What is hepatitis C
The disease is caused by the hepatitis C virus (HCV, hepatitis C virus). This RNA virus enters the body primarily through the blood. Damage to the skin and mucous membranes acts as an entry point for the virus. Hepatitis How dangerous and how is it transmitted? Here are the main ways:
- Performing medical procedures and surgical interventions.
- Injecting drugs.
- Cosmetic activities - tattoos, piercings, manicures, pedicures using contaminated instruments.
- Household use of scissors, razors, needles, and other sharp and cutting objects.
- Sexual intercourse accompanied by microtraumas of the genital mucosa.
- In utero from mother to child.
- During childbirth, when the child passes through the damaged, bleeding birth canal of the mother.
Once the hepatitis C virus enters the body, it penetrates into the cells of organs and tissues. HCV has the greatest affinity for liver cells and hepatocytes. Hepatocytes carry out the synthesis of proteins, glycogen, hormones, the formation of bile, the neutralization of toxins, and other liver functions.
After the viral particle or HCV virion enters the cell, a single strand of HCV is released. Then its repeated copying and replication begins. Around each of the resulting daughter replicas, viral organelles are formed - a capsule (capsid), and an outer shell.
This is how new virions are formed, which come out and populate new cells. In all these processes, the NS5A and NS5B proteins play an important role. These proteins are not included in the structure of virions, but ensure their reproduction. Replication of the virus RNA and completion of virions is accompanied by the consumption of organic substances. The virus takes these substances from the hepatocyte. As a result, metabolism (metabolism) inside the liver cell is disrupted, toxins accumulate, and it dies.
Hepatocytes are grouped into lobules. The liver tissue, parenchyma, consists of these hexagonal prismatic formations measuring about 2 mm. Damage to a large number of hepatocytes is accompanied by changes in the structure of the parenchyma and impaired liver function.
Nausea and vomiting
These symptoms are usually not classified as dangerous, and often people simply ignore them. But when nausea and vomiting begin to torment a person constantly and without obvious reasons (poisoning, toxicosis, motion sickness, stress, migraine), this may indicate liver or kidney disease.
Those who develop hepatitis often suffer from an annoying feeling of nausea. It haunts a person due to the deterioration of the liver’s functions to eliminate toxins. Problems with the gastrointestinal tract are also characterized by nausea. If these symptoms occur too frequently, you should seek medical help as soon as possible.
Why is hepatitis C dangerous?
The affected liver cannot do its job. This affects your well-being. There are complaints about:
- general weakness
- nausea, vomiting associated with food intake
- bloating
- flatulence
- diarrhea
- Increase in body temperature to subfebrile levels
- icterus, icteric coloration of the skin and sclera.
The immune system counteracts HCV and destroys a large number of virions. And hepatocytes themselves are capable of generating - new ones are formed to replace dead and damaged cells. With a successful combination of circumstances, the virus is completely destroyed, and the damaged parenchyma is renewed, and recovery occurs. But only 15% of hepatitis C cases end this way.
Basically, despite the resistance of the immune system, the virus manages to gain a foothold in the liver tissue. At the same time, the rate of death of liver cells is low. For this reason, the clinical picture in the acute period is blurred, and jaundice is observed in about a third of patients. In the rest, the disease occurs in an anicteric form, and its onset often goes unnoticed.
On the one hand, this is good - there is no violent onset, and with an asymptomatic, anicteric course there are almost no complaints, and the patient’s condition is stable. On the other hand, the disease is not detected in the acute period, progresses, and is recognized already in a complicated chronic course.
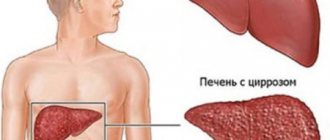
Complications of the hepatitis C virus are directly related to structural changes in the parenchyma. The constant presence or persistence of HCV in the parenchyma triggers a local inflammatory process. Against the background of chronic inflammation in the parenchyma, fat metabolism is disrupted, and steatohepatosis or fatty degeneration develops.
Some of the liver cells with the virus inside are destroyed by the immune system. The fewer hepatocytes, the smaller the parenchyma volume. As a result, fibrous connective tissue grows in its place.
Subsequently, fibrosis progresses and turns into cirrhosis. Almost all parenchyma in cirrhosis loses its lobular structure and is replaced by connective tissue. The liver is no longer able to work, and liver failure develops.
It is worth noting that decades pass from the onset of the disease to the development of cirrhosis. In this case, is hepatitis C dangerous for life? Unfortunately yes. Liver failure is accompanied by toxic encephalopathy, when toxic compounds not neutralized by the liver poison the brain. With encephalopathy, patients often fall into a coma, from which, despite treatment, they do not emerge.
Due to the redistribution of venous blood flow in cirrhosis, the veins of the hemorrhoidal plexus of the lower third of the esophagus become enlarged. The affected liver does not synthesize blood clotting factors in sufficient quantities. This is fraught with bleeding. Bleeding from esophageal varices is a common cause of death in hepatitis C with cirrhosis. There is another danger. Atypically changed cells in cirrhotic tissue sometimes give rise to hepatocellular carcinoma, liver cancer.
Hepatitis C affects more than just the liver. The virus, entering into confrontation with immune cells, changes their properties. Autoimmune reactions develop when antibodies released in response to viral antigens damage their own tissues. During autoimmune reactions with hepatitis C, the skin, joints, brain, myocardium, spleen, and kidneys are damaged.
Long-term persistence of HCV in the blood plasma leads to cryoglobulinemia, the formation of pathological plasma proteins cryoglobulins. These proteins precipitate, clog the vascular lumen, and disrupt blood circulation in the internal organs.
Cryoglobulinemia causes renal failure and aggravates liver failure in hepatitis C. Direct viral damage, intoxication, autoimmune reactions, cryoglobulinemia - all these negative factors contribute to the development of malignant tumors not only in the liver, but also in other organs.
Diagnosis of drug-induced hepatitis
The clinical picture of the disease differs little from other types of hepatitis or other liver lesions.
To confirm the diagnosis and differentiate it from other types of hepatitis, the laboratory test scheme plays an important role:
- general blood and urine tests;
- biochemical blood test (taken from a vein);
- coprogram;
- coagulogram;
- liver biopsy.
Hardware methods for diagnosing drug-induced hepatitis cannot be considered specific; specialists use them to create a complete diagnostic history:
- X-ray - allows you to identify changes in the size of the liver, but is a low-informative method in diagnosing hepatitis, which is not characterized by an increase in the volume of the organ;
- Ultrasound of the liver - diagnoses the size of the organ, density and shape. Does not make it possible to determine the cause of deviations from the norm;
- CT or MRI of the liver - determines the locality or diffuseness of liver changes due to the ability to display layer-by-layer sections. But it also does not provide objectivity about the reasons for the changes.
Laboratory tests are of great importance in diagnosing hepatitis from medications. The use of hardware techniques will help to display only structural changes, without making it possible to determine the cause.
Is hepatitis C dangerous for others?
An infected patient is a priori epidemiologically dangerous. It poses a potential threat to others in terms of the spread of infection. How dangerous is hepatitis C to others? Since the virus is transmitted only through blood, the epidemiological danger is not the patient himself, but objects contaminated with his blood.
But if you follow all the rules of protection, then even if you are in the hospital in the acute stage, a patient with hepatitis C is not dangerous. After all, HCV is not transmitted through saliva or sweat. Therefore, you cannot become infected by coughing, sneezing, or shaking hands. The virus is not transmitted through food or water. The dishes and cutlery used by the patient are also not dangerous. For this reason, infection is impossible in catering establishments - cafes, canteens, restaurants.
Although HCV is transmitted through blood, no cases of hepatitis C transmission through blood-sucking insects have yet been reported. There is a danger of infection through sexual contact. But it can be easily avoided if sexual intercourse is protected.
Changes in the abdominal area

If the liver is faulty, a person often feels unpleasant discomfort in the abdominal cavity: pain or cramping in the lower abdomen, swelling, and a feeling of bloating. Medically speaking, these symptoms may be related to a problem known as ascites, a buildup of fluid in the abdomen that usually occurs in advanced liver disease. Ascites is usually accompanied by portal hypertension (increased blood pressure in the hepatic portal vein system). But fluid can accumulate in the abdominal cavity without liver disease. In any case, if you have obsessive discomfort in the abdominal area, it is better to talk to your doctor.
What is more dangerous – hepatitis C or B?
DNA-containing hepatitis B virus, HBV, Hepatitis B virus, is transmitted through blood or transplacentally. It is impossible to become infected at home through food, water, and common objects if they are not contaminated with blood. The virus multiplies inside hepatocytes, which leads to structural changes and functional disorders in the liver.
In this respect, HBV is similar to HCV. Similar methods of infection and the mechanism of disease development are responsible for a large number of cases of coinfections, when both viruses are present in the patient’s body, and hepatitis B is accompanied by hepatitis C.
But despite the similarities, both diseases have differences. Thus, the acute stage of hepatitis occurs with severe weakness, digestive disorders, jaundice, dark colored urine, and discolored feces. Such violent symptoms allow one to suspect hepatitis in time and begin treatment.
An important role in treatment belongs to synthetic interferons and Ribavirin. These drugs stimulate the immune system and indirectly help destroy the virus. Although with initially strong immunity, spontaneous recovery from hepatitis B also occurs.
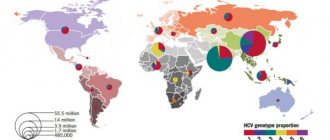
With weak immunity and untimely treatment, hepatitis B becomes chronic, followed by fibrosis and cirrhosis. But the likelihood of chronic hepatitis B is much less than hepatitis C, only 10-30%. Therefore, to the question of what is more dangerous, hepatitis B or C, one could answer: hepatitis B. But among those infected with HBV there are also a considerable number of asymptomatic virus carriers. According to research by experts, this constitutes about 5% of the planet's population.
In addition, hepatitis B sometimes takes a fulminant or fulminant course, when viral aggression over a relatively short period leads to liver failure and death. Fulminant hepatitis C is extremely rare.
Viral
A dangerous infectious type of disease that results from diseases such as rubella, mumps, herpes, AIDS, fever and other viral diseases. Liver damage occurs under the influence of the spread of infectious cells throughout the body. Which in turn leads to a prolonged course of the disease:
- hepatitis A - 3 months,
- hepatitis B and C - up to six months,
- hepatitis B, C and D (chronic form) - more than six months.
This group of diseases of a vital organ is very dangerous for the future health of the patient, since it is practically incurable completely, except for hepatitis A. The disease may go into remission, but not completely disappear. Therefore, it is very important not to bring the condition of your liver to this type of hepatitis.
What is more dangerous – hepatitis C or HIV?
Co-infection with HCV and HIV has often been observed in individuals following blood transfusions and internal organ transplants. After the discovery of HCV in 1989, all donor material is tested not only for HIV, but also for hepatitis C. Therefore, the combination of these diseases after treatment is now not found. But HIV and hepatitis C infections are common among drug addicts.
Hepatitis C has little effect on the course of HIV infection. Even in the absence of HCV, HIV is severe. If the main target for HCV is hepatocytes, then the representative of the HIV family of retroviruses has chosen T-helper cells. This type of lymphocyte is one of the elements of the immune system. Damage to these cells makes the body defenseless against pathogenic infection. As a result, the final phase of HIV infection, AIDS, occurs with atypical pneumonia, malignant tumor growth, and leads to death.
HIV aggravates the course of hepatitis C. Damage to T-helper cells and suppression of the immune system reduces the likelihood of spontaneous recovery to zero. Unchecked by the immune system, HCV multiplies rapidly. Fibrosis progresses rapidly in the liver, and after a short time cirrhosis develops. In addition, with HIV and HCV infection, the risk of hepatocellular carcinoma increases.
Therefore, the answer to the question of what is more dangerous, hepatitis C or HIV, is obvious. Of course HIV. A group of drugs has been created to treat this disease. These drugs inhibit the main stages of HIV reproduction. They were included in the HAART regimen - highly active antiretroviral therapy.
With the right treatment, the development of AIDS can be delayed by decades. But even HAART cannot completely rid a patient of HIV. There are no drugs yet that can treat HIV. But drugs have been created that completely destroy HCV.
Darkening of urine
If, after consuming a normal volume of liquid, a person’s urine acquires a dark tint, this may indicate liver diseases such as hepatitis, cirrhosis, and hepatosis. Urine in such cases has a dark orange, brown or deep yellow color. This is due to high levels of bilirubin, which is characteristic of the phenomenon of jaundice that accompanies most liver diseases.
If the liver is not functioning well, bilirubin is poorly eliminated through the kidneys, so it also colors the urine. But urine can also acquire a dark shade due to a lack of moisture in the body, excessive intake of vitamin supplements, the action of antibiotics, and diseases of the genitourinary system. If there is a clear change in the color of urine within three to five days, it is better to consult a doctor.
How to treat hepatitis C
Hepatitis C can only be treated and cured with direct-acting antiviral drugs (DAAs). These are pills. As active substances, they contain Sofosbuvir in combination with Daclatasvir, Velpatasvir, Ledipasvir. These agents inhibit non-structural viral proteins NS5A NS5B, and suppress intracellular reproduction of HCV¸
DAAs are produced by Indian companies in the form of generics, copies of original American drugs. These drugs act on all genotypes and are capable of destroying the virus even with complicated hepatitis C. Recovery occurs in 95% of cases or more.
Do you want to be cured and forget about hepatitis C forever? Contact GepatitaNet and we will help you.
Did you find apk for android? You can find new Free Android Games and apps.
Tips for strengthening the liver and preventing hepatitis
- Stop drinking alcohol and smoking cigarettes.
- Always wash your hands thoroughly with soap before eating, after going outside and in the toilet.
- Do not have unprotected sex and do not use drugs.
- Observe personal hygiene rules.
- There are foods that cleanse the liver: garlic, turmeric, walnuts, grapefruit, beets, apples, broccoli, avocado, lemon.
- Include high-quality probiotics in your diet to help your liver remove toxins.
- Drink green tea 2 to 3 cups per day.
- Prefer foods rich in vitamin C, which protects the liver from oxidative damage.
- Do not rely too much on animal protein, caffeine, dairy products and limit your salt intake.
- Avoid fast foods and refined sugar.
- Move and do exercises every day. It is useful to do fitness, running, yoga, swimming.
- Avoid constipation.
- Try to control cholesterol and triglyceride levels.
- Get rid of excess weight.
- If you have diabetes, strictly control your blood sugar levels.
- Don't forget to get enough sleep every day.
Signs of drug-induced hepatitis
This disease is a set of inflammatory processes in the liver area, which develops under the influence of drugs. Elderly people are most susceptible to this disease. This is due to the natural processes of aging, during which the size of the organ decreases, as well as its blood supply. These factors lead to a deterioration in the performance of this organ, as a result of which the bio-transformation of medicinal substances occurs more slowly.
Signs of hepatitis that develops under the influence of drugs are extremely varied. This is caused both by various active substances and by the individual characteristics of the patient’s body.
Drug-induced hepatitis is characterized by an increase in liver size, digestive disorders, increased body temperature, chills and fever. Jaundice may or may not be present at all. The severity of symptoms can also vary and directly depends on the dosage of the drug used.
Treatment
Despite the similarity of symptoms, the treatment of each type and type of hepatitis has its own characteristics. Acute viral and toxic pathology, exacerbation of chronic forms is an indication for hospitalization in a hospital, where detoxification therapy is carried out (sodium chloride solution, glucose, colloidal solutions). A drug found to be hepatotoxic should be discontinued or replaced if the patient cannot stop taking it.
Specific treatment exists only in the form of antidotes to paracetamol (N-acetylcysteine), methyl alcohol and ethylene glycol (ethanol). Other measures are based on a strict diet (exclusion of fatty, fried, spicy, salty foods, carbonated drinks, alcohol, strong coffee and tea), bed rest.

A diet is also required for patients with chronic hepatitis in order to reduce the load on the liver. Interferon therapy (Viferon, Alfaferon) is indicated for viral hepatitis B, C, D; immunosuppressive (azathioprine, prednisolone) – in case of an autoimmune process.
Symptoms of reactive hepatitis can only be alleviated by addressing the underlying disease; What measures are taken in this case - conservative (medication, physiotherapy) or surgical - is decided in each case individually.
Ischemic hepatitis leads to massive necrosis; it is necessary to slow down the progression of liver cirrhosis. For this purpose, hepatoprotectors (Essentiale, silymarin, B vitamins) and antioxidants (vitamin E) are used. To eliminate the defect in the lumen of the vessel, surgical treatment is used.