General rules of diet for intestinal colitis
Ulcerative colitis is a disease that affects the lining of the colon. The disorder manifests itself as destructive-ulcerative inflammation of varying intensity. The lesion begins in the rectum and gradually spreads or immediately affects the rest of the colon. The disease is also called ulcerative colitis.
First of all, doctors exclude foods that irritate the mucous membrane of the digestive organs.
Table 4 - diet for intestinal colitis
Patients are recommended to follow a gentle diet that meets the following requirements:
- inclusion of high-protein foods in the menu;
- eliminating coarse fiber from the diet: unprocessed berries, fruits, raw vegetables, nuts, seeds, sesame, bran, legumes;
- food should be boiled or steamed;
- warm food is rubbed or boiled vegetables are grated on a coarse grater;
- exclusion of chemical irritants to the mucous membrane (spicy, salty, pickled, sour foods);
- It is permissible to add butter to dishes, no more than 10 g;
- Porridge should be cooked in water.
Features and types of colitis
Colitis is an inflammatory disease of the colon with a tendency to quickly transform into a chronic form and spread throughout all parts of the intestine. The main causes of inflammation are traumatic factors of any nature, hereditary predisposition and the influence of other external or internal factors. Based on the nature of occurrence, the following types of colitis are conventionally distinguished:
- toxic (pathogenesis is caused by intoxication with alcohol, poisons, drugs);
- ischemic (caused by impaired blood circulation in the mucous and submucosal structures of the intestine, their necrosis);
- spastic (occurs with a persistent stress factor, increased psycho-emotional stress, often appears in teenage children);
- infectious (the pathological process is caused by a violation of the intestinal microflora, the development of an infectious process);
- atonic (the nature of its occurrence is associated with impaired intestinal motility, with a decrease in muscle tone of submucosal structures);
- allergic (intestinal reaction to an unfavorable allergic background);
- nutritional (excessive amounts of fried and fatty foods, overeating along with fasting).
According to the nature of the course, erosive, ulcerative, pseudomembranous, and atrophic colitis are distinguished. The classification of intestinal colitis is determined by multiple criteria, so dietary principles may vary. The disease often occurs in women.
Important! The diversity of the pathological process is also determined by the structural changes in the mucous membranes, so nutrition for each patient with colitis may be different.
What should you consider when creating a menu?
A diet for colitis should be balanced, including fruits, vegetables, grains, dairy products and proteins. It is necessary to include some healthy fats such as olive oil in your diet.
There is no single diet plan that works for all types of colitis.
It is not uncommon to have problems with foods that a person previously tolerated and then, after eating them, develop stomach problems. It is necessary to remove from the diet foods that irritate the mucous membranes and cause increased gas formation. Cooked foods should be digested easily and without difficulty.
Diet
Instead of several large meals, the eating regimen should be divided into 5-6 small meals, which will give the intestines time to digest the food.
Food temperature
Meals 1 and 2 should be warm, drinks should also not be consumed cold.
Cooking
A diet for colitis is light in all respects.
To do this, there are certain ways to process products:
- steam cooking;
- stewing;
- boiling;
- languor;
- cooking in foil, special baking bags.
The best result is achieved if dishes are cooked in a double boiler or multicooker. If it is not possible to chew food thoroughly, the food should be pre-chopped.
Plant fiber
Fiber-rich foods such as grains, vegetables and fruits are an important part of a balanced diet, but consuming too much of them can impair bowel function.

It's best to discuss the amount of fiber you consume with your doctor, and changing the way you prepare fruits and vegetables can also make them easier to digest.
Salt
Some medications used to treat ulcerative colitis cause side effects if too much sodium is consumed. For example, they can cause swelling and bloating in the abdomen. Therefore, you should follow a low-salt diet to prevent water retention.
Free liquid
People with conditions such as ulcerative colitis may need to drink more fluids, as diarrhea often leads to dehydration.
Alcohol
It has been found that alcohol increases inflammatory reactions in the intestines and worsens the symptoms of the disease.
Doctors have found that after one week of alcohol consumption, protective barriers in the intestines are reduced and intestinal permeability increases, which leads to a worsening of ulcerative colitis. It's best to avoid drinking alcohol whenever possible and limit your intake when drinking.
Reviews and results
The existing restrictions are minor, so this therapeutic diet is easily tolerated and is simply necessary for combined gastrointestinal pathology. A balanced diet allows you to constantly follow it, which prevents the occurrence of exacerbations. Judging by the reviews, this diet allows you to eliminate discomfort in the stomach, belching, bloating and normalize its function.
- “... The diet is easy and healthy, so I always stick to it. I have irritable bowel syndrome and, although there are no changes in the mucous membrane, I still complain about pain, bloating, and rumbling. Constipation may alternate with diarrhea. All this forces you to constantly monitor your diet. Too much vegetables is accompanied by diarrhea, if you eat more baked goods and pasta - constipation. It all started with gastritis, and then problems with the intestines appeared. Over the years I have studied the body and I cannot leave the diet, as it will worsen or even worsen. I selectively eat fruits and juices, and very rarely allow sweets and a little marshmallow or marmalade. And everyday food consists of soups, boiled chicken and fish.”
- “...Nonspecific ulcerative colitis is a rather serious disease, plus gastritis. So diet for me is a way to feel relatively good. I already know what needs to be excluded so that there is no exacerbation. I periodically conduct courses of treatment - it’s impossible without it. It's not difficult to cook if you have a steamer. I immediately make vegetables and cutlets in it. Then I beat the vegetables until pureed and dilute them with a decoction of vegetables. I can’t stand milk, but I can drink kefir. Cafe food is not for the sick, so I gave it up a long time ago. I also have to take dietary meals to work”;
- “... Colitis and gastritis worsen in turn. My stomach starts to ache after fried foods and spices, and my intestines start to ache after cabbage (I can’t even eat borscht), nuts and seeds. I know this, but sometimes I want it so much that I can’t resist a handful of seeds. It turns out to be enough to cause pain in the intestines and colic. When everything gets worse, I start to eat right, but I still can’t prevent it. Dishes cooked in a double boiler and baked are used. During this period, I refuse fresh and pickled vegetables, do not eat anything fried, fatty, or with spices. After ten days it gets better: the belching disappears, the pain in the stomach subsides, there is no bloating, and the stool becomes softer. I bake fish or meat with vegetables in a slow cooker - all without oil. Then I make bechamel sauce (I really love it) and it improves the taste of the vegetables. I cook soups in water or very weak broth. In general, you can adapt and the food does not seem boring and monotonous.”
Authorized Products
People with ulcerative colitis should eat foods that provide significant amounts of:
- potassium;
- folate;
- magnesium;
- calcium;
- gland.
Good menus for ulcerative colitis are foods that can provide all the nutrients the body needs without wreaking havoc on the gastrointestinal tract.
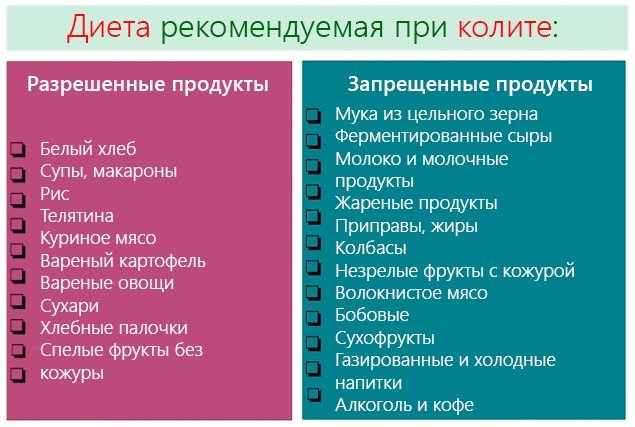
The main thing in the treatment of chronic colitis is diet
Some of the best foods for ulcerative colitis include:
- Yesterday's bread made from wheat flour.
- Soups with secondary broth from chicken, turkey, rabbit, vegetable broths.
- The meat is lean.
- Boiled ham, milk sausages.
- Lean fish.
- Dairy products: sour cream, cottage cheese, yogurt, cream, fermented baked milk, skim milk.
- Eggs in the form of omelets, soft-boiled, no more than 3 per week.
- Porridge on water: rice, buckwheat, oatmeal, rolled oatmeal.
- Applesauce is a good source of nutrients. However, the high fiber and fructose content in applesauce can make it difficult to digest during a flare-up of symptoms.
- Pumpkin, zucchini. Some high fiber vegetables are not suitable for people during relapses of the disease.
- Refined grain. It is better to eat pasta, bread and cereals made from refined grains. Whole grains are more difficult to digest.
- Sweet fruits without peel in puree form.
- Marshmallows, marshmallows, marmalade.
- Weak tea, preferably with milk, herbal decoctions, berry juices diluted 1/1, compotes, jelly, mousses, jellies.
Symptoms for prescribing a diet
The diet is prescribed for the following signs and symptoms:
- Pain appears after eating in the stomach or hypochondrium.
- An unpleasant taste may appear in your mouth.
- Heartburn occurs, which may be accompanied by sour belching.
- Feeling of fullness in the stomach.
- The occurrence of constipation.
- Poor appetite.
During the period of exacerbation of chronic gastritis, the menu is more strict, and the diet itself is more gentle. During this period it is necessary:
- eat foods that are easily digestible in small quantities;
- reduce the volume of liquid consumed to 1500 ml.
Doctors recommend sticking to a diet that is determined by the diet of the first table. It is characterized by the fact that mainly grated products are used for food. Fried foods are completely excluded. Before going to bed, you should drink milk. The number of calories consumed during the day should not exceed three thousand.
Partially restricted and prohibited products
Medical professionals recognize certain foods as potentially dangerous for ulcerative colitis:
- Caffeine.
- Sour dairy products.
- Carbonated drinks.
- Foods high in fiber. These include dried beans, fruits, whole grains, berries, peas and legumes. They increase the frequency of gastric emptying, the amount of gas, and abdominal cramps.
- Potato. This vegetable contains glycoalkaloids, which can disrupt the integrity of the intestinal cell membrane.
- Products that contain sulfur or sulfites. This mineral promotes excess gas formation. It is found in beer, wine, almonds, soy, wheat pasta, bread, peanuts, raisins and sausages.
- Fat meat. During an outbreak, the intestines may not fully absorb fat from meat, making negative symptoms worse.
- Nuts, nut butters and seeds. These foods cause abdominal cramps, bloating, and diarrhea.
- Sugar alcohols. They can cause bloating, diarrhea and gas, and are often used as a sweetener in chewing gum and sugar-free candy, some fruit juices and ice cream.
- Vegetables that contain a lot of fiber: celery, Brussels sprouts, broccoli.
- Spicy foods. These include hot sauces and pepper.
- Gluten. It is a component of wheat, rye and barley. It sometimes causes symptoms of ulcerative colitis.

To improve intestinal function, you should increase the amount of foods containing:
- inulin – bananas, chicory, Jerusalem artichoke:
- Oligofructose is a prebiotic often added to foods.
Diet menu according to disease types
Diet, as one of the components of the course of treatment for colitis, reduces inflammation, fermentation and putrefactive processes in the intestines. It is better to cook porridge, vegetable, meat and fish dishes by steaming or in a double boiler.
For chronic colitis with constipation
It is recommended to eat at least 5 times a day. Dishes should be liquid and ground; porridges should be cooked halfway with water.
Menu for 1 day:
| Breakfast | Hercules porridge, cocoa on water |
| 2 breakfast | Soft cheese |
| Dinner | Cereal soup with chicken broth, boiled chicken meatballs, rosehip infusion |
| Dinner | Grated and boiled vegetables |
| Afternoon snack | Unsweetened cookies, kefir |
If you have colitis with constipation, you should limit the amount of salt. It is permissible to consume no more than 10-15 g per day. Fruits and vegetables rich in fiber should be consumed boiled.
For chronic colitis with diarrhea
Various types of boiled lean fish are useful. The best meats to use are veal and chicken.

| Breakfast | 1 soft-boiled egg, 1 slice wheat bread, tea |
| Snack | Baked green peas, cocoa water |
| Dinner | Boiled bream, grated, boiled zucchini |
| Afternoon snack | Marshmallow |
| Dinner | Steamed chicken with pumpkin pieces |
| Snack | Rose hip jelly |
A diet for colitis to restore intestinal function must be followed for at least 1 year. During the period of remission, soups with meat broth and raw vegetables are allowed.
With exacerbation of chronic colitis
Exacerbation of the disease requires a more stringent approach to the choice of products:
| Breakfast | Oatmeal with water, slimy, tea |
| Breakfast 2 | Kissel |
| Dinner | Lean meat broth, diluted, rice porridge on water, slimy, crackers |
| Afternoon snack | Steamed carrot-apple soufflé |
| Dinner | Steamed fish cutlets, lean |
| Snack | Curdled milk |
You can add lean skinless chicken to the menu. It is better to cook porridge in a double boiler. Use unleavened cottage cheese, fruit jelly, and cook cocoa in water.
With ulcerative form
This form of the disease is autoimmune in nature. When dieting, special attention should be paid to foods containing proteins.
| Breakfast | Rice porridge with water, bird cherry infusion |
| 2 breakfast | Fruit puree from pears |
| Dinner | Fish with white sauce, fish broth, peeled, peach compote |
| Afternoon snack | Fruit jelly, biscuits
|
| Dinner | Carrot pudding |
The last meal should be no later than 19:00. You can add butter to prepared dishes, no more than 10 g per day.
In spastic form
Spastic colitis is a disorder of the intestines, which is manifested by abdominal pain and alternately constipation and diarrhea.
The diet for colitis, especially spastic one, includes a variety of foods with a lot of fiber, which is necessary for constant constipation. For adult patients, fasting is recommended for the first 2 days after the onset of an exacerbation.
In the following days, you should drink 1 glass of warm water in the morning, it is preferable to eat oatmeal for breakfast, and if loose stools bother you, then cook rice porridge. Vegetable soups should be prepared for dinner. In the following days, you can gradually add fish, boiled meat, and eggs.
| Breakfast | 1 glass of clean warm water, 25 g of probiotic yogurt |
| Snack | 1 banana |
| Dinner | 1 glass of warm water, baked fish with raw salad |
| Snack | Fruit juice without pulp |
| Dinner | 1 glass of water, boiled zucchini, grated vegetable soup |
| Snack | Yogurt |
To avoid dehydration, you should drink at least 8 glasses of warm water per day. During exacerbations, you should eat stewed vegetables, and then, as symptoms subside, raw vegetables and fruits, peeled, are added to the diet.
With catarrhal form
A diet for this type of colitis involves fasting for the first 2 days after the onset of an exacerbation. You can drink tea, rosehip decoction, mineral water. More dishes will be added in the future.
| Breakfast | Steamed omelette
|
| 2 breakfast | Fresh pear jelly |
| Dinner | Fresh cabbage soup, crackers, fish dumplings |
| Afternoon snack | Peach compote, biscuits |
| Dinner | Applesauce with lemon juice |
The diet should be aimed at protecting the mucous membrane and reducing the acidity of gastric juice.
In the atrophic form
The daily diet for this type of diet should include at least 100 g of protein, 100 g of fat and 60 g of carbohydrates.
| Breakfast | Apple puree |
| 2 breakfast | Hercules on water, pear compote without sugar |
| Dinner | Fresh cabbage soup, 1 piece wheat bread, boiled meat with porridge on water |
| Afternoon snack | Apple marshmallow |
| Dinner | Zucchini with kefir |
Meals should be intermittent, in small portions, without coarse fiber.
For erosive colitis
The menu should contain an increased amount of protein foods. Milk is contraindicated for this form of colitis.
| breakfast | Semolina porridge with water, weak tea |
| 2 breakfast | Rosehip decoction, crackers |
| Dinner | Bean pod puree soup, low-fat cottage cheese dumplings, rosehip juice |
| Afternoon snack | Curdled milk jelly |
| Dinner | Carrot and fish stew |
For erosive colitis, doctors recommend boiled meat, white, stale bread, grated fruit, without skin.
For pseudomembranous colitis
This type of colitis is caused by an imbalance of bacteria in the colon.
Main symptoms:
- frequent watery diarrhea;
- lack of appetite;
- nausea;
- pain and tension in the abdominal area.
The diet for pseudomembranous colitis involves increased protein intake and reduced fat intake. Vegetables can only be eaten boiled, fruits should be baked, and fruit juices should be diluted with water.
| Breakfast | Oatmeal with water, dry wheat bread |
| Snack | Cottage cheese
|
| Dinner | Steamed beef, meat broth diluted with water, rose hip decoction |
| Afternoon snack | Blueberry decoction, dry bread |
| Dinner | Grated boiled vegetables, steamed chicken |
| Snack | Ryazhenka |
Plenty of water, especially with added sodium and potassium, and diluted juices will help cleanse the system. Compliance with daily hygiene procedures will help get rid of the further spread of Clostridium difficile bacteria, clostridia, which are responsible for the development of this form of colitis.
With combined colitis with enterocolitis
The diet should be selected by a doctor taking into account the severity of the inflammatory process. The combination of colitis and enterocolitis can enhance the fermentation process in the intestines. Diet No. 4 according to Pevzner is prescribed.
Sample menu for 1 day:
| Breakfast | Steamed omelette of 2 eggs, crackers |
| 2 breakfast | Mashed cottage cheese, blackcurrant decoction |
| Dinner | Chicken meatballs, lean beef, pureed boiled vegetables |
| Afternoon snack | Bird cherry jelly |
| Dinner | Slimy rice soup, tea without milk |
| Snack | Rosehip decoction, stale bread |
You can add meat dishes to the menu in the form of meatballs and quenelles. Semolina and oatmeal soups will also be useful. In the acute stage, diet 4a is recommended.
With combined gastritis and colitis
The combination of 2 types of diseases requires the use of the Pevzner menu, table No. 2.
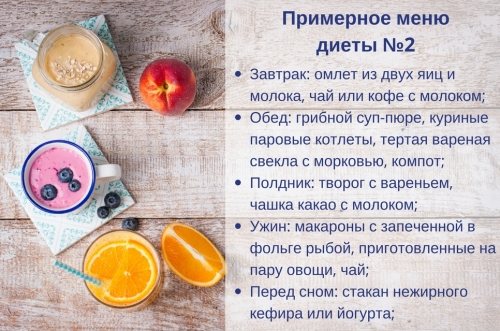
| Breakfast | 1 soft-boiled egg, cocoa |
| 2 breakfast | Tea, dried bread, butter 5 g |
| Dinner | Vegetable puree soup, fried fish (without breading) |
| Afternoon snack | Fruit jelly |
| Dinner | Boiled beets, grated, with added cream, dried bun |
| Snack | Curdled milk |
During the period of remission, you can consume cocoa, yogurt, milk, fish dishes, and low-fat chopped herring. Various jellies, mousses, grated fruits, compotes, jelly, and fish sauces will be useful.
For childhood colitis
In case of illness, all foods that increase fermentation in the intestines are excluded.
| Breakfast | Omelet in a water bath, baked apple |
| 2 breakfast | Milk tea, biscuits |
| Dinner | Vegetable puree soup, steamed meat soufflé, cranberry drink |
| Afternoon snack | Pear puree |
| Dinner | Curd pudding |
| Before bedtime | Kefir or blueberry jelly |
As for fruits, the child is recommended to eat apples, blueberries and pears. Milk, soups with cereals are excluded, pasta is prohibited.
What you can't eat
If you have colitis, you need to be very selective when choosing foods to eat, and some should be avoided.

Floury . All baked goods put a strain on the intestines, so you should avoid them.
Soups . Fatty broth is prohibited. Soups containing large quantities of cereals, pasta and meat are not welcome.
Meat and fish . Fatty meats are excluded immediately, this also applies to all semi-finished products.
Milk products . Milk, cottage cheese and other products, except kefir and fermented baked milk, are excluded from the diet.
Cereals . Avoid legumes, pearl barley and millet. You should forget about pasta.
Canned food . Canned vegetables, fruits and other foods can have a detrimental effect on the patient's health.
They should be administered only after the patient has recovered.
Beverages . It is unacceptable to drink coffee if you have colitis. Carbonated drinks can also cause harm to the body.
Fats . Avoid any fatty foods. The only exception is butter in small quantities.
Do you know the benefits of mustard oil for the body? We will tell you a lot of useful and interesting things!
Read about the benefits of tea with ginger and lemon in our publication.
And here we describe in detail an easy diet for quickly losing weight on your stomach and sides. Effective weight loss to you!
Sample menu for a week during an exacerbation period
This diet helps during periods of exacerbation of ulcerative colitis symptoms.
Day 1:
- Breakfast: 1 glass of clean warm water, 25 g of low-fat yogurt, 1 banana.
- Lunch: 1 glass of water, baked salmon with grated vegetable salad.
- Snack: fruit juices without pulp.
- Dinner: 1 glass of water, omelette with vegetables.
Continue to drink water over the next days before breakfast, lunch and dinner.
Day 2:
- Breakfast: 1 soft-boiled egg.
- Lunch: boiled skinless chicken with green beans.
- Snack: 3 bananas.
- Dinner: white rice porridge with water.
Day 3:
- Breakfast: fruit smoothie with bananas.
- Lunch: oatmeal soup, chicken soufflé.
- Snack: yogurt with chopped fruit.
- Dinner: boiled zucchini.
Day 4:
- Breakfast: banana and avocado smoothie.
- Lunch: carrot soup with cornbread.
- Snack: canned fruit.
- Dinner: brown rice, vegetable salad with feta cheese.
Day 5:
- Breakfast: steam omelette with 1 wheat cracker.
- Lunch: pearl barley soup with vegetables.

- Snack: 5 plums.
- Dinner: baked potatoes, 2 cucumbers.
Day 6:
- Breakfast: blueberry or blackberry smoothie.
- Lunch: cauliflower soup, steamed salmon,
- Snack: 2 small pieces of watermelon.
- Dinner: pumpkin-apple pudding.
Day 7:
- Breakfast: several fresh apricots, a cup of tea with milk.
- Lunch: fish soup, vegetable puree.
- Snack: oatmeal jelly.
- Dinner: white rice with steamed cabbage.
Sample menu
In the first days of the disease, the following sample menu is offered:
- Breakfast: thin porridge cooked in water; tea with a little sugar and a couple of crackers.
- Lunch: one glass of jelly or fruit drink.
- Lunch: soup with weak broth; a piece of boiled meat with buckwheat; fruit compote
- Afternoon snack: egg white omelette; a decoction of medicinal herbs or rose hips.
- Dinner: vegetable stew with meatballs; slightly sweet tea.
It is recommended to follow a strict diet for several days. Next, jelly or tea can be replaced with a decoction of rice or raisins. After the first week of illness, the diet includes baked fruits, puddings, vegetable salads, and some dairy products.
Dietary nutrition for spastic colitis is the basis of non-drug treatment. Eating healthy food can help you get rid of troubling symptoms and promote a speedy recovery. But you need to know that this diet must be observed under the supervision of a specialist.
Recipes for dietary dishes and drinks
The choice of products should correspond to the severity of the disease. The phases of remission and exacerbation also affect the method of preparing dishes.
Zucchini soup
The dish is recommended for colitis with constipation.
Compound:
- zucchini – 500 g;
- butter 2 g;
- vegetable broth 3 cups;
- shallots 15 g;
- salt to taste;
- sour cream - 1 glass;
- lemon juice - 1 tsp.
Peel the zucchini and grate on a coarse grater. Melt the butter in a saucepan, boil the finely chopped onion for a little while. Add the zucchini and pour the broth over everything. Cook for 10-12 minutes. Place everything in a blender and mix. Mix sour cream with 1 tbsp. l. flour, add gradually to the soup, stirring until thickened. Add salt and lemon juice to the plate to taste.
Cabbage soup
For ulcerative colitis, you can prepare cabbage soup from fresh cabbage with fish.
Ingredients:
- fish (pike perch) – 500 g;
- cabbage (it is better to take Savoy or Peking cabbage) – 300 g;
- carrots – 1 pc.;
- olive oil – 3 g;
- water;
- salt;
- greens for decoration.

Place vegetables in a saucepan, add 3 liters of water, add salt and cook for 30-35 minutes. Place the fish, lightly stewed in oil, into the broth for 5 minutes. until the end. Season with spices. When serving, add sour cream and herbs.
Chicken soufflé
The dish can be prepared for any type of ulcerative colitis.
Compound:
- chicken meat, white - 200 g;
- milk sauce - 100 g;
- butter - 5 g;
- egg - 1 pc.;
- white cheese - 12 g;
- salt.
Boil the prepared chicken, mince it, add milk sauce and egg yolk. Mix everything. In 15 min. Before serving the dish, add the whipped egg white and transfer to a serving bowl. Bake in the oven, first sprinkled with grated cheese.
Fish in white sauce
For gastritis and colitis, you can include hake fish in your diet, serving it with white sauce. To do this, place the hake fillet in a wide pan greased with vegetable oil, add water and cook for 25 minutes. When the fish is ready, remove it from the broth and strain it.
For the sauce, take 300 ml of fish broth, cooled to 50°, add wheat flour (1-2 tbsp.) and quickly stir everything, add salt and butter, 5 g.

Place pieces of fish into the multicooker bowl, pour in the sauce, and cook in the “Stew” mode for about 20 minutes.
Steamed chicken dumplings
For colitis and enterocolitis, you can include this delicate dish in your diet. It contains: white chicken meat 500 g, crackers 50 g, butter 10 g, eggs 2 pcs., salt to taste.
Pass the fillet through a meat grinder, adding crackers soaked in water. Add salt, yolks, butter to the minced meat. Mix everything, and then add the beaten egg whites to the minced meat. Form balls from the resulting mass and steam or steam them in a double boiler.
Pike perch fillet in foil
For spastic colitis, you can add fish dishes to your diet. One of them is pike perch fillet. To do this, you need to take a cleaned and prepared fish carcass. Place finely chopped herbs inside the fish. Lay out the foil, sprinkle with vegetable oil, place the fish on it and wrap well. Bake in the oven for 30 minutes. at 200°C.
Blackcurrant jelly
For catarrhal colitis, you can include jelly in the menu; a drink made from black currant is especially useful.

Place berries (200 g), sugar (2-3 tbsp) in a saucepan, add water (2.5 l). Bring everything to a boil, boil for 5-10 minutes, and then strain. Dilute 45 g of starch with 50 ml of cold water and gradually add to the hot drink. Bring to a boil, stirring constantly.
Berry jelly
Berry jelly is recommended for various types of colitis. To prepare them, take 150-200 g of berries, 100 g of granulated sugar (less possible), 40 g of starch, 1 g of citric acid.
Place the washed berries in a saucepan, add water and cook until tender. Then strain the broth, add granulated sugar, and add citric acid. After 1 boil, add starch diluted in cold water. Bring everything to boiling point 2, but do not boil.
Peach compote
Peach compote can be offered to patients with ulcerative colitis, but it should be prepared without sugar. For 500 g of peeled peaches, add 2 liters of water, everything is brought to a boil. Cook for 12-15 minutes, and then let the drink brew. If a lot of pulp has formed in the compote, then it should be strained through cheesecloth.
Consequences of not following the diet
A small number of people with colitis may develop inflammation in other parts of the body, such as the liver, skin, joints and eyes. Regular monitoring by a gastroenterologist, as well as colonoscopy, will help prevent the development of complications.
But medications may be required, including steroids and medications designed to prevent inflammation, and sometimes surgery.
Cases of severe inflammation caused by ulcerative colitis if treatment and diets are not followed:
- nutritional deficiencies;
- severe bleeding due to deep ulcers;
- perforation (rupture) of the intestine;
- problems with the biliary tract affecting the liver;
- fulminant colitis and toxic megacolon are conditions in which the intestines stop working.
In the long term, the disease is associated with an increased risk of developing bowel cancer.
Death from ulcerative colitis is extremely rare. In most cases, the disease can be managed throughout life with diet, proper and timely treatment.
Author: Belyaeva Anna
Chronic atrophic gastritis
If the disease is in the stage of chronic atrophic gastritis, then a diet is prescribed that corresponds to treatment table No. 2. With this disease:
- the gastric mucosa becomes inflamed;
- atrophy of glandular cells occurs, which are replaced by intestinal-type epithelium.
Atrophic gastritis is manifested by the following symptoms:
- Severe abdominal pain appears.
- Frequent cases of constipation, as well as diarrhea, which can be chronic.
- Heartburn occurs.
- Sudden loss of appetite.
- A coating appears on the tongue, which has a yellow-gray color.













