Many patients want to know why hypofunction or hyperfunction of the pancreas occurs, whether it is possible to distinguish one from the other based on symptoms, and what can be done to prevent these pathologies. It is problematic that in the early stages of the development of these ailments, they manifest themselves as symptoms, often mistaken for ordinary fatigue or other “routine” ailments, and they begin to sound the alarm only when faced with an acute hypoglycemic state. Let’s look at why excessive function of the glandular organ occurs and what symptoms can be used to suggest its presence.
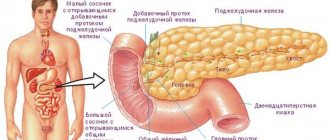
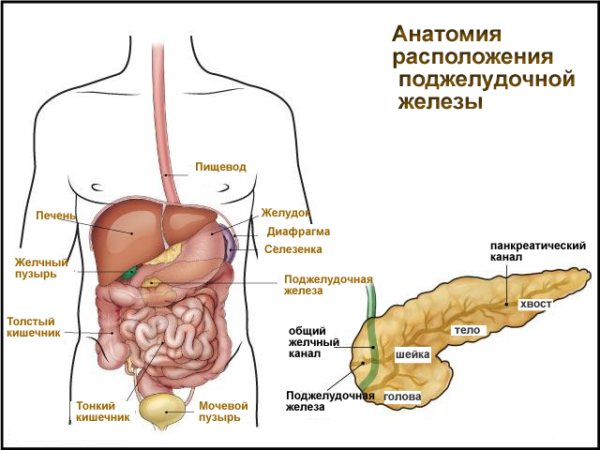
The structure of the pancreatic gland
Causes of pancreatic hyperfunction
The functions for which the pancreas is responsible are:
- The production of hormones on which the body’s absorption of carbohydrates – insulin, glucagon – depends;
- Production of gastric juice rich in enzyme compounds, without which proper digestion is impossible.
Let's consider the functions performed by hormones secreted by the gland:
- Glucagon is produced by alpha cells in areas called the islets of Langerhans. It sends a signal to liver cells to synthesize glucose or release glycogen from the liver. It also increases heart rate and blood pressure;
- Insulin is generated by beta cells to ensure the absorption of glucose by body tissues. Without it, high-quality nutrition of tissues and organs is impossible.
What happens when the gland over- or under-functions? When there is a deficiency in insulin production, the patient develops diabetes mellitus. With hyperfunction, the gland produces excessive amounts of hormones, and the patient develops a hypoglycemic state. With this pathology, so much insulin is produced that it blocks the production of glucagon, which is necessary for the production of glucose from glycogen in the liver.
Glucose deficiency is a significant problem for the body, especially for the brain, because it is the main source of nutrition. The pathology described more often occurs in women, this is due to the characteristics of their hormonal levels. Typically, the age of affected women is from thirty to fifty years.
Hyperfunction of the pancreas can occur due to the following phenomena:
- Incorrect diabetes therapy. Most often, taking excessive doses of insulin;
- Formation of insulinoma (this is a benign tumor of the gland that produces very high doses of insulin). It can form not only on the gland itself, but also on the areas of the digestive organs adjacent to it;
- The occurrence of glucagonoma (this tumor is localized on the islets of Langerhans and easily becomes malignant);
- The emergence of other neoplasms of any nature.
Any cause of pathology in a particular patient requires receiving qualified medical care as soon as possible. Since hyperfunction of this gland is fraught with a pronounced hypoglycemic state.
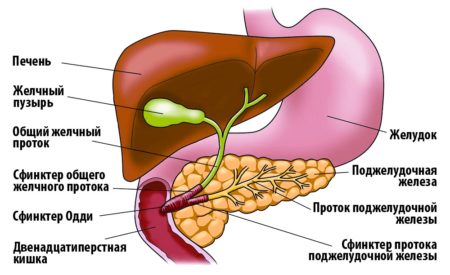
Place of the organ in the digestive system
Diabetes mellitus and pancreas
In diabetes mellitus, there is a gradual disruption of nutrition of all organs. Shifts in metabolic processes lead to cell atrophy, including in the pancreas. Against this background, all the substances that it produces reduce their concentration. Secondary damage to the organ occurs, and insulin secretion worsens. A vicious circle leads to worsening diabetes.
Sometimes pancreatitis develops regardless of the presence or absence of disruptions in sugar metabolism. But even in this case, treatment must restore the secretory function of the gland as soon as possible, otherwise progression of the process is inevitable.
Main harbingers
It can be determined that a patient is developing increased gland function by the following signs:
- Weakness, fatigue, decreased performance;
- Sharp weight gain without changing diet;
- Limb spasms;
- Drowsiness;
- Absent-mindedness, impaired concentration;
- Loss, confusion.
Many of these symptoms, especially if the person’s condition is not accompanied by disturbances of consciousness, are usually attributed to overwork and stress. Because of this, the patient may delay visiting the doctor.

To alleviate the disease, injectable glucagon is administered
Hypofunction
If the pancreas produces a reduced dose of insulin, diabetes mellitus develops. Hypofunction of the pancreas occurs as a result of destruction of the structure of the islets of Langerhans.
Risk factors include:
- hereditary predisposition;
- being overweight;
- frequent stressful situations and nervous tension.

Symptoms of hypofunction may vary. This depends on the individual characteristics of the person and the stage of development of the pathology. Most often, the following symptoms are observed with such diseases:
- dehydration of the body, accompanied by frequent feelings of thirst;
- dryness of the oral mucosa;
- frequent and copious urination;
- rapid weight loss;
- nausea and vomiting;
- pain in the abdominal area;
- disturbance of consciousness;
- increased fatigue.
To identify the disease, it is necessary to conduct a urine test for the amount of glucose. Treatment should begin immediately after testing. First of all, injections of artificial insulin are carried out. This is necessary in order to normalize glucose levels.
If digestive disorders, dizziness and chronic fatigue are added to other symptoms of the pathology, then there is a risk of developing a diabetic coma. If such signs are present, it is necessary to conduct blood tests for sugar levels and urine tests for the amount of acetone.
It is impossible to completely cure a disease of this nature, but with proper therapy it will be possible to significantly improve the patient’s quality of life.
Symptoms
The symptoms of this disease are closely related to hypoglycemic syndrome. When the disease worsens, it makes itself felt with the following clinical manifestations:
- Neurovegetative disorders - cardiac arrhythmia, redness of the facial skin, surges in blood pressure, profuse sweating;
- Problems concentrating in the morning;
- Psychomotor overexcitation and repetition of monotonous movements may also occur;
- Various types of disturbances of consciousness (in the most severe cases - coma);
- Retrograde amnesia.
During periods between exacerbations, the pathology manifests itself with the following symptoms:
- Neurological disorders - paralysis of the facial muscles, swallowing disorders, decreased sensitivity of the upper part of the pharynx, the appearance of pathological tendon reflexes, impaired sense of taste;
- Degradation of memory, thinking, professional qualities.
Provided that the hyperfunction is provoked by a tumor process, the following symptoms also occur:
- Paresis (decreased strength during habitual movements);
- Stool disorders (diarrhea), abdominal pain;
- Excess weight.
However, the hyperfunction of this organ does not have an absolute monopoly on the indicated symptoms; they are also characteristic of a number of other diseases, therefore, if such unpleasant symptoms occur, it is advisable to get to a professional clinic as soon as possible and undergo the required diagnostic procedures.

Excess weight is a frequent accompaniment of hypofunction
Primary symptoms of the disease
The first signs of pancreatic hyperfunction often go unnoticed. They are attributed by patients to nervous strain or fatigue. The main symptoms include:
- fatigue;
- apathy;
- weakness;
- drowsiness;
- convulsive twitching;
- loss of consciousness.
Over time, the symptoms only get worse. Minor convulsive twitches are observed more and more often. Then long, painful attacks appear. A person may lose consciousness unexpectedly, which poses a serious danger to his life. Another specific sign is sudden, groundless weight gain.
Severe diabetes: it may present. Manifestations and pathophysiology of late diabetic syndrome. You might think that this is a consequence of metabolic syndrome or that it is genetic. Destructiveness of the lens. Activation of the alternative sorbitol pathway does not require insulin but results in the accumulation of this polyol with an osmotic effect.
Myo-inositol and glucose compete for transport. Hyperglycemia causes myoinositol deficiency because it is displaced by glucose. Angiopathy: there is intense hyperglycemia, which causes glucosidation of proteins. Microangiopathies: result from the deposition of glycosylated proteins into the wall of small vessels, so that permeability increases and vascular light decreases.
Diagnostics
When a patient suspects this condition, they should go to a place where proper diagnostic procedures are performed. Provincial public hospitals usually lack the required equipment and specialists. Therefore, you first need to find the nearest clinic that offers the necessary services. Procedures that are advisable to perform on a patient include:
- Radioimmunological blood test. The most important parameters include insulin levels, as well as C-peptide data;
- Angiographic examination - x-ray with a contrast agent, it is carried out to detect incipient tumors and determine the stage of their development;
- Computed tomography to study the condition of the digestive system;
- Study of blood glucose levels. The procedure must be carried out on an empty stomach: you cannot eat on the day of the procedure, the day before - eating is allowed no later than 18 pm. A reading below 2-3 mmol per liter indicates hyperfunction of the gland in question and excessive insulin production;
To detect the content of immunoreactive insulin, the patient has a portal vein catheterized.

To prevent glandular diseases, it is necessary to maintain a healthy lifestyle
Functional test - checking the reaction to glucose. Before the procedure, the patient must avoid eating for 15-20 hours. During this time, the blood glucose level has time to drop significantly compared to the routine level, and if there is excessive pancreatic function, the patient will experience signs of a hypoglycemic attack. The patient's blood sugar is measured, and then a glucose solution is administered intravenously.
Prevention
In order to prevent the development of dysfunction of the pancreas, you should follow some preventive rules that will reduce the risk of many diseases. It is necessary to completely stop smoking and drinking alcohol, as well as adhere to proper nutrition and lead an active lifestyle. In order to maintain the gland in normal condition, it is recommended to take vitamin and mineral complexes, especially in the autumn-winter period.
The pancreas is the most important organ of the digestive system, responsible for the complete digestion of food. Disturbance in the functioning of this organ entails damage to other organs of the gastrointestinal tract.
One of these disorders is pancreatic hyperfunction, which occurs against the background of increased insulin production. What causes the development of a pathological process, how does it manifest itself and how to deal with it correctly? This article will answer these and many other questions.
Treatment
The primary task here is to normalize blood glucose levels, since this parameter greatly affects the activity of the entire body, especially brain productivity. Depending on the stage of the disease and the nature of its course, the following methods are used:
- If instrumental examinations show the presence of a tumor process, the neoplasm is removed surgically. If insulinoma is found, it is removed along with some fragments of gland tissue;
- In the event of an acute attack of hypoglycemia, the patient should be given an intravenous injection of glucose solution as soon as possible. The patient must be under constant medical supervision, and a blood glucose test is performed once an hour;
- If the patient has become worse in a chronic condition, he is advised to eat food and drinks rich in simple carbohydrates (sweet tea, chocolate, cookies, etc.);
- During routine therapy, the patient is prescribed drugs that suppress insulin production, such as Diazoxide, Octreotide, as well as medications that increase glucose - the most common of these are glucagon injections. If a patient, some period after the start of therapy, shows signs of enzyme deficiency (and this occurs due to an artificial reduction in the load on the gland, as a result of which it minimizes the production of both hormones and digestive enzymes), medications with enzymes may be prescribed.
It is advisable to recognize the hyperfunction of secretory activity in time, which is complicated by the fact that the early symptoms of the disease process have much in common with the usual signs of accumulating fatigue, among which the patient is often not aware of the problem. However, insulin hypersecretion is dangerous for the entire body. Sometimes it is associated with tumor phenomena. Therefore, this problem must be recognized as early as possible in order to provide the body with relevant therapy.