If a person is healthy and no pathological changes occur in his body, the intestinal microflora does not change and continues to work normally. If there is any disease that affects the intestines, or an infectious process that requires the use of antibiotic therapy, it is the intestinal microflora that will suffer first. Usually in such situations, intestinal dysbiosis develops. It is necessary to analyze stool for dysbacteriosis.
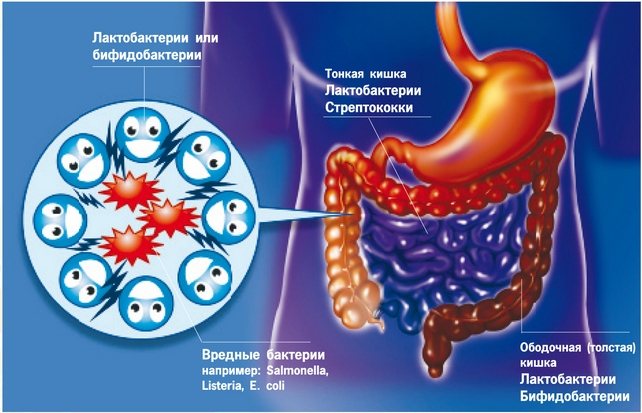
The human intestine is a rather complex and unique organ. Absorption of most nutrients, parietal and cavity digestion occurs here. All this is typical for the small intestine. However, an equally important section is the large intestine. Its main feature is that its cavity is inhabited by microorganisms - various opportunistic bacteria.
In general, both bacteria and humans are in a state of symbiosis. Bacteria receive from a person a nutrient substrate with which they can live and function, and back from them a person receives some vitamins that can only be synthesized by these microorganisms. In addition, bacteria help a person in the normal absorption and processing of food through fermentation processes.
Dysbacteriosis: what causes it?
Normally, the intestinal microflora has a relative constancy of its composition. As a result of a change in the state of the body (most often against the background of immunodeficiency), opportunistic microorganisms (bacteria that, under certain conditions, become capable of developing an infectious process) are activated. Because of this, normal fermentative bacteria are displaced, which leads to digestive disorders and the development of dysbacteriosis.
Its main clinical manifestations will be flatulence, bloating (due to the predominance of putrefactive processes), nausea, vomiting, and loose stools. Over time, with long-term dysbacteriosis, metabolic processes may be disrupted (dry skin, brittle nails and hair, muscle weakness, cramps, etc.). If such symptoms appear, you should definitely seek advice from a physician or gastroenterologist.
Children are especially affected by this condition. They may have physiological dysbiosis, but it is typical only for the neonatal period. By the age of one year, a colony of bacteria that promote digestion should already have formed in the baby’s intestines. If this does not happen, the child may experience developmental delays. In this regard, at the first signs of dysbiosis, an examination of the intestinal condition should be carried out.
In order to assess the condition of the bacteria, certain studies should be carried out.
Stool analysis for dysbacteriosis: explanation
First of all, a stool test or coprogram is prescribed.
This analysis is prescribed to almost everyone due to its simplicity and low cost. The result is usually known the very next day, and it can be carried out in any medical institution equipped with even a small laboratory.
Few people know how to take a stool test.
It is necessary to decide what interests the doctor in this analysis. First, you need to evaluate the color of the stool. Normal stool is characterized by a brown tint. Any color changes (pallor, change in hue, for example to yellow, may be considered pathological). Most often, the cause of color change can be the activity of pathogenic flora.
After visually assessing the color of the stool, it is necessary to assess the consistency of the stool. Normally, stool should be “sausage-shaped.” A change in consistency (for example, loose stools) may indicate an infection of the large intestine (most often cholera).
At the initial laboratory stage, the presence or absence of pathological impurities should be determined. These include mucus, blood, undigested food debris or fiber.
Mucus in the stool often indicates the development of pathology in the sigmoid colon. Blood appears as a result of:
- Development of ulcers (for example, duodenum or colon in ulcerative colitis).
- Bleeding (a clear admixture of blood indicates the presence of a bleeding wound in the intestinal wall, which again could develop due to ulceration and progression of pathogenic microflora) When bleeding from the upper intestines, an occult blood test is required.
Undigested fibers, especially if they are accompanied by an unpleasant, putrid odor, indicate a predominance of rotting over fermentation in the intestines (this is already an indirect factor of dysbiosis).
If the analysis results in stool that is a different color than brown, has an incorrect consistency, and has an unpleasant odor, stool should be cultured to determine the quantitative composition of microorganisms.
What is dysbiosis
Dysbiosis is an imbalance of bacteria living in the intestines under the influence of various factors (taking antibiotics, poor nutrition). Recently, pathology is often observed in very young children.
The intestines are the habitat of beneficial and neutral bacteria
Features of the disease in newborns and infants
The risk group includes the following categories of children:
- premature;
- those who are bottle-fed;
- children whose mothers received antibiotics during pregnancy or breastfeeding;
- late applied to the breast.

Breastfeeding is a reliable prevention of dysbiosis
In babies who receive breast milk, dysbiosis develops much less frequently. Their intestinal microflora consists of 90% lactobacilli and bifidobacteria.
Signs of impaired intestinal microflora in newborns and infants are as follows:
- bloated stomach;
- bad breath;
- stomach ache;
- formation of gases in the intestines;
- secretion of a large amount of saliva;
- dry and tight skin;
- the appearance of allergic rashes on the skin;
- inflammation of the oral mucosa;
- signs of thrush in the mouth;
- difficult stool;
- diarrhea for three or more days;
- vomiting after eating;
- problems gaining weight;
- greenish foamy stool, possibly blood.
According to the World Health Organization, imbalance of intestinal microflora is not a disease. Some foreign experts suggest not interfering with this condition and allowing the body to independently regulate this process. However, most doctors are of the opinion that therapy is still necessary.
To fully evaluate bowel function in a newborn or breastfed infant, the following tests must be performed:
- coprogram (reveals the digestive activity of the intestine, inflammatory processes);
- sowing stool for opportunistic flora (shows how many neutral bacteria are in the intestines);
- tank. stool culture for dysbacteriosis (reveals the percentage of normal and opportunistic intestinal microflora).
According to some experts, it is incorrect to talk about dysbiosis in newborn babies. Children are born with a sterile intestine, which is gradually colonized by bacteria, so it is difficult to judge their normal ratio and quantity.
Causes of imbalance of intestinal microflora in adults and children
Dysbacteriosis can develop in children of preschool and school age, as well as in adults. Most often, the following reasons lead to this condition:
- taking antibiotics;
- eating disorder;
- the presence of a large amount of sweets in food, lack of coarse plant fiber;
- changing your usual food and water when moving to another area;
- infectious intestinal diseases (shigellosis, salmonellosis);
- general decrease in immune system activity;
- operations on the stomach and intestines;
- inflammatory diseases of the stomach and intestines (gastroenterocolitis).
Dysbacteriosis in men and women usually has the same causes. However, the following factors can also contribute to the development of pathology in the fairer sex:
- women's passion for strict diets;
- frequent bowel cleansing using enemas;
- addiction to laxatives for the purpose of losing weight;
- more active treatment with antibiotics.
What signs may indicate the presence of pathology?
Symptoms of dysbiosis in adults and children of preschool and school age:
- bloating and abdominal pain;
- decreased appetite;
- nausea and vomiting;
- undigested pieces of food in stool;
- the appearance of a white coating on the tongue;
- bad breath;
- decreased vitality, fatigue;
- periodic acute abdominal pain;
- dry and brittle hair;
- the appearance of bleeding gums and dark plaque on the teeth.
Microbiological examination of stool will show the ratio of microorganisms in the intestine
To confirm objective signs of dysbiosis, it is necessary to do a microbiological examination of stool. This analysis will show the concentration and ratio of beneficial microorganisms (bifidobacteria, lactobacilli, bacteroides) and opportunistic ones, as well as the presence of pathogenic bacteria (shigella, salmonella).
Doctor Komarovsky about dysbiosis - video
Stool analysis: deciphering the culture
Stool culture on special microenvironments is the main method for diagnosing intestinal diseases. It allows you to assess the qualitative composition of the intestinal microflora and determine the predominant group of bacteria.
Sowing is carried out on media, often consisting of natural components. One of the most commonly used media is meat peptide agar or broth.
Cultures are carried out under sterile conditions to prevent the introduction of foreign microorganisms and misinterpretation of the results.
Colonies of microorganisms usually grow within a week, although some samples can be obtained as early as the next day. By assessing the formed colonies, conclusions are drawn about what microorganisms formed them, and, accordingly, whether the patient has dysbacteriosis.
Normally, the intestines should contain:
- lactobacilli;
- bifidobacteria;
- saprophytic staphylococci;
- some enterococci;
- and Escherichia.
Normally, their content is different, but the point is to detect in the analysis not only them, but also other pathogenic microorganisms. These include:
- clostridia;
- Giardia;
- Vibrio cholerae;
- Haemophilus influenzae.
When they grow on media, it is already possible to make a diagnosis of dysbiosis and begin appropriate treatment.
Culture on media is the most widely used method for determining the bacterial composition of the intestine. However, the disadvantage of this procedure is the rather long time required for the bacteria to grow. Because of this, express methods for diagnosing dysbiosis have been created, allowing results to be obtained directly on the day of the study.
Normal data
For both children and adults, there are clear standards for how many and what bacteria should be in the intestines.
By analyzing stool for dysbacteriosis, you can accurately determine whether there are deviations and how critical they are.
The table below will help you understand which decoding will reflect the normal state of the intestinal microflora.
READ Increased fecal calprotectin - what does it mean?
| Pathogenic enterobacteria | For adults | For babies | For older children |
| Bifidobacteria | 108 – 1010 | 1010 – 1011 | 109 – 1010 |
| Lactobacilli | 106 – 108 | 106 – 107 | 107 – 108 |
| Escherichia | 106 – 108 | 106 – 107 | 107 – 108 |
| Bacteroides | 107 – 108 | ||
| Peptostreptococci | 105 – 106 | 103 – 105 | 105 – 106 |
| Enterococci | 105 – 108 | 105 – 107 | 105 – 108 |
| Saprophytic staphylococci | ≤104 | ||
| Pathogenic staphylococci | — | ||
| Clostridia | ≤105 | ≤103 | ≤105 |
| Candida | ≤104 | ≤103 | ≤104 |
It is imperative to take into account that the norms vary for children, infants and adults; in addition, you should not try to make a diagnosis yourself - only a doctor will be able to tell exactly how damaged the intestines are and what treatment is required to restore it.
How to pass a biochemical analysis: explanation
These techniques are also called biochemical stool analysis. Its essence lies in the following: all microorganisms produce a certain range of fatty acids during their life activity. Some of them are specific to only one type of microorganism, while others can be produced by all bacteria. By determining the spectrum of these fatty acids, we can assume which microorganisms predominate in the gastrointestinal tract and which part of it is affected.
The advantages of this express method are the speed of obtaining results (they are available in almost an hour), the determination of not only those microorganisms that are in the intestinal lumen, but also located near its walls (these microorganisms cannot always be obtained by examining the patient’s stool), the delay of the study material (stool examination can be carried out even one day after receiving the material).
Preparing for analysis
When taking a stool test, you should remember that its results may depend not only on what microorganisms have settled in the intestines, but also on the conditions under which the test was taken and its exposure to fresh air (you will find the rules for collecting stool samples here).
The analysis itself must be taken in clean, sterile containers. It is advisable to purchase a special container for taking tests at a pharmacy - the entry of bacteria from the environment into the container is almost completely eliminated.
The analysis itself should be taken with a sterile cotton swab. At least 7-8 smears are taken from different areas of the stool (for the most accurate study). Be sure to take a stool sample from the area where you can visually notice mucous contents or blood.
You cannot take stool for analysis after taking laxatives - defecation should be voluntary and not earlier than 12 hours after stopping antibiotics.
Immediately after taking the test, it should be delivered to the laboratory no later than 2 hours later. After this time has passed, the results of the analysis lose their reliability. In addition, it is imperative to avoid contact of the taken material with air, since the results obtained are distorted and aerobic flora, which is normally absent in the intestine, may be activated, which will further confuse the laboratory assistant.
Reasons for the increase and decrease in enterococci in feces, methods of treatment
Medicine
Enterococci are gram-positive microbes represented by 15 different species. There are non-pathogenic, beneficial species, and opportunistic ones. A large number of the latter can lead to the development of various diseases. Enterococci are round in shape. They cannot form capsules and spores around themselves.
There are several groups: in 80-90% of the bacteria are Enterococcus faecalis, in second place is Enterococcus faecium. There are other, less numerous species.
For the first time, our body encounters enterococci when they come to us along with mother's milk. Most of it remains in the small and large intestines.
The number of enterococci depends not only on the characteristics of the organism, but also on age. The older a person is, the greater the chance of an increased number of bacteria in the body.
Normal for 1 g. feces should contain no more than 100 million bacteria. If the quantitative characteristics are not higher than this mark, then:
- opportunistic microflora is effectively destroyed;
- rapid absorption and proper distribution of glucose throughout the body occurs;
- vitamins are synthesized;
- carbohydrates begin to be broken down and processed;
- immunity increases.
Some non-pathogenic types of microbes are used in the food industry to ferment milk, reducing the number of pathogenic microorganisms in food. Some varieties are also used in medicine. Based on them, drugs are made that can effectively combat dysbiosis and intestinal infections.
Danger
Exceeding normal levels of bacteria can lead to the development of disease. Disruption of the natural balance can lead to an increase in opportunistic microflora.
They become pathogenic when they appear in atypical habitats. This could be the kidneys, urinary tract and other organs. The danger is hidden behind a whole chain of serious diseases; it is important to ensure that the indicators are always normal.
Normal indicators
When studying feces, the following quantities are considered normal:
- for children under 1 year – 106 – 107.
- for children after 1 year – 107 – 108.
- for adults – 106 – 108.
Reasons for appearance
In children, the most common cause is taking medications, hypothermia, or damage to the integrity of the mucous membrane. Sometimes bacteria appear in stool when invasive diagnostic methods are used.
In adults, there are more reasons for the appearance of enterococci in the stool. This may be long-term use of antibiotics, hormonal imbalance in women. Sometimes there is a large number of bacteria in pregnant women as a result of constant surges in estrogen and androgens.
It is usually impossible to become infected with enterococci, since they are natural inhabitants of our body.
Their increase may be due to non-compliance with personal hygiene rules and a decrease in immune reactivity.
The latter is possible due to stress and the presence of various infectious pathologies.
Excessive consumption of alcoholic beverages and natural human aging are also provoking factors.
Enterococci in stool are increased
The bacteria can cause serious health problems. These include:
- Meningitis. Infectious disease of the lining of the spinal cord or brain.
- Diverticulitis. A painful process associated with the formation of various formations on the walls. Disturbs the processes of normal intestinal motility.
- Pathologies of the genitourinary system. If left untreated, chronic forms may appear that are difficult to treat and cause relapses.
- Endocarditis. Heart disease, which can be acute or chronic. Pathogenic microflora affects the inner lining of the atria, ventricle, and valve apparatus.
- Septic arthritis. It causes infection of the joints.
- Gastritis. Characterized by superficial inflammation of the stomach lining.
- Enteritis. A pathology that mainly affects healthy cells of the small intestine.
In infancy, an excessive increase in the number of bacteria can be assumed based on various symptoms. These include the release of foul-smelling feces, diarrhea, and bloating. The child may become whiny and refuse to eat.
In adults, signs of an increase in pathogenic microflora are not only symptoms characteristic of a particular disease, but also depression, weakness, and increased fatigue. In men, potency may suffer.
If they are demoted?
Sometimes the indicators are reduced. This may occur for physiological reasons. It has no diagnostic information. Sudden growth can trigger severe inflammatory reactions.
Diagnosis of diseases caused by bacteria
It is possible to identify the cause of a disease caused by an increased number of enterococci only using laboratory research methods.
In addition to stool analysis, urine tests and a smear may be required. The latter is used in most cases in women, since bacteria often cause vaginitis and other inflammations of the genital tract.
If enterococci appear in large numbers, then blood tests may be required to determine the inflammatory response. Other diagnostic methods are selected taking into account the specific course of the pathology.
Over the past 30 years, enterococci have become resistant to almost all known classes of antibiotics. Despite this, such drugs are among the main ones for the treatment of pathology.
To reduce the risk of developing resistance, combinations of different antimicrobial drugs are used. Additionally, culture is carried out to determine the degree of sensitivity of the enterococcus strain to a particular drug.
Most often, for mild pathologies, aminoglycosides are used. Additionally, immunomodulators may be prescribed. Helping restore the body's protective properties.
Beneficial enterococci allow you to cope with pathogenic microflora. Therefore, they are sold in the form of special products.
Probiotics are intended to treat dysbiosis and restore normal gastrointestinal microflora.
Popular and well-known means are Bifiform, Linex. To create such drugs, strains that were selected for the food industry are often used. Such strains are not designed to remain in the body for too long.
If the growth of enterococci is too large, liquid bacteriophage is used. It can be given to children in the first months of life. The bacteriophage can be drunk or used for an enema.
In conclusion, we note that maintaining the normal growth of microflora in the intestines is easy if you follow the correct diet and take walks in the fresh air.
Doctors remind that bad habits reduce the body's defenses. Therefore, it is recommended to abandon them and focus on regular sports and hardening. Particular attention is paid to infants. Their immunity is not yet fully formed, so you need to monitor their proper nutrition.
Tonsillitis is a disease accompanied by inflammatory processes in the palatine tonsils (tonsils) due to infectious infection. Most often, staphylococci and streptococci act as catalysts for sore throat.
Sore throat has two forms: purulent (acute) and chronic. The acute form is more dangerous, as it is characterized by a white coating on the pharyngeal ring. If treated incorrectly or not, angina can cause serious complications.
The Aptekin reference portal will help you compare prices for medications for sore throats in Kharkov pharmacies.
Complications of acute tonsillitis
Sore throat significantly weakens the immune system and can cause viruses to spread to other organs (for example, the kidneys or heart). The most likely consequences of untreated sore throat include:
- bronchitis;
- otitis;
- pneumonia;
- pyelonephritis;
- sinusitis;
- laryngitis;
- cholecystitis;
- blood poisoning;
- cervical phlegmon.
Among the most severe but rare complications is postanginal septicemia, which can be fatal.
Treatment methods
For acute tonsillitis, complex treatment is necessary. It consists of taking medications and physiotherapeutic procedures.
The last resort to prevent tonsillitis is surgery - tonsillectomy. According to experts, it is better to keep your organs clean than to remove them at the first opportunity.
Even traditional medicine methods are suitable for eliminating purulent sore throat, but only after consulting a doctor.
Conservative treatment methods include: local treatment and antibacterial therapy.
Local therapy includes the following:
- Lubricating the tonsils. For this purpose, special solutions (iodine or Lugol), local antibiotics, and anti-inflammatory drugs are used. This helps to destroy pathogenic microflora and relieve pain.
- Rinse and inhalation. The mechanical action of rinsing helps remove infection and cleanse the tonsils. Herbal decoctions have an anti-inflammatory effect, and inhalations with tube quartz kill germs.
- Local medications in the form of tablets or lozenges for the throat (Faringosept, Lizobakt).
Antibacterial therapy involves systemic treatment with antibiotics. For acute tonsillitis, the doctor may prescribe a broad-spectrum drug. However, after the test, the antibiotic is selected depending on the strain of the pathogenic bacterium. Their intake must be strictly followed by the doctor's recommendations.
The surgical method involves surgical intervention - removal of the tonsils, which is the point of no return. Indications for such an operation are purulent detritus or recurrence of sore throat more than 4 times a year.
To prevent the occurrence of acute tonsillitis, it is necessary to take preventive measures against throat diseases.
Source: https://svadba1000.ru/zdorove/meditsina/3916-prichiny-povysheniya-i-ponizheniya-enterokokkov-v-kale-sposoby-lecheniya.html
Analysis of stool for dysbacteriosis: hemotest, interpretation
An important indicator of the condition of the intestines (and in particular dysbiosis) is the presence of blood in the stool. As mentioned, with massive bleeding from the lower intestines, blood is visible to the naked eye. Moreover, if the bleeding is insignificant or its area is located quite high, in this case, a hemotest or stool test for occult blood should be performed at the same time.
Analysis for this study is carried out in the same way as for the general study. The main conditions are refusal to consume meat products 3 days before the test, prohibition of enemas and taking laxatives before the test.
The essence of the reaction lies in the determination of altered hemoglobin, and not red blood cells. Under the influence of digestive enzymes and bile, deformation and change in the structure of the hemoglobin molecule occurs. When benzidine is added to the analysis (this test is also called the benzidine test or Gregersen test), it is possible to detect the presence of altered hemoglobin, and in this case the test is considered positive. This condition can be observed with intestinal ulcers, tuberculosis, and helminthiasis.
You should not rely on negative test results, as they do not always have informational value. If there is no result, it is imperative to repeat the test to confirm the condition.
A false positive reaction during this study can be observed as a result of eating meat products or certain medications.
Let's sum it up
Intestinal dysbiosis is a rather serious condition. This condition is especially dangerous in children, who need vitamins and simple substances (amino acids, monosaccharides) more than adults, the excretion of which increases with dysbacteriosis.
Dysbacteriosis is the main complication of long-term use of antibiotics. In such a situation, it is necessary to take a stool test. In this case, the patient is directly indicated for the use of probiotics in order to repopulate the intestines with bacteria and restore normal digestion.
When not to get tested
It is not recommended to be tested for dysbacteriosis when taking the following medications:
- antibiotics;
- anti-inflammatory non-steroidal drugs;
- other groups of antibacterial drugs;
- vitamins;
- drugs that reduce gas formation in the intestines (Plantex, Espumisan);
- enterosorbents (Smecta, Enterosgel);
- laxatives.
The study should not be performed if the patient is receiving rectal suppositories or enemas.