membrane.
What is this stomach pathology? It has a name: “hyperplasia of the integumentary pitted epithelium.” This is a dangerous disease that can cause swelling. The columnar epithelium changes under the influence of unfavorable factors: both the number of epithelial cells and their structure. The cells increase in size, mucin accumulates in the cytoplasm, and the nucleus is displaced to the base. The patient develops new spur-shaped gastric pits.
The closing, last part of the stomach is called the antrum, it is from here that food passes into the intestines. The antrum is the third part of the stomach, and is one of the most vulnerable parts of the organ, as it most often suffers from various diseases and is subject to all kinds of stress. If a patient has hyperplasia of the antrum of the stomach, then many small growths appear in this place. You can also often see wide branched ridges and elongated pits, which also indicate the presence of pathology.
Foveal hyperplasia of the stomach is a pathology in which the length and curvature of the folds present on the mucous membrane increase. More often, the cause of its appearance is a prolonged inflammatory process or taking anti-inflammatory drugs without a doctor’s prescription.
As the name implies, with this pathology, the cells that are responsible for the functioning of the glands suffer. Growths form, they are made of glandular cells.
Polypoid hyperplasia is a pathology that is dangerous because it can transform into a cancerous tumor. Another name is hyperplastic polyp. Doctors are concerned about polyps whose size exceeds two centimeters. There can be many polyps, or only one polyp is formed, often serious structural changes begin in its walls.
We figured out what hyperplasia is. It would be quite difficult to make a diagnosis based only on symptoms, so the patient is sent for gastroscopy. An endoscope, which has a light source and cameras, is inserted into the patient's stomach. The doctor can examine the walls of the stomach and note any changes. The doctor also performs a biopsy of the stomach walls. Histology helps to make an accurate diagnosis, exclude oncology, and also helps to identify the type of hyperplasia and the cause of its occurrence.
A gastroenterologist treats gastric hyperplasia; if necessary, he can refer you to an oncologist or a surgeon, but surgical intervention is required in rare cases; conservative treatment is more often prescribed.
If a patient has gastric hyperplasia, treatment is the fight against the underlying disease that caused this pathology. The doctor may prescribe either antibacterial agents if you need to fight an antibacterial infection, or gastroprotectors that protect the gastric mucosa. If the cause of the disease is increased acidity, then drugs that reduce acidity are prescribed. Hormonal medications can also help in those rare cases when the disease is caused by hormonal imbalances.
If there are too many polyps and they have reached a significant size, the doctor may prescribe an endoscopic polypectomy, when they are removed using an endoscope. As a last resort, open surgery is performed on the stomach or part of the organ is removed.
If a person has gastric hyperplasia, the patient is prescribed dietary nutrition, that is, only foods that are safe for the gastric mucosa and do not cause irritation are allowed. The diet largely depends on the underlying disease that caused the appearance of hyperplasia. However, some nutritional rules are suitable for all patients with this pathology, for example, split meals. The patient should eat at least 5 times a day, in small portions. Among the prohibited foods:
- alcohol;
- soda, coffee, strong tea;
- spicy and fatty, fried foods;
- food too hot.
It is useful to eat foods rich in fiber, such as porridge. You shouldn’t give up meat or fish, but it’s better to choose low-fat varieties; rabbit, chicken and turkey are especially healthy. It is advisable to boil or stew everything; you can steam it. If you want to cure a disease faster, diet should become a part of your life.
If the attending physician does not mind, you can also use traditional methods. But a contraindication to their use may be the presence of a particular disease. Therefore, before drinking certain infusions or decoctions, study all the contraindications for each herb that is included in this decoction, and only after that begin treatment.
Stomach diseases are well treated by chamomile, which is an excellent antiseptic. It relieves pain and muscle spasms. Ginger root also has antibacterial properties. Peppermint helps relieve heartburn and nausea.
There are other recipes that help cure hyperplasia, for example, an infusion of parsley roots. To prepare it, take 250 ml of boiling water and pour 1 tbsp. chopped roots, leave to infuse overnight. You need to take this medicine in the morning, afternoon and evening, 1 tbsp. A decoction of fireweed tea is useful. You will need 10 g of chopped herb, which is poured with 250 ml of water. The broth should be boiled for at least a quarter of an hour, then left for 1 hour. Then you need to add water to restore the original volume. You need to drink the decoction 3 times a day, 1 tablespoon, before meals.
It would be a mistake to call gastric hyperplasia a separate disease; it is rather a pathological process that accompanies many diseases (most often gastritis). If these and other symptoms appear, it is better to immediately go to the clinic, get examined and begin treatment. Cured stomach diseases are a guarantee that you will not develop hyperplasia. Proper nutrition and a healthy lifestyle also play an important role. In some cases, timely treatment can save lives, for example, prevent the occurrence of stomach cancer.
source
In medicine, the term “gastric hyperplasia” refers to a pathological process characterized by an increase in the number of cells of the digestive organ. Its mucous membrane thickens, and over time, polyps form on it. There are several forms of the disease. One of the most common is follicular hyperplasia of the gastric mucosa.
The disease is based on cell division, which is normally necessary. But under the influence of various unfavorable factors, an abnormal process of proliferation of epithelial tissue of the digestive system organ is started. During diagnostic procedures, the doctor has the opportunity to visualize areas of the mucous membrane covered with curvatures. The folds of the organ become deformed and their length increases. In addition, the gastric pits also undergo external changes. As a rule, at the initial stage, deformities and growths are discovered randomly during an endoscopic examination prescribed for another reason.
The area most often affected by the disease is the antrum of the stomach. This is explained by the fact that it is this area that experiences the greatest load when digesting food. However, the pathological process may involve the cardia of the stomach, the body, and the fundus. The disease has no specific localization. According to ICD-10, gastric polyps are assigned code D13.1.
A feature of the disease is that the formed neoplasms do not degenerate into tumors of either a benign or malignant nature.
It is important to understand that gastric foveal hyperplasia is a disease that does not occur on its own. The most common trigger for its development is an unbalanced diet and excessive consumption of foods containing carcinogens.
In addition, the following diseases and conditions are the causes of foveal hyperplasia of the stomach:
- chronic pathologies (for example, ulcers or gastritis);
- hereditary predisposition;
- hormonal imbalance;
- the presence of the pathogen Helicobacter pylori in the organ;
- alcoholism;
- long stay in a state of stress;
- improper functioning of the parasympathetic nervous system.
In addition, the disease often develops against the background of long-term use of non-steroidal anti-inflammatory drugs.
It is important to know that foveal hyperplasia of the stomach is such an insidious disease, the danger of which lies in the fact that in the first stages of development it is not accompanied by a deterioration in a person’s well-being. Gradually, the disease progresses and becomes an advanced form, which sometimes cannot be cured with conservative methods.
The danger of the disease also lies in the fact that it does not have specific symptoms. In this regard, it is necessary to immediately consult a doctor if your health worsens.
The main symptoms of foveal hyperplasia of the stomach:
- Pronounced painful sensations. They can be either temporary or permanent. The pain is often accompanied by involuntary contractions of muscle tissue.
- Digestive disorders.
- Loss of appetite.
- Nausea progressing to vomiting.
- Stomach bloating.
- Increased gas formation.
- General weakness.
- Paleness of the skin.
- Increased body temperature.
- Frequent episodes of headaches.
- Feeling of aching in muscle tissue and joints.
The first alarming sign that may indicate the development of foveal hyperplasia of the stomach is pain that occurs at night, when the organ is empty.
If unpleasant symptoms occur, you must make an appointment with a gastroenterologist. The specialist will issue a referral for diagnostics and, based on the research results, will create the most effective treatment regimen.
You should not ignore warning signs, as they may indicate the development of many dangerous diseases. In addition, there are several types of gastric hyperplasia, which can become a provoking factor for the development of malignant pathology.
In most cases, the disease is detected during a routine examination or during a study prescribed for a completely different reason. The difficulty of timely diagnosis of foveal hyperplasia of the stomach lies in the fact that the pathology in the early stages is asymptomatic.
In order to make an accurate diagnosis, the doctor prescribes the following tests:
- FGDS. This is the main way to diagnose pathology. During the examination, the doctor has the opportunity to examine the walls of the organ and identify the extent and nature of its damage. This allows us to assess the scale of the pathological process, since it may involve the area where the antrum of the stomach is located, and areas related to the cardia, body and bottom of the organ. Often during FGDS, biomaterial is collected and sent for histological analysis. This is necessary to exclude the presence of a malignant process.
- X-ray examination using a contrast agent. Its essence is as follows: the patient is asked to drink a certain amount of barium, after which several standard photographs are taken. This allows us to identify the degree of deformation of folds and polyps. When the latter are detected, their sizes and shapes are assessed.
- Ultrasound. This type of research is necessary to establish the root cause of the disease.
In addition, to understand whether polyps in the stomach and deformities are dangerous, the doctor prescribes urine, blood and stool tests. The research results make it possible to exclude the presence of oncology and identify the true cause of the disease.
The choice of treatment regimen directly depends on the disease that caused foveal hyperplasia of the stomach. Very often it develops while taking non-steroidal anti-inflammatory drugs. In this regard, the patient must complete the course of treatment with these medications.
Also often the cause of the development of the disease is the vital activity of the pathogen Helicobacter pylori.
In order to destroy pathogens, doctors prescribe the following medications:
- Antibiotics (for example, Tetracycline, Amoxicillin, Levofloxacin).
- Drugs that reduce the degree of acid production in the stomach (Omez, Pantoprazole).
- Products whose active ingredient is bismuth (“De-Nol”, “Ulkavis”).
The specialist prescribes medications and calculates their dosage individually, based on the results of all studies.
In almost all cases, the development of the pathological process is accompanied by the formation of various types of growths. First of all, the doctor must determine whether polyps in the stomach are dangerous. If oncology is excluded and the formations are small, treatment is not required. It is only necessary to periodically undergo FGDS to monitor the course of the disease. If the growths increase in size, the doctor decides on the advisability of surgical intervention.
If conservative methods of therapy are ineffective, deformed tissues with obvious signs of hyperplasia are removed.
This can be done in several ways:
In the first case, the procedure is minimally invasive. The doctor, through several incisions in the abdominal cavity, inserts endoscopic instruments into the body and removes pathologically altered tissue.
The open method is carried out in the classical way. The doctor uses a scalpel to cut through soft tissue. Having gained access, he removes either the deformed areas or part of the organ, leaving behind a stump of the stomach. After an open operation, the patient needs special care. This is due to the fact that after surgical intervention in this way there is always a risk of developing an inflammatory process in the stomach or suppuration of the sutures.
It is possible to reduce the severity of symptoms of the disease and improve its course by adjusting the diet. In addition, you need to change your diet.
Patients diagnosed with any form of gastric hyperplasia must follow the following rules:
- Portions should be small (about 200 grams), but the number of meals should be increased (up to 5-6).
- It is necessary to consume only those foods that do not have a negative effect on the gastric mucosa. The diet should include porridge, fish and lean meat (of the latter, preference should be given to chicken, turkey and rabbit). All dishes must be boiled, stewed, baked or steamed. Food should be warm.
- Completely avoid fried, spicy, smoked, salted, pickled and canned foods. Ignoring this rule will not only reduce the effectiveness of drug therapy, but will also significantly worsen the course of the disease, since such dishes inevitably irritate the gastric mucosa. In addition, it is strictly forbidden to drink carbonated and alcohol-containing drinks, strong tea, and coffee.
Patients suffering from gastric hyperplasia should make diet a part of their life. Only following its principles will help cure the disease and reduce the risk of relapse to a minimum.
After consultation with a doctor, alternative methods of therapy may be used. The need for a preliminary conversation with a specialist is due to the fact that all medicinal herbs have a number of contraindications. The doctor will help you choose recipes that will improve the course of the disease and reduce the severity of symptoms.
Chamomile, ginger root and peppermint are considered the most effective in the treatment of foveal hyperplasia of the stomach. Products based on them have antiseptic, analgesic and antispasmodic effects. They also negatively affect the activity of pathogenic microorganisms and help relieve nausea and heartburn.
An infusion of parsley roots is also considered an effective remedy. To prepare it you need to take 1 tbsp. chopped plant and pour a glass of boiling water (200 ml). Let it brew for several hours. After this time, strain the product and use 1 tbsp. three times a day.
Gastric hyperplasia is a pathological process that can develop against the background of many ailments. In this regard, it is a mistake to consider it an independent disease. Before treating foveal hyperplasia of the stomach, the doctor must find out the cause of its appearance. If you manage to successfully get rid of the underlying disease, the pathology will recede.
Ignoring the disease can lead to serious consequences. The foveal form of hyperplasia does not degenerate into a malignant disease, but over time, gastric polyps can form on the mucous membrane (according to ICD-10 code, see above). In addition, deformed tissues disrupt the digestion process, and therefore they can become a provoking factor in the development of many other ailments of the digestive system.
The main measure to prevent the appearance of hyperplasia is to control the diet and regimen. This is explained by the fact that very often the cause of the development of the pathological process is a passion for low-quality, fatty, heavy food. In addition, it is necessary to strictly follow the treatment regimen for other diseases, avoid getting into stressful situations and lead an active lifestyle.
Foveal hyperplasia of the gastric mucosa is a pathological process characterized by abnormal proliferation of epithelial tissue cells. The folds of the organ become deformed, their length increases, and sometimes polyps form. The body, fundus, antrum, and cardia of the stomach may be involved in the pathological process.
When the first alarming signs appear, you should contact a gastroenterologist. The doctor will prescribe studies, based on the results of which he will create the most effective treatment regimen, which may include both conservative and surgical methods.
source
All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict sourcing guidelines and only link to reputable sites, academic research institutions and, where possible, proven medical studies. Please note that the numbers in parentheses ([1], [2], etc.) are clickable links to such studies.
If you believe that any of our content is inaccurate, out of date, or otherwise questionable, please select it and press Ctrl + Enter.
Hyperplasia can affect any human organ, but gastric hyperplasia is especially common. Therefore, with any suspicion of gastric hyperplasia, you should not delay, but you should consult a doctor, take all tests, and if the disease is detected, begin treatment immediately.
Hyperplasia is an increase in cell growth in organs, the formation of tumors. It appears most often as a result of cell division, that is, essentially through their normal reproduction, but in large, excessive quantities. Hyperplasia may occur in the tissues of the organ, in the mucous membrane or in the epithelium. In addition, with hyperplasia, not only does the number of cells increase, but also in advanced diseases, changes begin within the cells themselves, their structure irreversibly changes, which can subsequently lead to the degeneration of the changed cells into malignant tumors.
[1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14]
There are many reasons why gastric hyperplasia appears, including:
- hormonal disorders in the body
- advanced chronic gastritis, chronic inflammation in the stomach tissues and mucous membrane
- untreated stomach infections
- disorders of the intrasecretory function of the mucous membrane
- improper nervous regulation in the stomach
- the effect of various carcinogens on the stomach also promotes cell proliferation
- some types of gastric hyperplasia can develop due to the presence of the bacterium Helicobacter pylori in the body
- hereditary predisposition to the disease.
[15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25]
Very often, gastric hyperplasia is initially not accompanied by any obvious symptoms, this is the danger of the disease, because in the absence of any symptoms, a person does not even suspect a progressive disease until it enters a chronic, advanced stage.
Over time, gastric hyperplasia begins to be characterized by the following main signs of the disease:
- severe pain, resulting in involuntary muscle contractions in the patient, sometimes temporary, in chronic cases it can be permanent.
- Possible stomach upset, digestive disorders.
- At times, signs of anemia appear.
You should not postpone the examination if pain begins to appear at night when the stomach is empty; this may well be the first sign of gastric hyperplasia. At the first symptoms, you should consult a doctor; you should never self-medicate, much less let the disease progress by itself, because this is fraught with aggravation and negative consequences. The ideal option is to visit a doctor once every six months for diagnosis, so as not to miss the moment of the onset of the disease and treat it at an early stage.
[26], [27], [28], [29], [30], [31]
Focal hyperplasia of the stomach is an early form of a polyp, manifests itself in the form of a benign tumor in one of the sectors of the stomach, in the so-called “focus”, hence the name. It can have a different size, usually resembles a small growth, with a modified structure, this can be seen especially well during a study with contrast, when paint gets on the foci of hyperplasia, they immediately change color and stand out against the background of normal tissues. The outgrowths may look like a tubercle or have a stalk; they can be single or multiple. They are also called wart hyperplasia.
Most often they are transformed from erosion of the mucous membrane. Detected by endoscopic examination.
[32], [33], [34], [35], [36]
Foveal hyperplasia of the stomach is the proliferation of epitolyal cells in the mucous membrane or tissues of the stomach.
Foveal hyperplasia of the stomach can occur against the background of chronic inflammation of the gastric mucosa, and is classified as a disease that often does not cause the formation of either benign or malignant tumors.
Typically, the onset of the disease is asymptomatic in the early stages, and it is called an “endoscopic finding”, since it is discovered during examination by a doctor quite by accident. Despite being asymptomatic in the early stages, gastric foveal hyperplasia is considered the initial stage of the appearance of hyperplastic polyps.
The antrum of the stomach is most often susceptible to the appearance of hyperplasia, since, firstly, it makes up almost a third of the entire stomach, is located in its very lower part and passes into the duodenum. Its main function is to grind, digest and push food further, so it is more susceptible to stress and disease than other departments. The absence of symptoms at an early stage and the course of the disease in the antrum is the same as in any other, the differences are only in the appearance of the outgrowths. Often, neoplasms in the antrum of the stomach are multiple growths of small size. When studying the morphology, experts identify elongation of the pits and the presence of wide branched ridges.
Lymphofollicular hyperplasia of the stomach is a new formation of cells in the follicular layer of the gastric mucosa. This type of gastric hyperplasia appears mainly due to various disturbances of hormonal processes, improper intrasecretory functioning and violations of correlative connections. Tissue breakdown products that do not decompose in the usual way can also cause the appearance of lymphofollicular hyperplasia of the stomach. In addition, blastomogenic and carcinogenic substances with which the body comes into contact also affect the occurrence of the disease. This disease can develop as a result of negative effects on internal tissues, disturbances of hormonal processes, nervous regulation, correlative connections and improper intrasecretory work. Specific tissue breakdown products that do not decompose in the usual way and carcinogenic substances can enhance the growth of the lymphofollicular layer of the stomach.
Lymphofollicular hyperplasia of the stomach in combination with gastritis is very dangerous for human life. Such a connection can lead to the development of malignant tumors.
Histochemical examination and electron microscopy reveal functional changes in the activity of cellular elements of the mucous membrane. These changes are especially pronounced in the cells of the integumentary epithelium of the stomach; they are increased in size and contain a large amount of mucin inside, which fills the cell and pushes the nucleus to its base. In addition to functional changes, integumentary pitting hyperplasia of the stomach is observed, which leads to the appearance of new gastric pits, which gives them a corkscrew shape. The symptoms are also difficult to diagnose; it is better to seek advice from a specialist.
Focal hyperplasia of the stomach is polyps that appear in connection with a long-term inflammatory process in tissues, epitolyal cells and mucous membranes, with pronounced phenomena of proliferation and degeneration. Typically, such changes are located locally, and this allows them to be easily identified using tests and quickly removed, thereby preventing their reproduction and aggravation of the body’s condition. The stomach has different sections in its structure: the antrum, the cadia, the fundus of the stomach, and the body. And unfortunately, all these departments can be susceptible to various diseases, including gastric hyperplasia.
[37], [38], [39], [40], [41], [42]
Lymphoid hyperplasia of the stomach is an excessive formation of lymphocytes in the lymph nodes. Lymph nodes are very important for the body; they suppress the proliferation of viruses, bacteria, and the spread of malignant processes. Lymphoid hyperplasia is an inflammatory process that involves the lymph nodes themselves and their enlargement, and not just a reaction to inflammation of some other organ.
Based on the location of enlarged lymph nodes, areas of serious disease can be identified. For example, hyperplasia of the lymph nodes in the groin can provoke malignant tumors in the legs or cancer metastases in the genitals.
Lymphoid hyperplasia of the gastric mucosa is a pseudolymphomatous lesion of the stomach, most often occurs against the background of a chronic ulcer, but thickening of the mucous membrane, nodular growths that can penetrate into the mucous membrane and even into its deeper balls can also be observed. It is also possible for polyps to form in the mucous membrane. Lymphoid hyperplasia is difficult to diagnose; it is characterized by the absence of atypical cells, the presence of signs of stromal fibrosis, and the nodular nature of formations in the submucosal and muscular layers.
Glandular hyperplasia of the stomach is an excessive formation of glandular endometrial tissue, manifested in its thickening and increase in volume.
Hyperplasia of the gastric glands is detected in the form of small polypous growths, mostly round or oval in shape, surrounded by a mucous membrane altered at the cellular level.
The body of the polyp consists of glandular elements or of overgrown integumentary epithelium and vascular-rich connective tissue, as well as a stalk, which is a continuation of the adjacent mucous membrane and submucosal layer.
The glandular elements of benign polyps are similar to the surrounding tissue, the epithelium is not very changed. In some places, the glands can expand into cystic cavities. The glands never extend beyond the muscular membrane, no matter how extensive the glandular hyperplasia is.
A polyp is a small tumor in the tissues or mucous membrane, it can be “sessile” or located on a stalk, be single or multiple, and has a different morphological structure.
Polyps with gastric hyperplasia can appear in any part of the stomach, the reasons are standard - advanced stomach disease, although many scientists consider the reasons for their appearance unknown. According to statistics, people over 50 years of age are most often predisposed to polypoid hyperplasia, but unfortunately, every year statistics show that polyps have begun to affect the younger generation. Such growths are often removed surgically.
source
Etiology
Gastric hyperplasia develops due to unfinished treatment of diseases of the gastrointestinal tract. As a result, active cell growth begins and polyps appear.
The main causes of hyperplasia:
- changes in hormonal balance, especially when the amount of estrogen is increased;
- genetic predisposition, in particular adenomatous polyposis (characteristic of polyps in the stomach) - if the pathology is diagnosed in a woman, the disease can be inherited by a daughter or granddaughter;
- long-term use of medications that can affect changes in the structure of the gastric mucosa;
- unfavorable environment - a pathological increase in the number of cells may begin.
The cause is the bacterium Helicobacter pylori and other infectious diseases.
Folk remedies for gastric hyperplasia
Very often, people try to cure gastric hyperplasia with folk remedies, without resorting to the help of doctors. This poses a threat to their health and life, since some types of hyperplasia can cause the development of stomach cancer. Therefore, you can resort to folk remedies only with the permission of a doctor. Typically, most of these prescriptions are aimed at reducing the acidity of gastric contents and eliminating H. pylori infection.
Many plants are used for this, for example:
- Ginger . It has anti-inflammatory and antibacterial properties, reduces inflammation and relieves symptoms such as abdominal pain, bloating, flatulence and nausea.
- Chamomile . It is rich in substances beneficial to the digestive tract, which reduces abdominal pain and eliminates excess gases from the intestines, relieves inflammation in the stomach and reduces the risk of ulcers.
- Peppermint . It has anti-inflammatory, antibacterial and antispasmodic properties, reduces inflammation in the stomach, relieves nausea and heartburn.
Gastric hyperplasia is not a disease, it is a histological characteristic of a pathological process in its mucous membrane during a certain disease. Most often it develops with chronic gastritis caused by H. pylori infection. A common form of gastric hyperplasia are polyps. Treatment depends on the cause and type of pathological changes in the mucous membrane.
Classification
In medicine, experts distinguish between many different types of hyperplasia:
- Focal developing hyperplasia of the gastric mucosa. The first stage of development of the anomaly, when certain polyps begin to appear. Focal diagnosed hyperplasia of the stomach covers only some areas (“foci”), which is why it got its name. The lesions look like growths of various shapes and sizes, painted in a different color, so they are clearly visible during examination. Formations arise at the site of previously received damage or erosion.
- Follicular identified gastric hyperplasia. This type of pathology is often diagnosed. Lymphatic cells begin to grow. The reasons for the development of the anomaly are different: the influence of carcinogens, hormonal imbalance, the presence of the bacterium Helicobacter pylori, stressful situations and much more. A distinctive feature of this type of disease is the formation of follicles in the stomach.
- Hyperplasia of the integumentary pitted epithelium of the stomach. A dangerous type of pathology that can contribute to the appearance of a malignant tumor in the intestine. The structure of the epithelium changes under the influence of unfavorable factors: cells grow and become larger.
- Hyperplasia involving the antrum of the stomach. The antrum is the last part of the organ before it exits into the intestine. In this place, with the development of hyperplasia, multiple small growths, pits and ridges begin to form.
- Foveal hyperplasia of the gastric mucosa. This type of pathology is characterized by an increase in the length of the folds of the mucous membrane and an increase in their curvature. Pathology occurs due to prolonged inflammation or self-administration of anti-inflammatory drugs.
There are also other types of pathology: glandular, polypoid, lymphoid.
Superficial gastritis: types, causes of development and symptoms of the disease
The most common form of stomach inflammation, the symptoms of which, to one degree or another, can be found in every resident of megacities, is superficial gastritis. This is a particularly insidious type of pathology, affecting only the cells of the mucous epithelium, but slowly and surely preparing the ground for more severe manifestations.
Superficial gastritis is identified as the initial stage of the chronic course of the disease, the diagnosis and treatment of which does not present any difficulties. The insidiousness of this stage lies in the vague symptoms. Unexpressed pain, belching and nausea, a feeling of fullness in the stomach after eating, these are symptoms that few people will cause concern. And it is considered not at all decent to address such complaints to a doctor.
As a result, a chronic relapsing process gradually develops and turns into more severe forms, in which the following is disrupted:
- digestive;
- secretory;
- motor functions of the stomach.
Treatment of superficial gastritis, with timely contact with a gastroenterologist, can be carried out without medications. A strict diet, a reasonable alternation of work and rest, as well as a categorical refusal of bad habits, will allow the mucous membrane to recover on its own.
Unfortunately, the vast majority of patients come to see a doctor when prolonged inflammation has caused pathological changes, the mucous membrane has undergone degeneration, changes have affected the glandular layer, insufficiency of the cardia and duodenum has been added - gastric reflux, and superficial gastritis has passed into a more complex stage of the disease, hypertrophic or atrophic.
Causes and types of disease
The mechanism of damage has been seriously studied for many centuries. Today it has been reliably established that, due to the occurrence of superficial gastritis, it can be divided into three main groups, these are:
- Autoimmune “A” - inflammation of the mucous membrane occurs due to malfunctions of the immune system, when protective molecules begin to recognize the cells of the gastric mucosa as hostile substances.
- Bacterial “B” - the cause of the pathology in this case is infection with the bacteria Helicobacter pylori. Gastroenterologists say that this is the most common type of inflammation, which is almost impossible to treat without drug therapy.
- Reflux “C” is an inflammatory process on the surface of the gastric mucosa that begins due to insufficiency of the lower sphincter, which should prevent the return of food from the duodenum. Duodeno-gastric syndrome is as often the cause of inflammation of the internal surface as bacterial infection.
According to localization, superficial gastritis can be of the following types:
- Cardiac type, when the source of inflammation is located in the cardiac part of the stomach, that is, in close proximity to the esophagus. Most often it develops accompanied by dysfunction of the cardia (upper sphincter). This type of gastritis is most often diagnosed at the very beginning of development, since the failure of the cardia is accompanied by frequent spontaneous attacks of vomiting and “sound design” - gurgling, seething. Heartburn with superficial gastritis with cardia insufficiency constantly torments the patient, which forces him to quickly consult a specialist. Typically, cardiac gastritis occurs together with inflammation of the esophagus, that is, as gastric esophagitis.
- Fundal type, affects the fundus of the stomach. Inflammation of this section is usually not accompanied by the phenomenon of reflux (reflux) of contents into the esophagus, even if there is a slight deficiency of the cardia.
- Antral type, inflammation of the outlet, antrum of the stomach can develop both as “B” gastritis, since bacteria primarily settle in this area, and as toxic-induced “C” gastritis. Duodeno gastric reflux is a symptom that almost always accompanies superficial antrum gastritis. It can also be the main cause of inflammation of the antral mucosa. Superficial reflux gastritis or duodeno-gastric type of pathology is insidious due to the functional characteristics of the antrum of the stomach. A decrease in the acidity of the food bolus and increased motility, necessary for the evacuation of contents into the duodenum, creates ideal conditions for the life of Helicobacter pylori and the spread of inflammation throughout the intestines.
- Pangastritis is the most unpleasant form of superficial inflammation, in which the pathology covers the entire inner lining of the body of the stomach. In most cases, with superficial pangastitis, the cardiac valve, the pylori sphincter, and the duodeno-gastric region are involved in the pathological process.
According to the prevalence on the gastric mucosa, superficial gastritis can be:
- Focal, when the inflamed areas are located in the form of small foci.
- Diffuse, when the pathology covers the entire area of the affected area. The diffuse type of pathology, despite the damage to large areas, is less dangerous than focal. Diffuse superficial gastritis has longer periods of calm, and its spread occurs along the mucosal epithelium. While the focal type of lesion very quickly begins to penetrate into the deep tissues, affecting the glands and muscles.
Symptoms
The picture of symptoms that superficial gastritis gives directly depends on the location and extent of inflammation.
Inflammation in the cardiac part of the stomach with severe cardia insufficiency is characterized by strong and frequent belching, which occurs even after drinking plain water. This is accompanied by prolonged bouts of heartburn with a bitter taste. If cardia insufficiency is accompanied by a diffuse type of inflammation, then in addition to heartburn and belching, the patient will feel mild pain on an empty stomach, similar in nature to cramps.
For lesions of the fundus, nausea is more common both on an empty stomach and immediately after eating.
Focal fundal superficial gastritis is dangerous, since its symptoms can appear only after the inflammatory process spreads into the deep layers of the stomach lining with the formation of atrophic foci. Treatment of such gastritis should be started immediately, as the disease progresses quickly.
Antral superficial gastritis is the most common form of the disease, occurring in more than 60% of patients. Paradoxically, superficial antrum gastritis is diagnosed most often during preventive examinations or the appointment of an FGDS (fibro-gastro-duodenoscopy) for another reason.
Colonization of bacteria in the antrum occurs slowly and unnoticed by the patient. Helicobacter actively reproduces without showing its presence with negative symptoms. This is facilitated by the deep location and small number of nerve endings that can send a pain signal. Superficial gastritis does not disrupt gastric motility, which helps pathogenic flora to easily penetrate the intestines, where their main phase of life begins.
The picture on the FGDS monitor during the study in almost 90% of cases shows the presence of not only destruction of the antral portion of the mucosa, but also gastric duodenitis. Unlike insufficiency of the cardia, that is, the upper sphincter, in which reflux occurs into the esophagus, duodeno-gastric reflux directs intestinal contents into the stomach, and at the same time provokes stagnation of the food bolus. This will provoke not only a diffuse inflammatory process, but also putrefactive phenomena in the stomach.
Treatment of pathology
Treatment of superficial gastritis, as with cardia insufficiency, existing duodenal gastric reflux, always begins with adjusting the diet. The chronic process, both diffuse and focal, with the right diet, followed constantly, goes into remission for a long period, which can be calculated in years.
The immune system is able to independently restore cells destroyed by inflammation, without the help of medications. The exception is superficial gastritis “B”. It is quite difficult for the body to get rid of bacterial colonies.
If the pathogenic flora is found only in the stomach, and its reproduction has not reached a global scale, probiotics are prescribed, which help strengthen the beneficial microflora. But if the examination shows existing duodenitis and duodenal gastric reflux, it is useless to treat gastritis without a course of antibacterial therapy.
Practicing gastroenterologists advise treating superficial gastritis comprehensively, simultaneously influencing the pathology in several directions, these are:
- Adjusting your diet.
- Normalization of acidity using drugs such as ranitidine and omez.
- Increasing protective mucus with Maalox and Almagel.
- Normalization of motor skills - motilium.
- Vitamins and medicinal plants, such as aloe and sea buckthorn oil to stimulate tissue regeneration.
Important! Deciding on your own how and with what to treat gastritis is dangerous not only for health, but also for life. Only a specialist can determine the type of superficial gastritis using modern diagnostic methods and prescribe the treatment that is suitable for this particular case.
Symptoms
In the first stages of the development of the disease, it is very difficult to identify the pathology, because there are practically no symptoms: an increase in the number of cells does not cause discomfort to a person, there is no pain even when small polyps appear. When they increase, difficulties begin with the passage of food, which can cause severe bleeding or pain.
As the disease progresses, disruptions in the functioning of the stomach begin, and these are problems with digestion. The following symptoms begin to appear:
- constant or short-term pain that occurs after eating, sometimes during prolonged fasting;
- heartburn;
- flatulence and constipation;
- sour belching;
- nausea and vomiting;
- refusal to eat;
- general weakness, body aches, dizziness;
- anemia.
If such symptoms occur, you should consult your doctor so that the doctor can prescribe an examination.
Gastric hyperplasia
Hyperplasia is a pathological phenomenon in which cell tissue of an organ grows. Gastric hyperplasia is a disease in which this process leads to thickening of the mucous membrane and the formation of polyps on it.
How dangerous is this disease, what clinical signs indicate its presence, how to diagnose and treat pathological growth of the inner lining of the stomach.
Gastric hyperplasia occurs as a result of the following factors:
- Gastritis - when the inflammatory process is permanently present on the mucous membrane, cell division is disrupted and, consequently, thickening of the mucous membrane occurs.
- Hormonal disorders - first of all, we are talking about excess production of estrogen.
- Hereditary diseases - for example, adenomatous polyps of the gastric epithelium.
- Pathology of hormonal regulation of the stomach - with a Zollinger-Ellison tumor of the small intestine, a hormone is released into the blood, which causes hyperplasia of the upper digestive tract.
- Taking medications - non-steroidal anti-inflammatory drugs and proton pump inhibitors to reduce stomach acidity.
Gastric hyperplasia is often asymptomatic, so diagnosis of pathology at an early stage statistically occurs by chance, during gastroscopy of the stomach as part of confirmation of another pathology.
If signs of hyperplasia are present, the clinical picture may include:
- pain of any characteristic in the epigastric region;
- sour belching;
- nausea and vomiting;
- bloating;
- feeling of fullness in the stomach even after a sip of water;
- decreased appetite;
- hiccups
Obviously, the proliferation of mucosal tissues is similar in symptoms to the manifestations of chronic gastritis. But sometimes the clinical manifestations of the pathology may differ if ulcers form on the polyps. In this case, a person will experience signs of internal bleeding:
Diagnostics
During the examination, the medical officer collects the patient’s medical history and clarifies the complaints. It is impossible to establish a correct diagnosis using these data alone. Other studies are prescribed:
- gastroscopy - using an endoscope tube inserted into the stomach, the walls of the organ and polyps are examined;
- biopsy - a histological examination will establish an accurate diagnosis; using the procedure, the type of pathology and the main cause of the development of the anomaly are determined.

After an accurate diagnosis is made, effective treatment is prescribed.
Treatment
Gastric hyperplasia is treated by a gastroenterologist. If necessary, the patient may be scheduled for a consultation with an oncologist or surgeon. Surgery is performed only in extreme cases; usually the treatment regimen is limited to taking medications.
- Drug therapy. Treatment of gastric hyperplasia is aimed at eliminating the underlying cause of the pathology. If the anomaly has developed due to a bacterial infection in the body, the person is prescribed antibacterial drugs. To protect the mucous membrane, the doctor prescribes gastroprotectors. A gastroenterologist may prescribe medications to reduce acidity if the patient's test results show an elevated pH. The doctor prescribes hormonal medications when the disease is associated with hormonal imbalances.
- Carrying out surgery. If too many polyps of a significant size appear, the growths may need to be removed. Usually limited to endoscopic polypectomy. In severe cases, open gastric surgery is performed or part of the stomach is removed.
- Diet. The patient must adhere to dietary nutrition. You can only eat food that does not harm the mucous membrane. The menu will depend on the primary disease that caused the pathology. Fractional nutrition is suitable for any patient with such a deviation, regardless of the cause of the development of the anomaly. There should be up to 5 meals per day, small portions. List of products whose consumption is not recommended: alcohol, strong tea, coffee, carbonated drinks. Lean fish and meat, cereals are useful. It is better to cook if the food is steamed, stewed or boiled. Fried and spicy foods should be excluded from the diet. Hot dishes cannot be eaten. A strict diet will help you recover faster.
- Traditional medicine recipes. Can only be used in combination with traditional medicine after consultation with a doctor.
The method of treatment is selected individually. You should not self-medicate, because this can lead to irreversible consequences and serious complications.
Symptoms and treatment of esophageal hyperplasia
Hyperplasia of the esophagus, like any other organ, should be understood as the proliferation of its tissues with the possible replacement of an anatomically natural cellular structure with another (pathological) one.
In terms of changes in the esophagus, it is customary to speak of its hyperplasia if the epithelium of its inner wall (stratified squamous) is replaced by epithelial tissue, which is characteristic of the wall of the stomach (cylindrical epithelium).
Cellular hyperplasia of the esophagus was described in the middle of the last century by the English doctor Barrett. Subsequently, this type of change in the cellular structure of the esophagus began to be called Barrett's esophagus.
Causes of esophageal hyperplasia
The main cause of cellular transformation of the esophageal mucosa is its chronic chemical damage. This effect appears against the background of a long course of gastroesophageal reflux disease. In this case, the natural motility of the digestive tract is disrupted and the acidic contents of the stomach are constantly thrown into the upper esophagus.
What changes occur in the esophagus?
As chemical damage increases (enzymes of gastric juice, hydrochloric acid, bile acids, duodenal secretions), damage and subsequent destruction of the multilayered squamous epithelium typical of the esophagus is noted.
The resulting site of damage is first replaced by progenitor stem cells, which transform into columnar epithelium, which is typical of the gastric mucosa.
Columnar epithelium is much more resistant to the effects of chemically aggressive compounds, therefore, during the process of cell transformation, a person usually does not feel any discomfort or even, on the contrary, a decrease in pain.
Subsequently, in many patients, the process of cellular transformation continues, that is, the columnar epithelium in the esophagus turns into malignant tumor cells. As the size of the cancer increases, symptoms associated with difficulty swallowing and bolus passage increase.
The causes of malignant transformation of the epithelium in esophageal hyperplasia are not fully understood. It has been suggested that this process is genetically determined.
Diagnosis of esophageal hyperplasia
Symptoms typical of esophageal hyperplasia have not been described in the medical literature to date. Therefore, the greatest importance in diagnosing such cellular transformation is the periodic examination of patients suffering from gastroesophageal reflux disease, since the likelihood of epithelial hyperplasia increases as the “experience” of the disease increases.
On the other hand, with instrumental examination it is quite easy to identify morphological changes typical of esophageal hyperplasia, namely:
1. An X-ray examination reveals: the so-called mesh pattern of the inner lining of the esophageal tube, ulcerative changes in the lower third of the esophagus (the so-called Beretta ulcer) and a hiatal hernia.
2. When performing fibrogastroduodenoscopy, one of the supporting criteria for diagnosis is visualized, the so-called velvet mucosa and inflammatory changes of varying degrees of prevalence.
3. The final confirmation of esophageal hyperplasia is the result of a biopsy followed by a study of the cellular composition of the samples taken (at least in four zones located a few centimeters from each other).
4. Currently, immunochemical methods are increasingly used in practical healthcare, namely the detection of sucrazuisomaltase (specific to the Beretta esophagus).
5. When performing chromatography, a peculiar mosaic pattern of the mucous membrane is noted; areas with columnar epithelium are intensely stained, in contrast to the normal mucous membrane of the esophageal tube.
6. Esophagomanometry and pH monitoring helps to identify impaired motility and acidity levels in the lower esophagus.
7. Radioisotope research is of an auxiliary nature, most informative in the process of differential diagnosis of Beretta esophagus and malignant neoplasms.
Principles of treatment
The main condition for the treatment of esophageal hyperplasia is the therapy of gastro-esophageal reflux, which provokes cellular changes. For this, a whole range of drugs is used: antacids, prokinetics, proton pump inhibitors.
Treatment is only surgical. The extent of surgical intervention depends on the size of the malignant lesion, the presence of changes in the nearest lymph nodes and the formation of distant metastatic foci.
https://pishevod-wiki.ru/giperplaziya-pishhevoda.html
Source: https://medprevention.ru/pishchevarenie/zheludochno-kishechnyj-trakt/4905-simptomy-i-lechenie-giperplazii-pishchevoda
Causes
The main cause of mucosal hyperplasia is damage that occurs during long-term gastroesophageal reflux disease . In this case, the natural functioning of the digestive system changes, and the contents of the abdominal cavity constantly enter the esophagus.
Surgical
Surgical intervention is also prescribed, the scale of which depends on the size of the lesion. In addition, surgeons take into account the presence or absence of other pathologies and enlarged lymph nodes.
Folk remedies
As an additional method of treating the disease, the following traditional medicine can be used:
- Sea buckthorn oil. A spoonful of oil should be consumed 30 minutes before each meal.
- St. John's wort infusion. The decoction should be drunk in the morning and before bed (2 liters of plant per 2 tablespoons of boiling water).
- Horseradish. The patient should eat a spoonful of horseradish with honey before meals.
Diet food
Both during therapy and during the prevention of the disease, you should eat properly, since often eating harmful, fatty, salty and smoked foods in large quantities leads to the development of pathology. The occurrence of the disease is influenced by a violation of the daily diet.
This provokes disturbances in the functioning of the digestive system. To create a therapeutic diet plan, you should seek advice from a therapist or specialized specialists (for example, nutritionists).
They will refer you for an examination, and then help you select a list of products that can have a beneficial effect on the gastrointestinal tract, and prohibit junk food.
Prevention
Recommendations that should be followed to avoid the onset of the disease include maintaining a proper diet, exercise, regular examination and timely treatment of signs of the disease. The doctor gives more detailed information and advice regarding prevention depending on where the pathology is localized.
Source: https://PishcheVarenie.ru/pischevod/zabolevaniya/giperplaziya-pishhevoda.html
Prevention
Basic preventive measures for hyperplasia:
- healthy and balanced diet;
- active lifestyle;
- rejection of bad habits;
- use of medications only as prescribed by a doctor;
- regular preventive examinations;
- urgent treatment of gastric diseases.
Depending on the area of intestinal damage, the gastroenterologist will recommend individual methods of prevention to the person. Self-medication is excluded - you need to consult a doctor at the first symptoms of pathology.
source
Lymph node hyperplasia
Benign and malignant. Based on where the lymph nodes are enlarged, in some cases we can talk about cancer of the internal organs. For example, if the lymph nodes in the groin are enlarged, it is necessary to check the genitals.
Compresses are widely used in the treatment of lymph node hyperplasia
- Compresses are widely used in the treatment of lymph node hyperplasia. Pour boiling water over ten crushed walnut leaves so that it covers the raw material. After half an hour, strain. Moisten the compress cloth and apply it to the inflamed lymph node for twenty minutes. Repeat twice a day.
- Boil one spoonful of sorrel in a liter of white grape wine for five minutes. Leave to infuse for half an hour. Soak a linen cloth in the broth and place it on the lymph node.
- Lubricate the lymph node with an ointment prepared from two hundred grams of visceral fat and St. John's wort. Melt the fat and add three tablespoons of St. John's wort to it, place in a water bath for four hours. Pour the still hot ointment into a glass jar and screw the lid on tightly. The ointment should be used three times a day.
- Pour a quarter cup of hazel leaf and hazel bark into a liter of boiling water. Wrap in a warm cloth and leave to steep for one hour. Then strain and drink fifty milliliters four times a day.
Hyperplastic antral gastritis: how dangerous is pathological proliferation of the mucous membrane?
Hyperplastic gastritis is a lesion of the stomach, in which increased proliferation of the mucosal epithelium occurs, thick folds and polyps are formed. The antrum is most often affected. The pathology is of a secondary type, developing against the background of other processes. Antral gastritis with hyperplasia of the lining membranes accounts for about 5% of the total number of gastrointestinal diseases.
The structure of the stomach and the location of the antrum
Etiology
A common cause of mucosal damage is atrophic gastritis of autoimmune origin. The body produces antibodies to parietal cells, which is accompanied by their death and atrophy of the mucous membrane (SM). At the same time, hyperplasia of the lymphoid intramural tissue occurs.
In addition to the above, the following diseases and conditions cause the growth of CO:
- Menetrier's disease (giant hypertrophic gastritis) - an increase in the thickness of the inner layers of the stomach up to 2-3 cm.
- Zollinger-Ellison syndrome - gastrin production due to hormone-producing pancreatic tumors.
- Hypertrophic hypersecretory gastropathy - glandular hyperplasia without gastrinemia. Often accompanied by peptic ulcer.
With hyperplastic processes in the antral zone, inflammatory phenomena are mild or completely absent. Changes in the thickness of CO and its cellular composition come to the fore. Like most hyperplasias, the disease in question is considered a precancerous condition.
Clinical signs and diagnosis
Hyperplastic gastritis of the antrum (HAG) differs somewhat in course depending on what kind of process is taking place.
In the atrophic form, the patient experiences the following symptoms:
- heaviness in the epigastrium after eating;
- feeling of overeating;
- decreased appetite;
- unpleasant taste in the mouth;
- dyspepsia.
Up to a certain point, the disease can be asymptomatic. GAG often develops together with thyroiditis and B12-deficiency anemia.
The hypertrophic variety manifests itself in the form of:
- aching pain in the epigastric area;
- heaviness after eating;
- diarrhea;
- vomiting.
Appetite decreases significantly, up to anorexia. The patient may lose up to 20 kg of weight in a short time. Some patients experience peripheral edema. The reason for this phenomenon is the loss of a large amount of protein with gastric secretions due to insufficient absorption from food. Erosions may form.
The main diagnostic method is FGDS (fibrogastroduodenoscopy). With Ménétrier's disease, gigantic folds are found in the stomach, which outwardly resemble the convolutions of the brain. There are erosions and a large amount of mucus. SO atrophy is characterized by its pallor, smoothness, and visual decrease in volume. Hyperplastic processes at the initial stage occur in the depths of the outer layer. During the study, tissue is taken for biopsy.
Note: The examination of a biopsy specimen is considered reliable only if all layers of the mucous membrane and a plate of muscle tissue are present. Otherwise, it is impossible to speak unequivocally about the absence of hyperplasia, even if there are no visual signs of it.
Treatment
Hyperplasia of the gastric antrum requires diet and pharmacological therapy. Dietary restrictions vary. In case of mucosal hypertrophy, it is recommended to eat fractionally, chemical, thermal and mechanical sparing. With the atrophic type of pathology, food should be mechanically gentle, but stimulate the secretion of gastric juice.
Drug therapy is carried out using drugs from the following groups:
- m-anticholinergics;
- proton pump inhibitors;
- means of replacement treatment for insufficiency of secretory function;
- drugs to suppress immunity in the autoimmune nature of the disease.
Severe hyperplasia with a high risk of malignancy is treated surgically. Depending on the extent of the process, complete or partial resection of the stomach is performed. Subsequently, the patient is prescribed lifelong therapy aimed at compensating for lost digestive functions.