Intestinal tuberculosis is a chronic infectious disease caused by mycobacteria. This pathology is relatively rare. Most often, it develops secondary to the spread of mycobacteria throughout the body. Untimely treatment of tuberculosis leads to intestinal bleeding, difficulty defecating, peritonitis, acute appendicitis and other complications.
Mycobacterium that causes intestinal tuberculosis.
Diagnostics
Detection of intestinal tuberculosis at an early stage is almost impossible, since there are no specific diagnostic methods. The diagnosis is established by a combination of signs, the only indisputable one being the isolation of mycobacteria from biological fluids. However, this analysis takes time - the initial isolation and identification of the pathogen requires from 4 to 8 weeks.
At the initial consultation, the gastroenterologist can only assume the presence of a specific lesion. The diagnosis becomes clear in the later stages, namely with the development of caseous necrosis (dead tissue in appearance resembles cottage cheese).
The following methods are used:
- general blood test - increase in the number of leukocytes, eosinophils, decrease in lymphocytes, shift in ESR;
- coprogram - establishes the type of digestive disorder, but mycobacteria are almost never detected;
- intradermal tuberculin tests - are positive only in half of the patients, the reaction is not highly specific, and may be positive if infected with other microorganisms or decreased immunity;
- X-ray of the intestines, regular and with contrast, reveals calcified lymph nodes, ulcerative defects, tuberous infiltrates, changes in the mucosa;
- colonoscopy - ulcers of irregular shape, inextensibility of the walls, pseudopolyposis formations, narrowing of the lumen are visible;
- biopsy – tissues affected by mycobacteria are not always included in the biopsy specimen; nonspecific inflammation may be detected;
- X-ray of the lungs has been and remains the main method for diagnosing tuberculosis, regardless of its forms.
According to indications, other diagnostic methods can be used - ultrasound, CT, MRI, but they have an auxiliary value. The range of diagnostic tests depends on the clinical situation.
– chronic infectious disease caused by mycobacteria; characterized by the formation of specific granulomas in the intestinal wall with further melting of the focus, formation of a cavity and fibrosis during sanitation. The clinical picture is characterized by the absence of specific symptoms; typical pain syndrome, dyspeptic symptoms, intoxication. For diagnosis, an X-ray examination of the intestine, endoscopy with biopsy, tuberculin tests, ultrasound of the abdominal organs, and CT are performed. Therapy includes the use of tuberculostatic drugs; in the presence of complications, surgical treatment.
Pathological anatomy
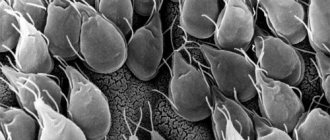
To recognize tuberculosis, examination of the mucous membrane is required. An endoscopic examination reveals hyperemia (redness), swelling, signs of hypertrophy (thickening and lumpiness), and ulcerative defects. The disease is indicated by the “niche” symptom, uneven contours, thickening of the folds and their smoothness. The intestinal lumen is reduced. With tuberculosis, healthy zones alternate with affected ones.
Important information: Features of the clinical development of renal tuberculosis in adults and children
Macroscopic changes

When examining an organ, the following may be determined:
- edema;
- thickening of the mucosa;
- pseudopolyps;
- ulcers;
- wall rigidity.
The defeat is not total, as in nonspecific ulcerative colitis.
Histological
A tissue biopsy is required to confirm the diagnosis. The material for research is fragments of the intestinal mucosa and submucosa. The main histological feature is the presence of a specific granuloma. It contains lymphocytes, epithelioid cells, multinucleated cells and Pirogov-Langhans cells. In severe cases, areas of caseous necrosis are found.
Symptoms
The peculiarity of the disease is the absence of any specific clinical manifestations that would accurately indicate the course of intestinal tuberculosis.
In some cases, the pathological process is asymptomatic: the diagnosis is made completely by accident during a routine examination in a medical institution or during the diagnosis of a completely different disease.
It is noteworthy that the first signs may appear a long period of time after infection. This period can vary from 1 year to 15 years.
The severity of symptoms is influenced by the following factors:
- stage of occurrence;
- prevalence of granulomatous intestinal lesions;
- localization of pathological changes.
Intestinal tuberculosis has the following clinical signs:
- pain in the abdominal area that does not have a clear localization - the intensity of pain gradually increases;
- alternating constipation and diarrhea;
- nausea without vomiting;
- general weakness and malaise;
- slight increase in temperature indicators;
- weight loss with normal appetite;
- unpleasant taste in the mouth;
- rumbling and heaviness in the intestines;
- increased sweating;
- hyperhidrosis.
It is advisable to apply clinical manifestations to both adult patients and children. The only difference may be the severity of symptoms.
Nutrition and diet
For this disease, it is recommended to eat foods that are easily digestible. Patients with intestinal tuberculosis are prescribed high-calorie foods:
- soups (low-fat);
- meat cutlets (beef, poultry, rabbit, chicken and turkey);
- fresh boiled fish;
- cottage cheese;
- scrambled eggs;
- omelette;
- butter;
- milk;
- kefir;
- porridge with milk (rice, oatmeal, semolina);
- fresh fruit juices;
The following should be excluded from the diet:
- pork;
- goose meat;
- lamb;
- smoked meats;
- legumes;
- canned food
Often, patients with intestinal tuberculosis experience digestive system disorders (diarrhea, nausea, vomiting, abdominal pain), but these symptoms may indicate not only this disease, so it is important to conduct a competent differential diagnosis. When using synthetic drugs, intestinal upset may also occur. This condition develops especially often during treatment with PASK.
We recommend reading: A baby has seborrheic dermatitis: how it manifests itself in newborns, at 1,2,3,5,8,9,10,12 years old, treatment
If a patient has severe diarrhea, the doctor must adjust his diet. The following foods are removed from the diet:
- black bread, white crackers;
- raw vegetables;
- fruits;
- restriction in meat consumption.
Patients should never self-medicate, as this can have a detrimental effect on their health.
A prerequisite for the development of a specific process in the intestine is the penetration of mycobacteria there, which is possible in several ways:
Additional therapies
Auxiliary methods of treating extrapulmonary tuberculosis include rest in a sanatorium, physiotherapy (ozone therapy), enhancing immunity and diet. If complications develop (bleeding, intestinal obstruction, fistulas, peritonitis), surgical intervention may be required.
Important information: Basic principles of treatment of spinal and bone tuberculosis in adults
Nutrition and diet for intestinal tuberculosis
When the body is exhausted, table No. 11 is indicated.
Patients need:
- give up spicy, coarse, fatty, smoked and fried foods;
- enrich the diet with meat, fresh fruits, berries and vegetables;
- eat 4-6 times a day;
- give up coffee, spices, processed foods, carbonated water and alcoholic drinks;
- eat steamed or boiled foods.

Patients with intestinal tuberculosis must adhere to a diet.
Diagnostics
Intestinal tuberculosis does not have specific or pronounced symptoms, so it is possible to make a correct diagnosis after the gastroenterologist studies the results of all laboratory and instrumental examinations and independently carries out a series of manipulations.
- study the medical history - to identify the most characteristic predisposing factor and confirm the occurrence of pulmonary tuberculosis;
- collect and analyze life history;
- carry out deep palpation and percussion of the anterior wall of the abdominal cavity;
- measure temperature indicators;
- interview the patient in detail - to determine the first time of onset and establish the intensity of clinical signs, which will clarify the nature and stage of the disease.
Laboratory studies are represented by the following tests:
- blood biochemistry;
- general clinical blood and urine tests;
- microscopic examination of feces;
- bacterial culture of blood, urine, prostate secretion, cerebrospinal and synovial fluid;
- specific tuberculosis tests;
- serological tests.
Instrumental diagnostics are limited to the following procedures:
- abdominal radiography;
- ultrasonography of the peritoneum;
- CT and MRI;
- colonoscopy;
- irrigoscopy;
- endoscopic biopsy;
- lumbar puncture;
- diagnostic laparoscopy.
Tuberculosis of the intestinal peritoneum and mesenteric lymph nodes must be differentiated from the following pathologies:
- inflammatory lesion of the appendix;
- intestinal amyloidosis;
- Crohn's disease;
- nonspecific ulcerative colitis;
- malignant neoplasms of the intestine.
Treatment
At the present stage, treatment of tuberculosis is quite effective. Typically, treatment of intestinal tuberculosis is carried out inpatiently in specialized dispensaries. First of all, the patient is prescribed drugs for tuberculosis. If they are not effective enough, chemotherapy is given.
If the disease is detected at a late stage or it does not respond to conservative treatment, surgery may be performed.
Timely consultation with a doctor and compliance with all his recommendations is extremely important. Intestinal tuberculosis is a dangerous disease that threatens a large number of complications.
Forecast
In general, with timely and competent treatment, the prognosis for this disease can be called favorable. If the patient strictly follows the doctor’s recommendations and does not miss taking medications, then recovery occurs in the vast majority of cases, even without surgical intervention.
On the other hand, if the patient neglects the doctor’s recommendations, skips taking the drug or voluntarily cancels it due to side effects, or if treatment is not carried out at all, then the likelihood of death is quite high. It can occur as a result of peritonitis, blood poisoning, cachexia, etc.
Diagnostics
To make an accurate diagnosis, it is first necessary to examine the condition of the lungs. Often it is the localization of the disease in the lungs that causes intestinal infection. The doctor may also prescribe the following types of examination:
- X-ray examination of the abdominal area. Helps to study the condition of the lymph nodes and determine the appearance of changes in the cecum and other parts of the intestine.
- Colonoscopy also allows you to detect disorders of the intestinal mucosa and changes in relief.
- Histological examination allows to distinguish tuberculosis from amoebic dysentery.
- Endoscopic biopsy excludes the possibility of Crohn's disease.
Symptoms
Intestinal tuberculosis is caused by tuberculosis bacteria. If the primary form of the disease occurs, infection occurs in a lymphogenous manner, and the secondary form appears due to sputum spreading in a sputogenic manner. According to the symptoms, tuberculosis of the intestine is often confused with ulcerative colitis, a pathology that is expressed in changes in the ileocecal region.
The main signs of intestinal tuberculosis include:
- Ulcers are erosive lesions of the intestinal mucosa.
- Presence of infiltrates.
- Colonization of the intestines, tubercles and irregularities on its surface.
Outwardly, these signs are invisible, so diagnosing intestinal tuberculosis can be very difficult. The presence of the disease can be suspected based on the following patient complaints:
- Frequent constipation or diarrhea.
- Abdominal pain, the localization of which cannot be determined.
- On palpation you can notice compactions.
- During periods of exacerbation, bloating is observed.
- Vomiting and nausea are common.
- There are traces of blood in the stool.
Less commonly, the disease develops on its own - in this case, it is much more difficult to identify it.
Preventive actions
A specific preventive measure is timely immunization with the BCG or BCG-m vaccine in childhood. To prevent secondary intestinal tuberculosis, it is recommended to promptly and correctly treat the underlying disease (primary forms).
Nonspecific preventive measures include:
- increasing immunity (giving up cigarettes and alcohol, eating well, playing sports, hardening);
- eliminating stress;
- taking vitamins;
- limiting contact with patients;
- washing hands before eating;
- boiling water and thoroughly cooking the meat.
These measures reduce the likelihood of developing infection and alleviate the course of the disease.
Diagnostics
A branch of medicine has been formed - phthisiology. Antibiotics do not work well against infections that quickly develop resistance. The doctor does not know how to treat intestinal tuberculosis. If I had known, I would have been left without a job - mycobacteria grow slowly. Doctors get sick 5-10 times more often. Some do not go to the hospital - they are treated in their own hospital.
In diagnosis, the main role is played by visual examination and tissue biopsy. The appearance of the affected area tells the researcher little. Numerous ulcers are recorded, often round in shape, up to 2 cm in size, leaving scars upon healing. The passage resembles an hourglass in longitudinal section, sharply narrowing at the site of the defect. With erosion, tissue destruction is deep, reaching perforation. This results in peritonitis. The signs are clear.
Blood tests rarely reveal abnormalities. During exacerbation, the level of ESR (erythrocyte sedimentation rate) increases. Types of laboratory tests used by doctors:
- Gastroduodenoscopy with examination of the duodenum.
- Colonoscopy is an examination of the colon through the anus with an endoscope.
It is important to take a biopsy of the affected area to make a diagnosis if pulmonary tuberculosis is not detected. Then the doctor will have a starting point for moving in the right direction. He will be aware of the presence of mycobacteria in the body and will see the discrepancy between ulcers and acute intestinal infections. There is no doubt about the cause - tuberculosis.
An endoscope and x-ray are used to make a diagnosis. When the small intestine is damaged, a characteristic picture is observed:
- uneven thickening of loops;
- uneven filling caused by partial obstruction.
Intestinal tuberculosis occurs more often than it is diagnosed. The disease is confused with:
- Ulcer.
- Chronic enteritis.
- Crohn's disease.
In intestinal tuberculosis with granulomatosis and ulcers, growths of connective tissue occur. The picture is varied: a perforation and adhesions of the lumen are found. Strictures interfere with intestinal patency
Clinical picture
The appearance of the contaminated surface often contains marks of other diseases. Diagnosis is difficult. There are no external clinical signs at the first stage. Phenomena accompanying intoxication:
- Abdominal pain. Gradually the localization moves to the right iliac region.
- Nausea to the point of vomiting during exacerbation.
- Impaired intestinal motility is manifested by constipation and diarrhea.
- In case of exacerbation - bloating, spasticity in the ileal loop. The abdomen is soft and painful to the touch.
- When the cecum is affected, pain and compaction are recorded upon palpation.
The ileocecal region is most often affected, including the cecum and terminal ileum. Typical signs of dyspepsia:
- Lack of appetite.
- Heaviness after eating.
- Weakness.
- General malaise.
- Sweating.
- Lesions of the rectum lead to the occurrence of tenesmus (false urge to defecate).
The intestinal wall seals are painful and can be felt upon palpation.
In 1862, Villemain anticipated Robert Koch's discovery by 20 years. He argued: tuberculosis is caused by a specific virus. Transmitted from humans to animals. Robert Koch added a description of the mycobacterium, erroneously claiming that infected cows were harmless. Bering (the author of the anti-tetanus serum) stated: the infection enters the intestines with milk. Intestinal tuberculosis is an inflammatory disease caused by the entry of the corresponding microbe (Mycobacterium tuberculosis complex) into the gastrointestinal tract.
We recommend reading: Bifidumbacterin: indications for taking the medicine, dosage and contraindications, instructions for use
The difficulty is making a diagnosis. There are no external symptoms of intestinal tuberculosis. Abdominal pain gradually appears, localized in the right iliac region. The treatment of intestinal tuberculosis looks more complicated - it is not effective. The “beauty” of the Gulag: a prisoner sat for a long time and came out sick. It is impossible to detect the first signs of intestinal tuberculosis - they are not there. The ileocecal region is most often affected.
The mechanism of spread of tuberculosis
Intestinal tuberculosis develops rarely, as a consequence of pulmonary disease. Schemes of development of the pathological process:
- The patient swallows his own sputum containing the pathogen. Mycobacterium enters the intestines. Here it is introduced into the mucous membrane, which is facilitated by sluggish diseases and acute inflammatory processes.
- Infection due to causes of local lymph nodes (usually mesenteric).
- The infection is brought by blood or lymph from other areas of the body.
Having a disease is not easy. Diagnosis and treatment of intestinal tuberculosis are more difficult. Scientific classification of cases:
- Primary intestinal tuberculosis complex.
- Secondary, formed from pulmonary tuberculosis.
- Hematogenous extrapulmonary tuberculosis.
- Abdominal pain. Gradually the localization moves to the right iliac region.
- Nausea to the point of vomiting during exacerbation.
- Impaired intestinal motility is manifested by constipation and diarrhea.
- In case of exacerbation - bloating, spasticity in the ileal loop. The abdomen is soft and painful to the touch.
- When the cecum is affected, pain and compaction are recorded upon palpation.
Causes and risk groups
Why does peritoneal tuberculosis develop? As mentioned above, most often it is of a secondary nature. What does this mean? With the development of a pathological tuberculosis process, for example, in the lungs, a fairly large number of bacteria that cause the disease spread throughout the body through the bloodstream and lymph flow. They can accumulate in various organs, systems and tissues.
When a sufficient number of such bacteria accumulates in an organ (and in the presence of some other aggravating factors), a tuberculous process may develop in it. When it comes to the peritoneum, lymph flow does not play any role and bacteria enter it through the bloodstream (however, lymph flow can cause damage to mesenteric lymph nodes located nearby).
The primary development of pathology is spoken of when other forms of the disease are absent in the body, and damage to the peritoneum develops immediately after the initial entry of the pathogenic bacterium into the body.
As is clear from what is written above, abdominal tuberculosis most often develops in people infected with pulmonary tuberculosis. However, not every such patient undergoes a similar process, since for this there must be some other predisposing factors:
- Reduced immunity, immunodeficiency states (both general immunity and local immunity);
- Severe exhaustion of the body;
- Improper, unbalanced diet;
- Strong physical activity;
- Difficult or unsuitable living conditions.
Failure to vaccinate against infection with the BCG vaccine significantly increases the likelihood of contracting primary peritoneal tuberculosis.
Reasons for the problem
There are certain causes of abdominal tuberculosis that are directly related to the routes of infection:
- First, the tubercle bacilli can enter the gastrointestinal tract through contaminated milk or saliva. The first to be affected is the intestinal mucosa with the formation of epithelioid tubercles in the lymphoid tissue of the submucosa. After 2-4 weeks, caseous necrosis of the tubercles leads to ulceration of the overlying mucosal tissue. Subsequently, the infection can spread to deeper layers, lymph nodes and mesentery. Less commonly, rods can penetrate the portal bloodstream or hepatic artery, involving the liver, pancreas and spleen in the pathological process.
- The second pathway involves the transport of microorganisms from another site somewhere in the body to the internal parenchymal organs, kidneys, lymph nodes and mesentery.
- Thirdly, the infection can spread by contact from nearby foci: fallopian tubes, appendages and abscess of the lumbar muscle (with tuberculous spondylitis).
- The latter route involves lymphatic vessels through which the rods migrate from infected nodes.
Symptoms of gastric tuberculosis.
There are no pathognomonic symptoms of gastric tuberculosis, but each of the two forms has significant features. In the ulcerative form of gastric tuberculosis, the clinical picture may resemble gastritis or peptic ulcer disease. At the same time, patients with this form experience a large number of symptoms characteristic of tuberculosis of the lungs and other organs. Complications such as perforation or bleeding are rare. Apparently, such complications are observed in patients with combined tuberculosis and peptic ulcer disease. Often patients with gastric tuberculosis are bothered by diarrhea, which is mostly associated with simultaneous specific damage to the intestines, moderate hypochromic anemia, increased temperature and ESR.
Tracheal and bronchial tuberculosis
These diseases individually occur extremely rarely, since they are complications of other forms of tuberculosis processes. In particularly difficult cases, tuberculosis can be detected using CT, but usually this requires a series of additional studies (bronchoscopy, microscopic analysis of the materials taken).
General concept of intestinal tuberculosis
Intestinal tuberculosis refers to extrapulmonary forms of the disease. It can be primary (due to infection with mycobacteria through food) and secondary (due to lung damage).
There has been an increase in the number of patients with this form of tuberculosis. At the same time, the poor clinical picture often complicates diagnosis and treatment.
Reasons for appearance
The cause of intestinal damage is the penetration of mycobacteria into the body.
These microorganisms have the following characteristics:
- belong to intracellular parasites;
- remain in tissues for a long time;
- capable of forming L-forms;
- have high stability in the external environment;
- have developed resistance to many drugs;
- have a rod-shaped shape;
- resistant to alkalis, acids and drying;
- multiply outside and inside cells;
- cannot move independently;
- have dimensions of 1-10 microns;
- capable of changing their morphology and genotype;
- are highly pathogenic;
- produce toxins (cord factor).
The risk of developing the disease is higher in physically weakened individuals, the elderly and children.
Predisposing factors are:
- the presence of foci of chronic infection (pyelonephritis, hepatitis, chlamydia);
- oncological pathology;
- recent radiation exposure;
- chemotherapy;
- primary immunodeficiency;
- hypovitaminosis;
- poor nutrition (lack of animal protein, vegetables, berries and fruits);
- smoking;
- alcoholism;
- poor living conditions (high humidity, low temperature);
- frequent acute respiratory diseases;
- untimely or irrational treatment of pulmonary tuberculosis;
- contact with or living with sources of infection;
- inactive lifestyle;
- taking drugs that suppress the immune system (corticosteroids, cytostatics);
- insufficient sleep;
- stress;
- endocrine pathology;
- stay in places of deprivation of liberty.

An inactive lifestyle is a predisposing factor to the development of the disease.
Contagious or not: transmission routes
The following mechanisms of tuberculosis infection are distinguished:
- aerogenic (through the air, when the pathogen spreads with microparticles of sputum when sneezing and coughing);
- contact (through dirty hands and objects);
- vertical (from sick mother to child);
- fecal-oral (through the mouth).
The primary form of the disease develops after the first contact with mycobacteria. Infection occurs through food. Transmission factors can be dirty hands, milk from sick animals, contaminated food, dishes, or toothbrushes of a sick person.
A person ingests bacteria. They enter the oral cavity, esophagus, stomach and intestines. Hydrochloric acid does not affect them, so bacteria easily penetrate into the lower gastrointestinal tract, and then into the mucous membrane and cells.
The secondary form occurs against the background of a primary tuberculosis complex, damage to the intrathoracic lymph nodes and tuberculosis intoxication if they are not treated in a timely manner. In this case, mycobacteria enter the intestine by hematogenous (through the blood), lymphogenous (through lymphatic vessels) and deglutation (by ingesting one’s own sputum with microbes) methods.
Important information: Clinical picture of fibrous-cavernous pulmonary tuberculosis