3389
Obstructive jaundice is a pathological condition of the biliary system, in which the lumen of the gallbladder or ducts is closed by some obstacle that disrupts the normal outflow of secretions. Clinically, this pathology is manifested by rapid discoloration of the skin and visible mucous membranes in yellow shades, painful sensations in the right side, darkening of urine and an increase in some specific indicators in a blood test.
Treatment of obstructive jaundice can only be surgical, since this condition is characterized by severe disturbances in the body. In fact, this pathology is a blockage of the lumen of the bile ducts, and it is impossible to eliminate the obstacle with medications.
If timely assistance is not provided in time, a serious complication may develop and death may occur.
Causes
The etiology of occurrence may be different. Classification:
- Malformations of the biliary system.
- Benign changes in the biliary system and pancreas.
- Organ tumors.
- Changes in the main bile ducts due to surgery.
- Parasitic lesions.
Obstructive jaundice often occurs in oncology and gallstone disease. The mechanism of pathology development is complex. Often the provocateur is an inflammatory process that affects the bile ducts. Inflammation leads to the development of edema and thickening of the mucosa. Because of this, the lumen of the ducts narrows. If even small stones enter, the flow of bile can completely stop.
Bile accumulates in the bile ducts and dilates them. Liver cells are destroyed, bilirubin and bile acids enter the bloodstream. The process of entry of bile acids into the intestines is disrupted. Bilirubin is highly toxic and has a poisonous effect on the body.
Factors contributing to the development of the disease:
- Sudden loss or gain of body weight.
- Infectious pathologies of the liver and pancreas.
- Abdominal surgery on the liver and biliary tract.
- Abdominal injuries.
How is bilirubin level determined?
Using a blood test, you can determine both the total level of bilirubin in the blood, which includes direct and indirect types, and each separately. The norm for total bilirubin is considered to be 3.4–17.1 µmol/l (error of about 10–15%), for direct - no more than 7.9 µmol/l, for indirect - up to 16.2 µmol/l. However, you should not independently interpret the results obtained. The diagnosis can only be made by a doctor, based on the general condition of your body and medical history.
In addition to a general blood test to diagnose jaundice, your doctor may prescribe:
- Blood chemistry;
- Ultrasound, computed tomography;
- Endoscopic retrograde cholangiopancreatography (ERCP) or puncture cholangiography, which allows examination of the bile ducts.
Take care of yourself, book a consultation now
Symptoms
A medical history is a protocol for examining a patient, where a description of all symptoms is recorded. Clinical signs develop slowly. Often, inflammation of the biliary tract occurs first. The clinic includes:
- Pain in the area of the right hypochondrium.
- Increase in body temperature.
- General weakness.
- Poor appetite.
- Headache.
Then a yellow coloration of the skin and mucous membranes occurs. Other signs of pathology:
- Pain in the right hypochondrium.
- Dark urine and discolored stool.
- Itching.
- Dyspeptic disorders.
- Poor appetite and weight loss.
- Increased body temperature.
- Enlargement of the liver.

With obstructive jaundice, the patient must receive prompt medical attention. Otherwise, due to the massive death of hepatocytes, liver failure is possible. Symptoms appear:
- Severe weakness.
- Drowsiness.
- Coagulopathic bleeding.
The progression of liver failure leads to brain damage. Multiple organ failure is observed. If there is a blockage of the bile ducts, then spastic, sharp pain appears, radiating to the chest area, right armpit and shoulder blade.
External signs are revealed 1-2 days after the hepatic colic subsides. The liver is painful. If you press in the area of the right hypochondrium, an involuntary holding of breath occurs.
Pancreatic cancer causes a dull pain that radiates to the back. A distended bladder can be felt, pressing on which does not cause pain. The liver increases in size and becomes dense. Itching and poor appetite appear first.
An enlarged liver is a common symptom of prolonged obstructive jaundice. This occurs due to a large amount of bile and inflammation of the bile ducts.
One of the first signs is itchy skin. It cannot be treated. Scratches and bruises appear on the skin. Weight loss is observed with jaundice due to cancerous tumors.
Body temperature is elevated and does not fall. This is a specific sign of subrenal jaundice, distinguishing it from viral hepatitis.

Subrenal jaundice in a patient
Pancreas cancer
Pancreas cancer
– a tumor lesion arising from the pancreatic ducts or pancreatic parenchyma. Symptoms of pancreatic cancer include nausea, loss of appetite, upper abdominal pain, bowel dysfunction, weight loss, and icteric discoloration of the sclera and visible mucous membranes.
To detect pancreatic cancer, laboratory (determination of biochemical parameters and blood tumor markers) and instrumental diagnostics (ultrasound, CT, MRI, ERCP) are used. Radical treatment involves resection of the pancreas to varying extents; Radiation and chemotherapy treatment may be used.
The concept of “pancreatic cancer” includes a group of malignant neoplasms that develop in the parenchyma of the pancreas: the head, body and tail. The main clinical manifestations of these diseases are abdominal pain, anorexia, weight loss, general weakness, and jaundice.
Every year, 8-10 people out of every hundred thousand people in the world develop pancreatic cancer. In more than half of cases, it occurs in elderly people (63% of patients diagnosed with pancreatic cancer are over 70 years of age).
Men are more prone to this type of malignancy; they develop pancreatic cancer one and a half times more often.
A malignant tumor of the pancreas is prone to metastasis to regional lymph nodes, lungs and liver. Direct tumor growth can lead to its penetration into the duodenum, stomach, and adjacent parts of the large intestine.
Pancreas cancer
The exact etiology of pancreatic cancer is not clear, but factors contributing to its occurrence are noted. However, in 40% of cases, pancreatic cancer occurs for no apparent reason. The risk of developing cancer increases markedly in people who smoke a pack or more of cigarettes daily, who consume large amounts of carbohydrate-containing foods, and who have undergone gastric surgery.
Diseases that contribute to the development of pancreatic cancer include:
The likelihood of developing cancer increases with age.
Pancreatic cancer is classified according to the international TNM classification system for malignant neoplasms, where T is the size of the tumor, N is the presence of metastases in regional lymph nodes, and M is metastases in other organs.
However, in this case, the classification is not sufficiently informative regarding the operability of cancer and the prognosis of the effectiveness of therapy, since the general condition of the body plays a significant role in the prospect of cure.
Pancreatic cancer is accompanied by the following clinical manifestations: abdominal pain in the area of the pancreas (upper half, radiating to the back, sometimes encircling). As the tumor grows, the pain symptom intensifies. Pancreatic pain is characterized by intensification when bending over.
When a tumor of glandular tissue is localized in the area of the head of the pancreas, the vast majority of cases experience jaundice, which may be accompanied by skin itching, darkening of urine and discoloration of feces.
Another common symptom of a malignant pancreatic tumor is weight loss. When the tumor is localized in the body and tail of the pancreas, weight loss is noted in all patients; with cancer of the head of the pancreas, body weight decreases in 92% of patients. This symptom is associated with impaired absorption of fats in the intestines as a result of insufficiency of the sectoral function of the pancreas.
In 64% of cases of pancreatic head cancer, anorexia is observed (in other tumor locations, this symptom is observed in only 30% of patients). When a large tumor compresses the duodenum or the lumen of the stomach, vomiting may occur. Secondary diabetes mellitus develops in 25-50% of cases and is usually accompanied by polyuria and polydipsia.
When the tumor is localized in the body or tail of the pancreas, splenomegaly and varicose veins of the esophagus and stomach (with episodes of bleeding) may be observed. Sometimes the clinical picture follows the type of acute cholecystitis or pancreatitis. If the peritoneum is affected by metastases, intestinal obstruction is possible due to narrowing of the intestinal lumen.
The course of pancreatic cancer is characterized by a gradual increase in symptoms, ranging from a mild, mild pain syndrome to a pronounced, varied clinical picture. If you consult a doctor in a timely manner and detect a tumor early, the prognosis for treatment and subsequent survival is significantly improved.
Malignant tumors of the pancreas are complicated by:
- diabetes mellitus
- malabsorption syndrome
- disorders of the bile circulation system
- trophic disorders due to impaired secretory function of the pancreas.
The tumor can grow into nearby organs - the stomach, small intestine, large intestine. Large tumors can contribute to intestinal compression and obstruction.
Diagnosing cancer at an early stage presents certain difficulties due to the lack of specific clinical manifestations. Only in 30% of cases the detected cancer is not older than two months.
Laboratory diagnosis
- A complete blood count shows signs of anemia; an increase in platelet count and acceleration of ESR may be noted. A biochemical blood test shows bilirubinemia, increased activity of alkaline phosphatase, liver enzymes with destruction of the bile ducts or metastasis to the liver. There may also be signs of developed malabsorption syndrome in the blood.
- Determination of tumor markers. The CA-19-9 marker is determined to resolve the issue of tumor operability. In the early stages, this marker is not detected in pancreatic cancer. Cancer embryonal antigen is detected in half of patients with pancreatic cancer. However, it is worth noting that a test for this marker can also be positive in chronic pancreatitis (5% of cases) and ulcerative colitis. CA-125 is also noted in half of the patients. In the later stages of the disease, tumor antigens can be detected: CF-50, CA-242, CA-494, etc.
Instrumental diagnostics
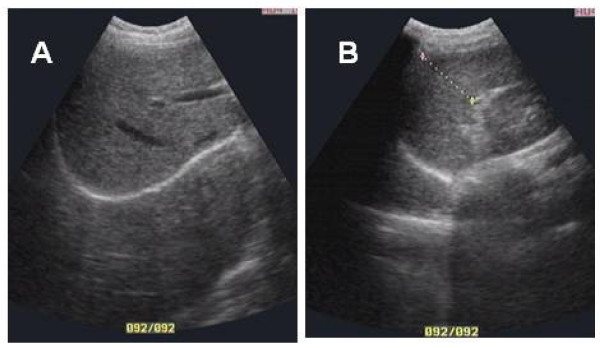
- Endoscopic or transabdominal ultrasonography. Ultrasound of the abdominal organs excludes diseases of the gallbladder and liver and can detect a tumor of the pancreas. Endoscopic examination makes it possible to take a biopsy sample for research.
- Computed tomography and MRI make it possible to visualize pancreatic tissue and detect tumor formations from 1 cm (CT) and 2 cm (MRI), as well as assess the condition of the abdominal organs, the presence of metastases, and enlarged lymph nodes.
- Positron emission tomography (PET) can identify malignant cells, detect tumors and metastases.
- ERCP detects tumors of any part of the pancreas measuring 2 cm or more. However, this procedure is invasive and contributes to the development of complications.
CT scan of the abdominal organs.
Tumor of the head of the pancreas (red arrow), pronounced dilation of the Wirsung duct with atrophy of the body and tail of the pancreas (blue arrow)
To identify small metastases in the liver, on the intestinal mesentery or peritoneum, diagnostic laparoscopy is performed.
Since most patients suffering from a malignant tumor of the pancreas have signs of malabsorption and anorexia, they are shown a diet high in fat and protein. The drug treatment for pancreatic cancer is chemotherapy.
Treatment is carried out with drugs that suppress the growth of cancer cells (fluorouracil, streptozocin, semustine, etc.). Either one drug or several in combination can be prescribed. Non-surgical treatment methods also include radiation therapy.
Dosages and course duration are chosen depending on the size of the tumor, stage of the disease, and general condition of the patient.
Palliative treatment for pancreatic cancer is aimed at relieving the main clinical symptoms: pain relief, correction of bile duct patency to treat jaundice.
If it is impossible to restore bile circulation, cholestyramine and phenobarbital are prescribed.
Insufficiency of exocrine pancreatic function is corrected with the help of enzyme preparations (lipase, amylase, protease, pancreatin).
Surgical treatment of pancreatic cancer is carried out by resection of the altered tissue of the gland and surrounding organs.
If it is possible to surgically remove the tumor, they often resort to radical surgery (the entire pancreas, gallbladder with bile duct, duodenum, adjacent area of the large intestine and stomach are removed). The survival rate after such an operation is 25% of patients within five years.
Prevention of pancreatic cancer includes the following measures: cessation of smoking and alcohol abuse, timely and complete treatment of diseases of the pancreas and biliary tract, proper correction of metabolism in diabetes mellitus, adherence to a diet, a balanced diet without overeating and a tendency to fatty and spicy foods. Patients who have undergone gastric surgery need to be attentive to the symptoms of pancreatitis.
Persons suffering from pancreatic cancer are under the supervision of specialists in gastroenterology, oncology, a surgeon and a radiologist.
When pancreatic cancer is detected, in most cases the prognosis is extremely unfavorable, about 4-6 months of life. Only 3% of patients achieve five-year survival. This prognosis is due to the fact that in most cases pancreatic cancer is detected at late stages and in elderly patients, which does not allow radical removal of the tumor.
Source: //www.KrasotaiMedicina.ru/diseases/zabolevanija_gastroenterologia/pancreatic-cancer
Obstructive jaundice in oncology
The pathogenesis of jaundice in oncology is simple. The tumor grows and compresses the blood vessels and bile ducts. Stagnation of bile occurs. The patient will notice such a symptom as yellow skin. Then itching appears. The patient scratches the skin and creates an entry point for infection.
With this disease, the liver cannot cope with large amounts of bilirubin, it poisons the entire body. The development of obstructive jaundice in oncology leads to death. Such a patient requires surgical intervention, but no surgeon will perform an operation until the symptoms of jaundice are relieved.
Klatskin tumor is a rare oncological pathology that affects the bile duct. There are 4 stages. The first signs appear in the later stages. When diagnosing the fourth stage, treatment does not bring results. Symptomatic therapy is prescribed.
For cancer of the tail and body of the pancreas, these organs and the gallbladder are removed. Sometimes the spleen is removed along with them. They live on average 10-12 months after surgery. After the intervention, 10-12% of patients die.
Clinical diagnostic guidelines
The patient is admitted to the hospital in the surgical or gastroenterology department. Diagnosis begins with ultrasonography of the biliary tract and pancreas.
It is not difficult to make a preliminary diagnosis if the disease develops against the background of a neoplasm. An advanced tumor can be easily palpated. Once symptoms of cholestasis begin, diagnosis becomes difficult. The general clinical picture is similar to many pathologies.
In the early stages, it is difficult to distinguish viral hepatitis from intrahepatic cholestasis, since high levels of cholesterol, bilirubin and alkaline phosphatase are characteristic of both pathologies.
Instrumental methods are used:
- Ultrasound. Its results reveal an enlargement of the bile ducts, the presence of stones and focal pathologies of the parenchymal organ.
- Relaxation duodenography. Conditions of artificial hypotension are created and an X-ray of the duodenum is performed. Frostberg syndrome can be diagnosed using this method.
- Endoscopic retrograde cholangiopancreatography. If there is a suspicion of blockade of the BDS, when the ultrasound results are not informative enough, the RCCP method is used. A contrast agent is injected into the duct and several x-rays are taken. Using this method, small tumors can be identified and cytology and histology can be performed. The disadvantage of the method is the development of complications after the study.
- Percutaneous transhepatic cholangiography. Carry out in the presence of blockage of the bile ducts at the gates of the liver. First, the patient is given local anesthesia. Then a thin needle with a contrast agent is inserted through the skin and liver tissue. The procedure is carried out under supervision through an ultrasound machine. Complications are possible after the manipulation.
- Radioisotope scan of the liver. Using this method, tumors and parasitic lesions are detected.
- Laparoscopy. It is used when the information content of other methods is insufficient. Metastases are detected using laparoscopy.
Patient's liver examination
Conduct laboratory tests:
- Coagulogram.
- Biochemistry of blood.
- UAC.
- Coprogram.
Diagnosis of jaundice
Diagnostic measures for jaundice are complex and aimed at determining the severity of the pathology itself, as well as the reasons that caused it. The following research methods are used:
Laboratory research. The main laboratory marker of jaundice is an increase in bilirubin. In the blood it exists in the form of two fractions - free and bound. With obstructive jaundice, at the initial stage there is an increase in the bound, direct bilirubin, then the amount of indirect bilirubin increases. Indicators that change with the development of cholestasis are also determined - cholesterol, lipids, alkaline phosphatase, GGTP, etc.

Ultrasound examination of the abdominal cavity, liver, bile ducts and retroperitoneal space. With obstructive jaundice, dilated bile ducts and hyperplasia of their walls will be detected. In some cases, it is possible to visualize the presence of a pancreatic tumor and determine its growth into the bile duct, or its compression by tumor masses.
A more informative method for visualizing a pancreatic tumor is CT and/or MRI with contrast . These methods make it possible to visualize the tumor and its relationship with surrounding tissues in more detail, and to detect metastases, including in regional lymph nodes or the liver.
Study of the patency of the bile ducts. Allows you to visualize the lumen of the ducts and detect places of their narrowing or obstruction. For this purpose, retrograde cholangiopancreatography is performed - using endoscopic technology, a radiopaque substance is injected into the lumen of the large duodenal papilla (the place through which the bile and pancreatic ducts open into the lumen of the duodenum) and photographs are taken in which the ductal system is visualized. The endoscope is inserted through the mouth. Before the procedure begins, the patient receives light sedation, and the throat is irrigated with an anesthetic solution to weaken the gag reflex.
Another method for visualizing the ductal system is percutaneous transhepatic cholangiography. In this case, contrast is administered through puncture of the hepatic ducts through the anterior abdominal wall. Ultrasonic guidance is used to correctly target the required area. After the contrast fills the ducts, X-rays are taken, which clearly show the hepatic ducts and their sites of obstruction.
Book a consultation 24 hours a day
+7+7+78
Treatment
Patients with obstructive jaundice are sent to hospital for treatment. The treatment regimen is aimed at eliminating bile stagnation and preventing liver failure.
Often the disease is eliminated using surgery. It depends on the cause that caused the jaundice. Surgery is the only effective way to restore the patency of the bile ducts. Surgical operations can be divided into two groups:
- Minimally invasive.
- Direct.
Minimally invasive methods are effective and at the same time low-traumatic. But it is impossible to carry them out in all patients; there are limitations. These include:
- Endoscopic papillosphinctertomy and lithoextraction.
- Local lithotripsy and lithoextraction.
- Bougienage and stenting of the bile ducts.

When carrying out such manipulations, a gastroduodenoscope and other special instruments are used. With their help, you can crush and remove stones, install stents, and remove tissue. Often operations are performed without anesthesia; there is no need for long rehabilitation.
If it is impossible to decompress the biliary tract using a gastroduodenoscope, percutaneous transhepatic cholangiostomy is performed. Under the supervision of ultrasound or x-ray, drainage of the bile ducts is installed. The bile is drained through a drainage tube, and medications are administered through it.
Direct operations are performed to provide full access to the gallbladder and eliminate the pathological factor. The operation can be performed using laparoscopic instruments or an open cavity method. The second method is the most traumatic, requires a long recovery, and the likelihood of complications increases. Because of this, it is used only in difficult situations.
All treatment is divided into two stages. The first includes non-surgical therapy and minimally invasive methods. These manipulations are carried out in the first days after the patient’s admission. If the effectiveness of the first stage is low, proceed to the second. It includes surgical operations. After the operation, there is a risk of complications, so such measures are taken only in extreme cases.
According to statistics, 30% of operations are unsuccessful. Even partial drainage is considered a good result.
Drug therapy is also being carried out. Treatment can be symptomatic or aimed at reducing the likelihood of complications, as well as preparing the patient for surgery. The amount of drug therapy administered depends on the severity of the disease. A seriously ill patient is admitted to the intensive care unit. He is prescribed:
- Infusion therapy.
- Forced diuresis.
- Vitamin complexes.
- Hepatoprotectors.
- Amino acids.
- Metabolism stimulants.
- Hormonal agents.
To relieve symptoms, antispasmodics, enveloping agents, antacids and other medications are prescribed.
Therapy comes down to eliminating the pathology that caused the development of obstructive jaundice. In this case, non-surgical and surgical therapy is carried out. Traditional medicine and self-medication are ineffective. They allow you to relieve symptoms and alleviate the patient’s condition for a short period of time. But at the same time, jaundice continues to progress, complications develop. Therefore, when the first symptoms appear, the patient needs qualified medical care.
Diet
Complex therapy includes dietary nutrition. This helps reduce the load on the liver. It is necessary to maintain water balance and drink 2 liters of fluid per day to remove bilirubin.

Before surgery, drink drinks rich in carbohydrates (compote, sweet tea). They do not overload the liver, supply the body with the necessary energy and improve metabolism.
After the operation, the diet includes juices, cereals with milk and vegetable puree soup. The products are consumed pureed, at room temperature. With the permission of the attending physician, the diet includes boiled or steamed fish and meat. The number of meals should be up to six.
You need to limit fats. If well tolerated, it is allowed to consume a small amount of butter or vegetable oil. It is prohibited to consume animal fats.
You need to exclude fatty dairy products, legumes, grapes, fatty meat and fish, smoked foods, soda, coffee, and canned vegetables from your diet.
If the patient's condition is stable, yesterday's or dried white bread and low-fat dairy products are allowed.
Forecast
The disease can last from several days to several months and depends on the primary pathology.
If the problem is diagnosed in time and adequate therapy is provided, the outcome will be favorable. The situation worsens if there is a tumor that compresses the bile duct. If left untreated, the following pathologies develop:
- Cirrhosis of the liver.
- Bilirubin encephalopathy.
- Sepsis.
- Liver failure.
Life prognosis and consequences depend on the patient. If he follows the diet and clinical recommendations, then the likelihood of relapse and complications is minimized. In the opposite situation, the risk of recurrent disease is high. The likelihood of complications also increases.