Peptic ulcer of the stomach and duodenum is a chronic disease characterized by the formation of ulcers in the stomach and duodenum. Peptic ulcer disease is characterized by seasonal exacerbations (spring and autumn).
According to statistics, every 10 resident of Russia suffers from this disease, and men predominate among patients (80%).
Peptic ulcer disease is dangerous due to its complications, which pose a serious threat to health. Thus, gastrointestinal bleeding often occurs, perforation of the stomach wall and penetration of the ulcer into neighboring organs, malignancy of the ulcer with the development of stomach cancer.
Peptic ulcer of the stomach and duodenum: causes.
2. An imbalance between the production of substances that aggressively affect the wall of the stomach and duodenum and protective factors.
Factors of aggression include hydrochloric acid and pepsin produced in the stomach, as well as pancreatic enzymes, bile acids, lysolecithin, which enter the lumen of the duodenum from the pancreas and liver.
The protective factors in this case are the production of mucus by the cells of the stomach, which envelops the mucous membrane, preventing direct contact of hydrochloric acid and enzymes with epithelial cells, timely renewal of the epithelium of the stomach and duodenum and its full blood supply. The production of bicarbonates in the stomach (its antrum) and duodenum and the complete closure of the pyloric sphincter ensures the protection of the duodenum from the acidic contents of the stomach.
An imbalance of aggressive and protective factors can occur under the influence of psycho-emotional stress, as a result of alcohol abuse, unhealthy diet, uncontrolled use of certain medications (aspirin and other non-steroidal anti-inflammatory drugs, glucocorticosteroid hormones (prednisolone, dexamethasone, metipred), cytostatics (methotrexate, etc.) and others).
Improper nutrition means eating too cold or hot, spicy, fried, smoked food, dry food, and drinking coffee.
Symptoms of peptic ulcer of the stomach and duodenum.
Gastric ulcer: clinical picture. Symptoms of a stomach ulcer.
In more than half of patients, an ulcer forms in the body of the stomach along its lesser curvature, so pain, which is the most common symptom of an ulcer, occurs in the majority of patients in the epigastric region, often slightly to the left of the midline of the abdomen. With this localization of the ulcer, pain occurs 60-90 minutes after eating, moderate, aching.
When an ulcer is localized in the upper part of the stomach, inflammation is often transmitted to the sphincter (sphincter), which separates the stomach cavity from the esophagus. As a result, sphincter insufficiency occurs, and the contents rise during peristalsis of the stomach through the esophagus, causing nausea and even vomiting. Pain with this location of the ulcer occurs half an hour after eating, is often localized behind the sternum and can radiate to the heart, to the left arm or shoulder blade, simulating an attack of angina. A distinctive feature of the pain syndrome in peptic ulcer disease is the connection between the occurrence of pain and food intake and the lack of connection with physical activity.
With an ulcer located in the pyloric region, pain occurs in the epigastric region on an “empty stomach” and at night. “Hungry” and “night” pains are classic symptoms of gastric ulcers, and almost never occur with gastritis. The intensity of pain is usually pronounced. The pain can occur in attacks repeatedly during the day. Often, patients do not find any connection between a painful attack and food intake.
In addition to pain, patients may be bothered by sour belching, heartburn, nausea, vomiting, excessive salivation, and a feeling of fullness in the stomach after eating a small portion of food. It is not uncommon for patients with ulcers to lose weight.
Duodenal ulcer: symptoms. Clinical picture of duodenal ulcer.
With a duodenal ulcer, pain occurs 1.5-4 hours after eating and is more often found in the right half of the abdomen, in its upper part. The pain is usually intense, paroxysmal, and can radiate to the right side of the chest. Eating brings relief: the pain subsides within 5-20 minutes after eating.
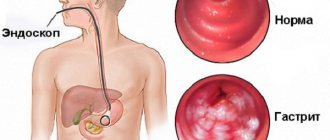
A little about gastritis
Gastritis is an inflammatory process of the gastric mucosa with impaired absorption of food.
There are chronic and acute forms of the disease.
In the acute form, functions are impaired for a short time. This happens due to the influence of external aggressors when they enter the digestive system (poisoning with poisons, chemicals, very hot or cold food, etc.). Microorganisms can also become pathogens. The first symptoms appear 6-12 hours after exposure to aggressors. Possible death.
In the chronic form, the function of the glands of the organ mucosa is impaired. Also, over time, the regeneration of healthy cells stops and atypical ones begin to predominate, which is how a stomach ulcer appears. With this form of the disease, ailments appear: nausea and vomiting, pain, bloating, bowel dysfunction, heartburn, belching and bad breath. There is a phase of exacerbation and calm.
Both adults and children are susceptible to this disease.
Treatment of peptic ulcer of the stomach and duodenum.
Approaches to the treatment of gastric ulcers, duodenal ulcers and those caused by Helicobacter are the same: treatment is carried out with antibiotics, enveloping (gastroprotective) and hydrochloric acid neutralizing drugs for a course of 10-14 days.
At the end of treatment, a control endoscopic examination of the stomach and duodenum is performed. If the ulcerative defect persists, proton pump inhibitors or bismuth preparations (De-nol) are added to treatment for the next 2-3 weeks. 1-1.5 months after the end of treatment, a repeat endoscopic examination of the stomach and duodenum is required, during which the effectiveness of treatment is assessed: whether the ulcer has healed and whether Helicobacter pylori has been destroyed.
If cure does not occur, treatment is carried out with second-line drugs.
IMPORTANT!
It is imperative to complete the course of treatment in full and strictly follow the doctor’s instructions. Otherwise, the effectiveness of treatment sharply decreases, and bacteria (Helicobacter), if they are not completely destroyed, very quickly become resistant to the antibiotics used during therapy.
It has been proven that most failures in the treatment of peptic ulcers are caused by the patient’s unscrupulous compliance with medical instructions.
It is important for the doctor to remember that if the patient has ever taken nitrofurantoin drugs (metronidazole, tinidazole, etc.) to treat any disease, they should not use treatment regimens in which they are used, since Helicobacter is already immune to their action.
Correctly administered treatment can lead to a complete cure of the patient. But even if there is no cure, long-term remission is achieved in 2/3 of patients, the frequency of exacerbations and the risk of complications of peptic ulcer disease, such as gastrointestinal bleeding, perforation and penetration of the ulcer, are sharply reduced.
Treatment methods using medication
Doctors prescribe treatment regimens for gastric and duodenal ulcers that have been proven over the years, all of which include taking antibacterial drugs.
Scheme 1
Used when a patient is infected with H. pylori. Therapy includes a proton pump inhibitor (omeprazole, omez) and antibacterial drugs - Clarithromycin and Amoxicillin (if you are allergic to the penicillin series, Amoxicillin is replaced with Metronidazole.). The drugs are used according to the instructions. Amoxicillin is usually prescribed in a dose of 1 g 2 times a day. This regimen is used for long-term gastritis and peptic ulcers, but without serious complications. The minimum course of treatment is 7 days.
Scheme 2
Prescribed in the absence of positive dynamics during treatment with a three-component regimen. A proton pump inhibitor, an antacid - bismuth citrate (Vis-Nol, De-Nol), an antimicrobial, antiprotozoal drug Metronidazole and usually an antibacterial agent of the tetracycline group are prescribed. The course of treatment is at least 7 days.
Scheme 3
One of the following combinations of drugs may be used::
- proton pump inhibitor and high doses of Amoxicillin - 10-14 days.
- proton pump inhibitor, Amoxicillin and Levofloxacin - 7-10 days.
- proton pump inhibitor, tetracycline, bismuth preparation, furazolidone - 7 days.
If a peptic ulcer is not associated with H. pylori, then lighter treatment regimens are prescribed - bismuth preparations, proton pump inhibitors, antacids, sorbents, phytotherapeutic drugs, diet. In this case, it is possible to achieve scarring of the ulcer without the use of antibacterial drugs.
For children, a treatment regimen should be selected by a pediatrician together with a gastroenterologist. Adults are also required to consult a gastroenterologist; as a rule, such pathological conditions should be observed by a gastroenterologist or local doctor, but always together with a specialized specialist. At the end of therapy, it is imperative to undergo repeated diagnostic procedures in order to ensure the effectiveness of the treatment. In such cases, fibrogastroduodenoscopy is informative, and in case of infection with H. pylori, special tests to detect the bacterial agent.
Treatment of gastric and duodenal ulcers caused by Helicobacter pylori.
Three-component scheme
Treatment is carried out for 10-14 days simultaneously with three drugs:
- Proton pump inhibitors (Omeprazole 20 mg 1-2 times a day, rabeprazole (Pariet) 20 mg 1 time a day, pantoprazole (Nolpaza) 40 mg 2 times a day, lansoprozole 30 mg 2 times a day, esomeprazole 20 mg 2 slot per day);
Four-component scheme
Treatment is also carried out for 10-14 days.
- Amoxicillin (Flemoxin Solutab®) 500 mg 4 times a day, or 1000 mg twice a day;
- Clarithromycin (Klacid) 500 mg twice a day, or josamycin (Vilprafen®) 1000 mg twice a day, or nifuratel (MacMirror) 400 mg twice a day;
- Proton pump inhibitors (Omeprazole 20 mg 1-2 times a day, rabeprazole (Pariet) 20 mg 1 time a day, pantoprazole (Nolpaza) 40 mg 2 times a day);
A three-component regimen for the treatment of patients with chronic gastritis and gastric ulcer, if the patient has atrophy of the gastric mucosa with a decrease in acid-forming function (low acidity)
The course of treatment is 10-14 days.
- Amoxicillin (Flemoxin Solutab®) 500 mg 4 times a day, or 1000 mg twice a day;
- Clarithromycin (Klacid) 500 mg twice a day, or josamycin (Vilprafen®) 1000 mg twice a day, or nifuratel (MacMirror) 400 mg twice a day;
- Bismuth tripotassium dicitrate (De-Nol®, Ventrisol) 120 mg 4 times a day, or 240 mg twice a day.
In 20% of patients with gastric ulcer, Helicobacter pylori is not detected. To treat such patients, regimens without an antibacterial component are used, which are prescribed in a course of 14-21 days. For example:
1. Drugs that suppress the secretion of hydrochloric acid:
Proton pump inhibitors:
- Omeprazole (Omez) 30 mg 1 - 2 times a day, or pantoprazole 40 mg 1 - 2 times a day, or esomeprazole 20 - 40 mg 1 - 2 times a day, or rabeprazole 20 mg 1 - 2 times a day.
or H2-histamine receptor blockers:
- Famotidine 20 mg twice a day for 2-3 weeks.
2. Gastroprotectors:
- Tripotassium bismuth dicitrate (De-nol, Ventrisol) 120 mg 4 times a day 30 minutes before meals;
- Sucralfate (Venter, Alsukral) 500-1000 mg 4 times a day 30-60 minutes before meals for 14-28 days.
Upon completion of the course of treatment, patients with peptic ulcer disease are often (especially with a history of complicated ulcers and gastric ulcers) prescribed drugs that reduce the secretion of hydrochloric acid for daily use. In such cases, as a rule, the drug is used in a minimum dosage once a day.
If complications of a peptic ulcer occur, such as bleeding from an ulcer with massive blood loss, perforation of an ulcer or degeneration of an ulcer into stomach cancer, impaired evacuation of food from the stomach as a result of narrowing of the outlet (pyloric) section of the stomach, and for a number of other indications, the patient may be offered surgical treatment.
“Second-line” regimens for the treatment of gastric and duodenal ulcers.
These regimens are also prescribed in a course of 10-14 days.
Four-component “second line” scheme with nitrofurans
1. Proton pump inhibitors; 2. Amoxicycline (500 mg 4 times a day or 1000 mg 2 times a day); 3. Nitrofuran drug: nifuratel (400 mg 2 times a day) or furazolidone (100 mg 4 times a day) 4. Tripotassium bismuth dicitrate (120 mg 4 times a day or 240 mg 2 times a day).
Quadruple second-line regimen with rifamixin
1. Proton pump inhibitor. 2. Amoxicillin (500 mg 4 times a day or 1000 mg 2 times a day). 3. Rifaximin (Alfa Normix) 400 mg 2 times a day. 4. Bismuth tripotassium dicitrate (120 mg 4 times a day) for 14 days.
For stomach and duodenal ulcers, the doctor prescribes antibiotics to suppress the Helicobacter bacteria. Antibacterial drugs are included in the complex treatment of peptic ulcer disease, but only if the disease is of bacterial origin. Antibiotics are not the safest medicines; they come in natural and semi-synthetic origins; when they enter the body, they specifically inhibit the development of living cells. In this case, the target of antibiotics is the bacterium Helicobacter pylori, located in the layers of the gastric mucosa.
The drug contains Clarithromycin, Tinidazole, Omeprazole. Omeprazole blocks the formation of acid in the damaged organ, Clarithromycin acts on the Helicobacter bacteria, and Tinidazole destroys anaerobic bacteria. The packaging of the drug is designed for 1 course of treatment. One blister contains one capsule and two tablets, which must be taken at a certain time.
Effective drugs for treating stomach ulcers
Antibiotic therapy is the basis for the treatment of stomach ulcers, since the disease is bacterial in nature. Each modern antibiotic is effective against certain groups of microorganisms.
Therefore, treatment of ulcers should be based on a comprehensive examination, the results of which will determine the optimal course of therapy. Next, therapy is carried out with various drugs that are prescribed for stomach ulcers.
Advice! In addition to a narrowly targeted group of drugs, patients with ulcers are prescribed vitamin complexes that improve the general condition of the body.
What antibacterial drugs are effective in treating peptic ulcers? Let's look at the most effective antibiotics for stomach and duodenal ulcers.
Clarithromycin
This antibiotic is often used in the treatment of ulcers and has the following advantages:

- has high resistance to hydrochloric acid;
- characterized by a long duration of action;
- quickly absorbed.
Currently, Clarithromycin is the main antibiotic used to treat stomach ulcers.
Amoxicillin
The drug belongs to the group of penicillins and has the following advantages:
- long period of elimination from the body;
- resistance to gastric enzymes;
- absorption is more than 90%.

Due to such high characteristics, the drug is often used for gastric ulcers.
Metronidazole
A classic antibiotic that has proven effectiveness over many years of use. A special feature of the drug is its direct effect on the DNA of pathogenic microflora. Therefore, the course of treatment lasts relatively short. The drug acts as a synthetic antibiotic and has the following advantages:
- has a wide spectrum of action;
- promotes the death of not only Helicobacter pylori infection, but also those microorganisms that cause dysbacteriosis;
- penetrates directly into the DNA of the bacterium, destroying it and causing the inevitable death of the microbe.

Tetracycline
This antibiotic has a wide spectrum of action and is therefore used to treat a number of diseases. A special feature of the drug is its influence on the process of protein synthesis of cells, resulting in the death of pathogenic microflora.
The effectiveness of Tetracycline also applies to Helicobacter pylori, and therefore the drug is often used to eliminate the symptoms of peptic ulcer disease. Features of Tetracycline:
- does not show effectiveness at high acidity;
- directly affects the process of bacterial reproduction, contributing to a gradual decrease in their number in the body.
McMiror and Klacid SR
Antibiotic Klacid SR is the most preferable for complex intestines. Klacid SR gives stable and quick results in a short antibacterial course. It is highly active against the main causative agent of gastric and duodenal ulcers - Helicobacter bacteria. Klacid SR is well tolerated by patients and is absorbed into the stomach regardless of food intake. The drug is resistant to acidic environments, safe and easy to use. The antibiotic Klacid SR is recommended for patients with gastric and duodenal ulcers by leading European and Russian gastroenterologists.
The antibiotic is produced in film-coated tablets. One tablet of Klacid SR contains 0.25 g of Clarithromycin. It can also be used for intravenous injection; it is available in bottles for preparing a solution.
The drug Macmiror, unlike Klacid SR, contains the active substance nifuratel. The drug has a pronounced antifungal, antibacterial, antiprotozoal effect. It inhibits the Helicobacter bacterium, which is why it is successfully used to treat peptic ulcers. It is allowed to be prescribed to children in case of inflammatory diseases of the stomach and duodenum. A good therapeutic effect is achieved due to the high efficiency and good tolerability of the drug.
Antibiotics Macmiror and Klacid SR are popular in gastroenterology due to the short treatment period and the possibility of being prescribed to children after 12 years of age.
Metronidazole for peptic ulcers
Standard regimens for the treatment of gastric and duodenal ulcers with Metronidazole involve oral administration of tablets. In severe cases of the disease, intravenous administration of the drug is also possible.
Treatment is carried out for two weeks. Regardless of taking other medications, it is usually recommended to take 2 tablets of Metronidazole 500 mg three times a day. At this dosage, the medicine penetrates well into the foci of inflammation and has optimal therapeutic activity. If necessary, treatment with Metronidazole is repeated after a week's break.
However, Metronidazole cannot be prescribed independently for stomach ulcers . Therapeutic therapy, as well as the calculation of dosages of medications, can only be carried out by a specialist. Otherwise, when self-medicating gastritis and ulcers, the patient’s condition may worsen (vomiting, internal bleeding and acute pain).
Hiconcil and Binoclar
The antibiotic Hiconcil has the active ingredient Amoxicillin and has a pronounced antibacterial effect. The drug can be prescribed to children and adults, as well as during pregnancy. The purpose of prescribing an antibiotic is to completely destroy the Helicobacter bacteria. This is a modern option for the treatment of peptic ulcers, which has already shown its high effectiveness. The drug is available in the form of capsules and powder for preparing a solution or drops. One capsule contains 0.25 or 0.5 g of amoxicillin.
The drug Binoclair is indicated for bacterial infections of the stomach and duodenum. Contains Clarithromycin, available in granules for suspension, capsules and powder. Indicated for children over 12 years of age and adults, the average course of treatment is from 6 to 15 days. These are macrolide antibiotics with a wide spectrum of activity, affecting, among other things, the Helicobacter bacterium.
Antibacterial therapy for peptic ulcer disease includes the prescription of several drugs to enhance the effect.
Ceftriaxone for stomach ulcers
The drug is administered intramuscularly or intravenously.
Adults and children over 12 years of age
Prescribe 1-2 g 1 time/day (every 24 hours). In severe cases or for infections whose pathogens are only moderately sensitive to ceftriaxone, the daily dose can be increased to 4 g.
Newborns (up to 2 weeks)
Prescribe 20-50 mg/kg body weight 1 time/day. The daily dose should not exceed 50 mg/kg body weight. When determining the dose, no distinction should be made between full-term and premature infants.
Infants and young children (from 15 days to 12 years)
Prescribe 20-80 mg/kg body weight 1 time/day.
Children weighing >50 kg
Prescribe doses intended for adults.
Doses of 50 mg/kg or more for intravenous administration should be administered by drip over at least 30 minutes.
Elderly patients should be given
usual doses intended for adults, without adjustment for age.
The duration of treatment depends on the course of the disease. The administration of Ceftriaxone should be continued in patients for at least 48-72 hours after the temperature has normalized and eradication of the pathogen has been confirmed.
For bacterial meningitis
in infants and young children,
treatment begins with a dose of 100 mg/kg (but not more than 4 g) 1 time/day. Once the pathogen has been identified and its sensitivity determined, the dose can be reduced accordingly.
For meningococcal meningitis
the best results were achieved with a treatment duration of 4 days, for meningitis caused by
Haemophilus influenzae -
6 days,
Streptococcus pneumoniae -
7 days.
For Lyme borreliosis:
adults and children over 12 years of age
are prescribed 50 mg/kg 1 time per day for 14 days; the maximum daily dose is 2 g.
For gonorrhea (caused by strains that form and do not form penicillinase) -
once intramuscularly at a dose of 250 mg.
To prevent postoperative infections
depending on the degree of infectious risk, the drug is administered in a dose of 1-2 g once 30-90 minutes before the start of surgery.
During operations on the colon and rectum
- simultaneous (but separate) administration of Ceftriaxone and one of the 5-nitroimidazoles, for example, ornidazole, is effective.
In patients with
impaired renal function
, there is no need to reduce the dose if
liver function remains normal
.
In cases of preterminal renal failure with CC<10 ml/min,
the daily dose of the drug should not exceed 2 g.
In patients with impaired liver function
there is no need to reduce the dose if
renal function remains normal
.
With a combination of severe renal and liver failure
The plasma concentration of ceftriaxone should be regularly determined and its dose adjusted if necessary.
Patients on
dialysis
do not require additional administration of the drug after dialysis. However, the serum concentration of ceftriaxone should be monitored for timely dose adjustment, since the rate of elimination of the drug in these patients may be reduced.
Rules for the preparation and administration of solutions
For intramuscular administration
The contents of the bottle (1 g) are dissolved in 3.6 ml of water for injection. After preparation, 1 ml of solution contains about 250 mg of ceftriaxone. If necessary, a more diluted solution can be used.
As with other IM injections, Ceftriaxone is injected into a relatively large muscle (gluteus); Test aspiration helps avoid inadvertent injection into a blood vessel. It is recommended to inject no more than 1 g of the drug into one muscle. To reduce pain during intramuscular injections, the drug should be administered with a 1% lidocaine solution. Do not administer lidocaine solution intravenously.
For intravenous administration
The contents of the bottle (1 g) are dissolved in 9.6 ml of water for injection. After preparation, 1 ml of solution contains about 100 mg of ceftriaxone. The solution is administered slowly over 2-4 minutes.
For IV infusion
Dissolve 2 g of Ceftriaxone in 40 ml of sterile water for injection or one of the infusion solutions that do not contain calcium (0.9% sodium chloride solution, 2.5%, 5% or 10% dextrose solution, 5% levulose solution, 6% dextran solution in dextrose) . The solution is administered over 30 minutes.
Disadvantages of antibacterial drugs
The main disadvantage of antibacterial drugs is the high risk of adverse reactions. With long-term use of antibiotics, changes in the central nervous system can be observed. Dizziness, hallucinations, confusion, apathy, depression, and convulsions may occur. Such consequences, of course, are not expected by everyone, since drugs are prescribed strictly according to indications and possible risks are always taken into account. Serious adverse reactions are an absolute contraindication to the use of antibiotics without a doctor's prescription.
Possible side effects:
- disorders of the gastrointestinal tract - diarrhea, dysbacteriosis, pain;
- difficulty urinating, temporary urinary incontinence;
- disruption of the kidneys and liver.
All antibacterial drugs, including the relatively safe Klacid SR, can, under certain conditions, lead to unpleasant consequences. The mildest adverse reactions include headache and dizziness. The consequences also include unreasonable fear, anxiety, insomnia and nightmares. In some cases, the body reacts with disorientation, psychosis, and depersonalization, but this happens extremely rarely. More often, complications such as vomiting, nausea, dental diseases, frequent urination, and tinnitus can be observed. From the circulatory system there is a risk of bleeding and thrombocytopenia. Even more often, allergic reactions may occur, which is manifested by skin itching, rash, and redness.
Treatment with antibiotics for liver disease should be constantly monitored, as with pathologies of the cardiovascular system.
Taking antibiotics without a doctor's prescription can lead to dyspeptic symptoms, dysbiosis and kidney failure. Without the help of a specialist, it is difficult to predict how self-medication will turn out, and if one person’s ulcer symptoms subside after a few days, another may end up in the intensive care unit.
It is important to know
Antibiotics for stomach and duodenal ulcers are necessarily included in the drug treatment regimen. But therapy that can save a person from developing pathological defects in these parts of the gastrointestinal tract should only be carried out in combination. A unilateral approach, without the use of preventive measures, will be ineffective.
In order to forget about the disease, antibacterial agents alone, although they are considered basic, are not enough. In order to speed up the recovery process, specialists in the treatment of patients with peptic ulcer and duodenal ulcer use various groups of drugs in combination. They are selected depending on what caused the disease and at what stage of development it is.
Features of the treatment of ulcerative lesions of the gastrointestinal tract
Ulcer treatment will not be effective if a specialist does not draw up a competent medication treatment regimen. It is necessarily formed with the use of antibiotics. These drugs are prescribed to suppress the development and growth of Helicobacter pylori, which is the main bacterium and duodenum.
After a suitable antibacterial agent has been selected, technical rules of therapy and additional drugs that will increase the effectiveness of treatment are selected. For each specific patient, it is selected individually, depending on the clinic of the disease.
If pathological defective changes in the mucous membrane of the duodenum or stomach have reached the stage of exacerbation, dynamic principles are used when providing care to patients. In this case, enhanced treatment is applied, distributed over 10 days. During this entire time, the patient is prescribed a strict diet and bed rest.
After all the manipulations undertaken have been successful, preventive therapy is prescribed. It includes both medications and folk remedies. The list of medications prescribed during this period is focused on the causes of the pathology:
- Antibacterial drugs that inhibit the development and growth of pathogenic microorganisms.
- Antiulcer agents with a high content of bismuth.
- Antisecretory drugs that normalize the acidic environment.
The primary task of the attending physician before prescribing medications is to assess the general physiological condition of the patient. This is necessary in order to draw up an adequate treatment plan, since intensive antibiotic therapy for a weakened body can result in the development of severe complications.
Basic principles of drug therapy
In medical practice, the treatment regimen for stomach ulcers with antibiotics is the main method aimed at combating a specific pathogenic microorganism. Only a specialist decides whether a particular patient can take a certain antibacterial drug and in combination with which medications it can be introduced into the course of treatment. Medicines are selected to suppress irritating factors and destroy pathogenic bacteria. The following groups of drugs are usually prescribed:
- Antibiotics (Metronidazole, Moxicillin, Mlarithromycin) intended to destroy pathogenic microorganisms.
- Bismuth preparations necessary to suppress the excessive activity of pepsin and hydrochloric acid (Bismuth Subnitrate, De-Nol and Vikalin).
- Proton pump inhibitors, PPIs, whose action is aimed at correcting the release of digestive enzymes (Lanzoprazole, Omeprazole).
The stronger the antibiotic prescribed to the patient, the sooner the desired result can be achieved.
Due to the fact that the abuse of antibacterial drugs poses a threat of complications and serious side effects, the main task of the doctor becomes an adequate assessment of the general physiological condition of the patient, so as not to harm his health with overly intensive therapy.
Treatment regimen for ulcers with antibiotics
In the treatment of gastritis and ulcers, a treatment regimen can be prescribed, consisting of several two stages:
- Treatment of gastritis and stomach ulcers with Metronidazole and Clarithromycin in combination with inhibitors. This therapy is used to suppress the vital activity of Helicobacter pylori in the patient’s body. In this case, the dosage of Metronidazole for stomach ulcers in the fight against Helicobacter pylori infection is calculated taking into account the individual characteristics of the clinical picture of the disease. If adverse reactions to basic medications occur, doctors can prescribe their analogues;
- Based on the results of the interim examination, the course of treatment with Metronidazole for duodenal ulcers or gastritis can be continued. However, instead of Clarithromycin, antibiotics of the tetracycline group should be taken at the second stage of therapy. The result of treatment should be the complete absence of pathogenic microorganisms in the human digestive system.

Antibacterial drugs used in the treatment of Helicobacter pylori infection complement each other. Bismuth, Omeprazole and the antihistamine Ranitadine are prescribed together with antibiotics. To obtain the expected therapeutic effect, antispasmodics, painkillers and healing drugs can be additionally prescribed. Traditional medicine may be recommended as additional therapy.
Basic criteria for choosing a course and regimen of therapy
At the very beginning, experts prefer to prescribe the simplest scheme. If the drugs are well tolerated, the patient is recommended to start taking more serious pills. Almost always, a quick result is achieved when a sick person starts taking 3 drugs at the same time - a combination of two antibiotics, for example, Amoxicillin and Clarithromycin with Omeprazole.
But only the doctor decides which antibiotics to take. Despite the fact that there is a list of potent medications that help cope with pathologies such as stomach ulcers, self-medication is strictly prohibited. Most often, after gastric ulceration is diagnosed, treatment is carried out according to the following scheme, the course of which lasts a week:
- De-Nol 120 mg/4 times a day.
- Metronidazole 200 mg/4 times or 400 mg/2 times.
- Amoxicillin 500/4 rub.
- Tinidazole 500/2 r.
- Clarithromycin 2500/2 r.
- Omeprazole 20 mg/1 time.
Although these drugs, based on reviews from specialists and patients, have proven themselves to be the best, it is strictly not recommended to use them without a doctor’s prescription. If you self-medicate with them, the disease of the gastrointestinal tract will not be cured, but will only become chronic, which will have to be treated for more than one year.
Therapeutic course for this disease in the presence of helicobacter pylori
In the event that ulcerative pathology of the duodenum or stomach is caused by Helicobacter pylori, antibiotic treatment is most often used. They are the ones who have a depressing effect on this bacterium, stopping its vital activity in a short time. For peptic ulcers that develop due to this pathogenic microorganism, it is possible to use 2 therapeutic regimens:
- Tritherapy, which consists of taking 3 medications at the same time. Typically, specialists using this regimen prescribe an antisecretory agent, most often using Omeprazole, and 2 antibiotics - Amoxicillin and Clarithromycin.
- Quad therapy, that is, it is necessary to use four drugs simultaneously. Among them are 2 antibiotics in tablet form (Tetracycline and Metronidazole), as well as De-Nol, a drug containing Bismuth, and Omeprazole, which normalizes the production of hydrochloric acid.
In some cases, doctors may prescribe a third, combined regimen. It includes drugs from the first and second groups of therapy, but other effective drugs are added to them based on the patient’s indications. The duration of this course is approximately 10 days.
It is important to remember that for ulcers, antibiotics should only be taken as prescribed by a doctor. Self-medication with them always leads to the most undesirable consequences.
Recently, specialists have increasingly used the treatment of Helicobacter pylori infection, which provokes the development of ulcerations in the stomach and duodenum, with De-Nol. This active drug contains bismuth and also acts as an antiseptic and bactericidal agent. It has a multifaceted protective effect, but is not an antibiotic, so it does not provoke the development of side effects.
The effect of the drug is that it actively destroys the membrane of the bacterium, which leads to its rapid death. The advantage of this drug is that helicobacter pylori resistance never develops to it.
Thanks to the use of multicomponent treatment regimens using antibacterial and other medications, ridding a person of ulcerated defects developing on the mucous membrane of his digestive organs has become much more effective. The use of antibiotics for therapeutic purposes significantly reduces the risk of relapse of the disease after a therapeutic course aimed at eliminating the causative agents of the ulcer.