Classification of the disease
The disease is classified according to the reasons for its manifestation:
- Bacterial. There is a specific type caused by various intestinal infections (shigellosis, salmonellosis, dysentery). And nonspecific - manifesting itself after the infection is destroyed.
- Parasitic. Occurs after various parasites appear in the intestines.
- Mechanical. As a consequence of prolonged constipation.
- Toxic. It appears after damage to the mucous membrane by toxins - chemicals, poisons, drugs.
- Secondary. Develops as a result of complications of other diseases of the digestive organs.
- Nutritional. Caused by prolonged poor nutrition.
What types of enterocolitis are there?
With enterocolitis, two forms of the disease are recorded - chronic and acute. The latter, despite the more pronounced symptoms of pain, indicates only superficial damage to the mucous layer in the intestine, which can be successfully treated. Chronic enterocolitis corresponds to deep penetration of the inflammatory process into the intestinal wall, which requires long and methodical therapy.
Another classification is based on the reasons that caused the inflammation. In this case, the following enterocolitis is distinguished:
- Infectious , caused by various types of pathological microenvironments, for example, salmonella, shigella, E. coli and others. The disease also appears in children against the background of rotaviruses and enteroviruses. Infectious cause is the most common factor resulting in acute enterocolitis.
- Parasitic appears with the development of helminthiasis and other lesions by protozoan microorganisms,
- The nutritional type is a consequence of poor nutrition, with the abuse of spicy and fatty foods. Another reason is frequent drinking of alcohol.
- Toxic enterocolitis is caused by the action of chemicals introduced into the body. It occurs due to drug overdoses.
- The mechanical type of the disease is formed with frequent constipation, when solid masses of feces deform the intestines from the inside.
- Autoimmune and allergic colitis appears as the ulcerative form of the disease progresses.
- Stress leads to disturbances in the supply of blood to the intestinal wall, leading to inflammatory phenomena in it.
Above we discussed primary enterocolitis, but there is also a secondary type, when inflammation in the intestines occurs due to other diseases of the gastrointestinal tract. In this case, suppressing the symptoms of enterocolitis without treating the underlying disease is pointless.
The main causes of pathology
The main and most common causes of enterocolitis, as described above, include acute intestinal infectious diseases: viral diarrhea, salmonellosis, typhoid fever, dysentery.
The disease also develops against the background of prolonged poor nutrition, various allergic reactions caused by prolonged use of antibiotics and some other medications.
Cases have been recorded in which enterocolitis occurred due to congenital chronic diseases: metabolic disorders, stomach diseases, problems with the immune system, dysbacteriosis and deficiency of vitamins in the body.
Enterocolitis begins to develop after an infection damages the tissue cells of the intestines, leading to their depletion.
If the intestinal flora begins to break down, chronic enterocolitis develops. As it leaks, it weakens the protective function of the intestinal mucosa, which makes it even more vulnerable to various bacteria. This is how enterocolitis usually occurs in adults; we will consider the symptoms and treatment further.
Enterocolitis: classification, symptoms and treatment methods
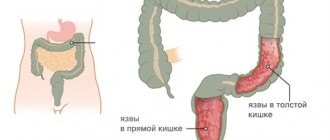
Enterocolitis is a disease that is characterized by the occurrence of inflammatory processes in the wall of the large and small intestines. Patients need to be aware of the possible symptoms of the pathology in order to see a doctor in time.
By etiology
Depending on the cause of its occurrence, enterocolitis is classified into:
- Infectious enterocolitis is caused by the proliferation of pathogenic microorganisms in the intestinal wall that adversely affect the condition of the organ.
- Non-infectious enterocolitis is associated with other factors that have a traumatic effect. They are divided into the following types: parasitic;
- nutritional;
- toxic;
- mechanical.
With the flow
- Spicy. An acute disease is characterized by a sudden onset of symptoms and their rapid development. The pathology progresses very rapidly and is often complicated by other diseases.
- Chronic. Chronic enterocolitis usually develops after acute. The disease is characterized by a specific course, during which periods of exacerbations and remissions alternate. Exacerbations are usually less pronounced than during an acute process, and they are less likely to lead to complications.
Intestinal manifestations
- severe pain in the lower abdomen;
- increased discomfort when pressing on the abdomen;
- bloating, flatulence;
- vomiting or nausea;
- diarrhea (diarrhea);
- change in stool character - the appearance of mucus or blood in the stool;
- loss of appetite, often – refusal to eat.
Extraintestinal manifestations
- increased fatigue;
- malfunction;
- increased body temperature, especially in acute enterocolitis;
- weight loss, exhaustion of the body;
- apathy or increased irritability;
- general weakness;
- headache;
- drowsiness;
- decreased attention and concentration;
- pain in muscles and joints;
- coated tongue.
Specific manifestations of different forms of enterocolitis
| Form of pathology | Specific symptoms |
| Ulcerative enterocolitis |
|
| Spastic enterocolitis |
|
Causes and risk factors
- Bacterial invasion. When pathogenic microorganisms penetrate the patient's body, an inflammatory process develops in the intestinal wall, which underlies the infectious form of enterocolitis. The disease can be caused by nonspecific microflora - E. coli, Proteus, etc. Less commonly, pathology occurs due to infection with bacteria of dysentery, salmonellosis or shigellosis.
- Parasitic diseases. Inflammation of the intestinal wall can be caused by pathogenic helminths, which are especially common in children. These include roundworms, pinworms, tapeworms, bovine and pork tapeworms, and liver fluke. Penetrating into the intestines, the worms attach to the mucous membrane and irritate it with their suckers. Because of this, the patient develops enterocolitis.
- Toxic effects. When harmful substances enter the digestive system, the intestinal mucosa is damaged, which leads to reactive inflammation. Not only poisons, but also some household chemicals and medications have a toxic effect on the gastrointestinal tract.
- Nutritional effects on the intestines. Rough food consumed by the patient in large quantities causes irritation in the wall of the digestive system. With constant exposure to harmful products, the patient develops an inflammatory process in the organ mucosa.
- Mechanical influence. With prolonged constipation, fecal stones form in the digestive system. They have a hard consistency and a rough surface, so when passing through the intestines they severely injure the mucous membrane.
Diagnostics
- Colonoscopy. An endoscopic examination allows you to carefully examine the mucous membrane of the large intestine and detect characteristic inflammatory changes in its wall. During the procedure, you can take a fragment of the organ mucosa - a biopsy sample.
- Histological examination. The resulting mucosal sample can be examined under a microscope and its cellular composition can be determined. The study allows you to confirm the diagnosis of enterocolitis and carry out differential diagnosis with other diseases.
- Coprogram. Stool examination reveals characteristic microscopic changes - the presence of leukocytes, mucus and blood.
Differential diagnosis of the disease should be carried out with the following diseases:
- peptic ulcer of the stomach and intestines;
- botulinum toxin poisoning;
- acute intestinal obstruction;
- arsenic or mushroom poisoning;
- acute appendicitis.
It is necessary to differentiate the disease on the basis of the clinical picture of the disease, as well as data from laboratory and instrumental studies.
Treatment
To eliminate enterocolitis, it is necessary to carry out complex therapy: drug treatment and general recommendations aimed at improving the patient’s condition.
Diet
If you have enterocolitis, the patient must follow the principles of a healthy diet. These include the following recommendations:
- eat 4-6 times a day;
- eat in small portions, avoid overeating;
- be sure to have breakfast every day;
- do not eat at night, take your last meal at least 4 hours before bedtime;
- completely limit the consumption of alcoholic beverages, do not smoke during treatment.
| Recommended Products | Not Recommended Products |
|
|
Drugs
Antibiotics. The main treatment for infectious enterocolitis is antibacterial drugs. These include:
- Amoxicillin;
- Furazolidone;
- Cefotaxime;
- Nifuroxazide;
- Ceftriaxone;
- Metronidazole.
Enzymes. During the inflammatory process in the intestines, the digestion of foods is disrupted, which leads to insufficient intake of metabolites into the body.
To normalize digestion, the patient is prescribed enzyme therapy. This group includes lipase, protease, amylase, pancreatin.
Before starting to use medications, you should consult your doctor to determine the required dosage.
Fixing drugs. To eliminate diarrhea, drugs are used that normalize the muscle activity of the intestines. The most common drugs are Loperamide and Mebeverine.
Probiotics and prebiotics. They are necessary to restore intestinal microflora, which usually suffers during the inflammatory process in the intestines.
Folk remedies
To eliminate the inflammatory process, special microenemas are used. They quickly relieve diarrhea and flatulence. Herbal decoctions are taken into enemas:
- chamomile;
- oak bark;
- bird cherry;
- St. John's wort;
- sea buckthorn.
Traditional methods of treatment should not be used as a replacement for drug therapy. Medicines can only relieve the symptoms of the disease, but are not able to influence the cause of the pathology. Therefore, traditional therapy should be part of a comprehensive, comprehensive treatment.
Read more: Use of herbs for inflammation of the gastrointestinal tract
Possible consequences of pathology and prognosis for life
Possible complications of enterocolitis include:
- acute cholecystitis;
- angiocholitis;
- hepatitis;
- anemia;
- intestinal perforation;
- acute peritonitis.
The disease usually has a favorable prognosis . If treatment is started in a timely manner, the symptoms of enterocolitis quickly disappear without serious consequences. If therapy is started late, complications may occur.
Inadequate treatment, completed prematurely, often leads to the fact that the acute disease becomes chronic and is present in the patient for many years. Therefore, it is so important to start therapy for enterocolitis in a timely manner.
Prevention
- balanced and nutritious nutrition (read here);
- active lifestyle, adequate physical activity;
- competent use of medications, especially antibiotics and anti-inflammatory drugs;
- timely elimination of parasitic infestation;
- regular examinations by a gastroenterologist;
- See a doctor if symptoms of inflammatory processes in the intestines appear.
Source: //ProKishechnik.info/zabolevaniya/enterokolit.html
Signs of the disease
Symptoms of enterocolitis are as follows. If the disease begins abruptly, it is accompanied by:
- rumbling in the stomach and bloating;
- nausea and vomiting;
- abdominal pain;
- coating on the tongue;
- diarrhea.
If the disease is infectious in nature, then mucus may be present in the stool, and rarely blood. Body temperature may also increase, and symptoms similar to those of intoxication will appear: muscle aches, general weakness, severe headaches.
The chronic form of the disease does not appear noticeably at first. But there are cases when the disease immediately affects the body, and with the occurrence of complications that are dangerous to human health and life.
Symptoms of chronic intestinal enterocolitis:
- Mild pain in the abdominal area. Depends on the severity of the disease. Most often, dull pain occurs after lunch. If the large intestine is inflamed, the pain will be more severe. During physical activity and after eating, the pain intensifies.
- Flatulence. Occurs due to intense formation of gases.
- Problems with bowel movements. Systematic diarrhea and constipation.
- Weight loss. It is observed in people suffering from inflammation of the small intestine.
Diagnostics
Acute enterocolitis is diagnosed after taking an epidemiological history from the patient, and if the main symptoms are pronounced, after examining the stool for the presence of bacteria.
The chronic form is determined after a survey, medical history, physical laboratory examination and instrumental diagnostics.

The most effective method for diagnosing colon disease is colonoscopy. During this examination, all erosions, destruction of the mucous membrane, ulcers, etc. are detected. That is, inflamed areas of the large intestine.
Another method for diagnosing enterocolitis is x-ray examination. With its help, you can identify all changes in the intestinal lumen, its defects, and the nature of the structure.
Video: How to cure enterocolitis
- Daytime sleepiness
- What is the T4 hormone responsible for in women?
- Inflammation of the sciatic nerve
- Fallopian tubes are not visualized on ultrasound
- The tip of the tongue goes numb - what does this mean?
- Pain in the left side of the lower abdomen in men
- White spots on the skin
- Chronic metroendometritis in women
- Pregnancy with adenomyosis
- Treatment of ENT diseases in a sanatorium
- The first signs of diabetes
- Treatment of diseases of the cardiovascular system in a sanatorium
Treatment of the disease
Treatment of enterocolitis in adults begins with switching to a tea-water diet. If necessary, the patient's stomach is washed. If severe vomiting and diarrhea are observed (that is, the body loses a lot of fluid), rehydration therapy is prescribed. The diet for enterocolitis should consist of porridges cooked in water and rice broth.
Infectious enterocolitis is treated with antibiotics and sulfonamide-based drugs. To prevent dysbiosis when treating a disease, a person should also take medications that normalize the intestinal flora.
How to treat enterocolitis if it is chronic? First you need to eliminate all the factors that provoke it:
- Adhere to a strict diet.
- Stop taking medications that disrupt bowel function.
- Get rid of diseases and infections of the digestive system.
As soon as the cause is eliminated, digestive problems are treated, and then dysbacteriosis therapy is prescribed. Read more about drugs for the treatment of dysbiosis →
The diet prescribed by the doctor for enterocolitis must be strictly followed. The consumption of all foods that cause intestinal upset is limited.
Treatment of intestinal enterocolitis in young children also begins with a balanced diet. The doctor prescribes the treatment of enterocolitis with drugs that stimulate metabolic processes in the body. If the baby has severe pain, the doctor prescribes painkillers.
In principle, enterocolitis in a child is treated in the same way as in an adult. A tea-water diet, low-fat meat broths, grated gruels and soups are prescribed. All foods that irritate the intestines are excluded.

Necrotizing enterocolitis in newborns is quite common. Its treatment differs from other subtypes of the disease. Thus, parenteral nutrition is prescribed with the complete abolition of normal nutrition and oral medications. Treatment is carried out under the strict supervision of a doctor using serious therapeutic measures.
Diet
Necrotizing enterocolitis (just like its other type) is treated with strict adherence to a diet, which doctors call Table No. 4. It is characterized by the following aspects:
- Light meals to prevent intestinal congestion.
- The intestinal flora should recover quickly.
- The diet must be complete.
The patient should not consume dairy products or hot spices. He should also give up smoked, salted and fried foods. You need to eat a couple of times a day.
What is special about the diet for enterocolitis in children and adults? diet for colitis and enterocolitis
Before prescribing proper nutrition, the doctor performs several procedures on the patient - gastric lavage, an enema to cleanse the intestines.
Then it is advisable for the patient to refuse to eat any food for 2 days and undergo therapeutic fasting.
It, in combination with medical measures, will have a positive effect on the mucous membrane of the small and large intestines.
During these days, you should definitely drink a lot of liquid, it can be plain water, weakly brewed tea. And already on the 3rd day, gentle nutrition is allowed. A person’s diet is gradually expanded by adding 2 products per week.
A patient with a disorder of the small intestine or colitis should adhere to the following recommendations:
- eat food in small portions, but often, at least 5 times a day;
- the menu should be dominated by products with vitamins B, C, PP;
- exclude spicy, fried, salty foods;
- It is not recommended to take fresh vegetables, only boiled, stewed, baked;
- do not eat dry food, refuse fast food;
- limit mayonnaise, seasonings, ketchup or take in small quantities;
- chew food thoroughly, the stomach digests small particles faster, and large ones provoke pain;
- products must be of high quality, healthy, use only freshly prepared food.
You need to eat boiled, steamed, stewed food. Food should be chopped during or after cooking. To normalize digestion, it is advisable to always have meals at the same time. When food enters the stomach at different times, hydrochloric acid agitates the walls of the intestines and stomach.
Forms of enterocolitis and nutrition
Enterocolitis occurs in 3 forms, each of them has its own dietary composition:
- Acute - in case of exacerbation of the disease, diet No. 4 is used.
- Chronic – at the time of chronic development, diet No. 3 is used.
- Remission period - when the symptoms decrease or are completely eliminated, the doctor prescribes table No. 2.
Treatment for intestinal enterocolitis with proper nutrition will speed up the recovery process.
Dietary nutrition should be carried out both at the time of exacerbation of enterocolitis and during remission. Each stage of the disease contains a separate table.
Table No. 4
Acute forms are characterized by the following symptoms: malaise, abdominal pain, diarrhea during the first days, malaise. There is swelling and rumbling. Intoxication of the body, presence of blood in the stool.
Nutritional value is 2050 kcal. The main purpose of table No. 4 is gentle nutrition, reduction of inflammatory and fermentation processes. This happens when cooking food by steaming, grinding, or boiling. Meals are small and frequent.
You need to avoid foods that increase peristalsis, contain a lot of fiber, have a high percentage of fat, and have an irritating effect:
- milk porridge, milk, fermented baked milk and other fatty products;
- black bread and crackers from it;
- oatmeal, semolina, wheat groats;
- barley, pearl barley;
- fatty broths, meat, fish;
- grapes, plums;
- legumes, pasta;
- cabbage, beets, turnips;
- fresh fruits and vegetables;
- sweets, chocolate;
- kvass, soda, coffee.
It is imperative to reduce the chemical, physical, and temperature effects on the intestinal walls. This will reduce the likelihood of fermentation and putrefaction.
In acute form of enterocolitis, you can eat:
- applesauce;
- wheat crackers;
- rice, buckwheat porridge (you can add a little butter to them);
- steamed omelette or 1 soft-boiled egg;
- meat, fish pate;
- soups with light meat broth, which can be supplemented with boiled minced meat;
- homemade low-fat cottage cheese, yogurt;
- herbal decoctions, still water, berry jelly;
- sweet apples.
Drinks also include green tea, compotes, and juices made from sweet fruits and vegetables. Decoctions of rose hips, quince, and currants have many beneficial properties for the body.
Table No. 3
Dietary therapy for the chronic form of the disease is slightly different. The menu should be dominated by protein, no more than 120 g per day. Nutritional value – up to 3200 kcal. Table No. 3 is suitable for people with frequent constipation and indigestion.
Recommended Products:
- black bread;
- cottage cheese, milk, yogurt;
- beets, carrots, tomatoes, cucumbers;
- pea soup, borscht, first courses with cauliflower;
- boiled fish (navaga, hake, carp);
- 2 eggs per day;
- dietary meat (rabbit, nutria, beef).
It is allowed to eat non-chopped products, but there should not be large particles. Plant products can be eaten raw or cooked.
Strict dietary nutrition is carried out for 2 months until the intestinal mucosa and the functioning of the digestive system improve.
Table No. 2
Table No. 2 implies proper nutrition for enterocolitis with minor restrictions. This treatment is aimed at maintaining the body, for speedy rehabilitation and recovery. Calorie content is up to 3000 kcal.
Indicative menu during the period of remission (one of the recipes to choose from):
- breakfast: rice, buckwheat or semolina porridge, steamed omelette, cottage cheese casserole, noodles with cheese, pumpkin puree, tea;
- second breakfast: fruit jelly or mousse, baked apples, rosehip broth;
- lunch: for the first course you can eat vegetable soup, with noodles and beef, pickle soup, rice soup or with meatballs; for the main course: chicken cutlet, beef stroganoff, meatballs, buckwheat with meat;
- dinner: fruit salad, boiled vegetables, cottage cheese with sour cream, stewed or jellied fish, chicken chop, pumpkin puree, noodle soup with boiled meat.
The list of vegetables (beets, cabbage, eggplants, tomatoes) and fruits (strawberries, raspberries, tangerines) is significantly increasing.
The use of a diet in adults with enterocolitis of this form should be used for a long time until the patient’s condition is completely restored.
Food for children
With a diagnosis of enterocolitis, a child is prescribed the same diet as an adult. Having determined the disease, the specialist prescribes a complex of vitamins, medications, and a diet menu for the baby, depending on the symptoms.
For intestinal infections, antibiotics, anti-inflammatory, and painkillers are used. The regimen and diet are established by the attending nutritionist; after the prescription is written, you must strictly adhere to it.
At first, difficulties may arise with treatment; it is difficult for the baby to understand why he is not given sweets or other foods that the child likes. Young patients need to be fed at least 5-6 times a day.
A child's diet may consist of:
- crushed soups, porridges;
- low-fat light broths;
- Cabbage juice will help relieve pain;
- steamed fish, meat;
- a little later - savory pies and buns.
It is advisable not to consume prohibited foods in front of the child, so as not to tempt the child, otherwise the psyche may be damaged.
Authorized Products
The basis of the diet is:
- Porridge in pureed form (rice, buckwheat, oatmeal). They are prepared in water or weak broth. Butter is added in the amount of 0.5 tsp per serving. You should not eat millet, barley, pearl barley and corn porridge.
- Soups in water, later - in low-fat fish/meat broth. They add cereals, some vegetables (carrots, potatoes, zucchini, pumpkin), egg flakes, pureed meat, and meatballs.
- Dried wheat bread and crackers, biscuits.
- Lean beef, rabbit, chicken and turkey, veal. You should choose quality meat without tendons or fascia, and remove the skin from the bird before cooking. Meat is prepared in the form of steamed minced products: minced meat, pate, cutlets, meatballs, meatballs. Some meat products can be stewed with water.
- Low-fat varieties of fish from which quenelles, cutlets, soufflés, pates and meatballs are prepared. All fish products are also steamed.
- If tolerated well, boiled vegetables in the form of puree are allowed.
- Eggs in the amount of one per day in the form of an omelet or soft-boiled. Beaten eggs can be added to soups to create flakes.
- Well pureed non-acidic cottage cheese, you can use it to prepare steam soufflés and casseroles.
- Berry jelly (blueberries, rowan, quince, bird cherry, dogwood, persimmon, pears are used), pureed fresh and baked apples. Diluted fresh juices are gradually introduced (non-acidic berries are used). You should not give your child grape, plum and apricot juice, as they have a laxative effect.
- Herbal teas (from bird cherry, dogwood, blueberry), rosehip decoction, filtered water.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal |
Vegetables and greens
zucchini 0.6 0.3 4.6 24 potatoes 2.0 0.4 18.1 80 carrots 1.3 0.1 6.9 32 pumpkin 1.3 0.3 7.7 28
Source: https://GolovaNeBoli.ru/diety/dieta-pri-enterokolite-pravila-pitaniya-i-prognoz-na-budushhee.html
Forecasts
Colitis and enterocolitis can be completely cured if the disease is detected in time and the correct measures are taken to treat it. After this there should be no consequences. In just 1–1.5 months, the flora will be completely restored.

The course of the chronic form of the disease directly depends on the timeliness of its diagnosis, as well as on the elimination of the causes of its occurrence and the correct sequence of measures to normalize a person’s habitual lifestyle.
Prevention
Prevention of intestinal diseases consists of measures taken to avoid factors leading to the occurrence of enterocolitis. These include:
- Quickly identify intestinal problems and eliminate them.
- Maintaining a proper diet.
- Taking medications as prescribed.
From our material you learned the symptoms of enterocolitis, how treatment is carried out in children and adults. We figured out the types of enterocolitis and diets.
It is worth noting that this disease cannot be treated with folk remedies. This approach will lead to complications in most cases. This is especially true for staphylococcal and viral enterocolitis.
Enterocolitis in newborns is especially dangerous. Therefore, if you notice the symptoms described above in yourself or your child, be sure to consult a doctor!
Author: Daria Tyutyunnik, doctor, especially for Zhkt.ru