The upper and lower sphincter of the stomach limit its cavity and contribute to the proper movement of food further through the digestive organs. In case of spasm or hypotension, the passage of food is disrupted and irritation of the mucous membrane occurs with hydrochloric acid, followed by inflammation, ulceration and scarring. Treatment of pathology in the early stages is symptomatic and aimed at eliminating the cause of the pathology.
In severe cases, patients are advised to undergo surgery.
Anatomy and structure
There are 2 valves in the stomach that regulate and ensure the normal functioning of the organ. Thanks to them, the forward movement of the food bolus through the organs is ensured and the reverse reflux of food is prevented. The sphincters of the stomach have a pronounced muscular layer, which promotes the opening and tight closing of the holes. They work as a coordinated mechanism, ensuring the movement of food through the intestinal tube. The mechanisms of sphincters are regulated by the central nervous system through special sensory receptors.
Therapy
Therapeutic instructions
Before starting treatment, consult a specialist
The following points must be followed so that the cardia of the stomach works normally and begins to close tightly:
- Correct diagnosis of the causes by a doctor and their subsequent elimination (this applies to pathologies leading to sphincter dysfunction).
- Eat food standing or sitting, keeping your back straight.
- Maintain a gap of 2-3 hours between your last meal and bedtime.
- Elevate your head while you sleep.
- Eliminate from your diet too spicy, fatty, cold or hot, pickled foods.
- Consume plenty of fiber daily and include daily entrees in your diet.
- Switch to smaller meals, do not overeat, especially be careful not to overeat before bed.
- Try to reduce intra-abdominal pressure by reducing the volume of fatty tissue if you are overweight.
- Reduce your consumption of foods that are dangerous to the gastric valve (strong coffee, tomatoes, chocolate, etc.).
- Quit smoking and limit your consumption of alcoholic beverages.
- Try to bend over less.
- Do not lie down after eating so as not to provoke heartburn and aggravate the condition of the esophagus.
- Wear comfortable clothes that are not tight on your body.
- Adjust your physical activity, try to work without significant effort. Walking in the fresh air is especially beneficial.
- Undergo periodic examinations with a gastroenterologist and complete the course of treatment prescribed by him.
- Do not experiment with medications to avoid complications.
Return to contents
Drug treatment
Prokinetics are used as effective treatment, for example: Cerucal, Metoclopramide, Reglan, Domperidone. They increase the activity of the cardiac sphincter, taken before meals up to 4 times a day. Along with prokinetics, medications are prescribed that suppress reflux (propulsid) and antacids that suppress heartburn (“Gaviscon”, “Almagel”, “Smecta”, “Maalox”, “Gastal”, “Phosphalugel”).
Treatment is supported by omeprazole to restore the walls of the esophagus, antiemetics and painkillers. Sometimes it is necessary to use antiprotozoal drugs and antibiotics.
Return to contents
Types of Gastric Valves
The upper or cardiac sphincter is located between the esophagus and the stomach. Normally, it is constantly closed and opens only when a person swallows food. The cardia has a rosette appearance and its weakening leads to esophageal reflux disease. The lower sphincter is located at the junction of the duodenum. Its opening occurs when receptors on the gastric mucosa near the outlet to the intestine are irritated by hydrochloric acid. And it closes when the acidity in the small intestine increases, to which the same receptors react. When the muscle that forms it weakens, it leads to peptic ulcer of the duodenum and stomach.
Cardiac sphincter
The cardinal valve serves to separate the contents of the stomach from the esophagus.
Separates the contents of the stomach from the esophagus. Thanks to it, food moves forward and prevents its return into the oral cavity. The valve is open only during swallowing, and the rest of the time its muscles are tightly closed. The insufficiency of this formation is associated with an increase in intra-abdominal pressure or the development of diaphragmatic hernias and causes esophageal reflux disease. Without the necessary treatment, the pathology can cause ulceration of the esophagus and impair its patency.
Pyloric valve
The gastric sphincter is located at the junction with the small intestine. Prevents the reflux of contents from the intestine into the stomach through peristaltic waves. Equally important is its timely closure to prevent hydrochloric acid from entering the duodenum. If the septum does not close or it is hypotonic, this can cause irritation of the mucous membrane of the stomach, pylorus and small intestine, with the subsequent development of ulcers and erosions in them. The pyloric sphincter closes in response to an impulse from the central nervous system.
Symptoms
Heartburn is one of the first clearly visible symptoms of the disease.
The most striking symptom of cardiac failure is heartburn, which makes itself felt regardless of food intake. In addition to this, the violation is accompanied by the following problems:
- belching of air with a bitter or sour taste;
- aching or burning pain in the sternum;
- pain in the epigastric region;
- rumbling sounds in the intestines;
- obsessive nausea, sudden vomiting;
- increased fatigue, dizziness, weakness.
These conditions may be accompanied by dizziness, rumbling in the stomach and the appearance of a white coating on the tongue, which indicates inflammation of the walls of the esophagus.
Return to contents
Diseases of the gastric sphincter, their causes and symptoms
The pathology of the gastric cardia can be provoked by the influence of the following factors on the human body:

A constant cough can provoke pathology of the valve of the digestive organ.
- bad habits;
- heavy physical activity;
- sedentary lifestyle;
- constant and debilitating cough;
- frequent constipation;
- diaphragmatic hernia.
In this case, the patient is bothered by constant heartburn and a burning sensation in the chest. Periodic pain in the epigastrium and heaviness after eating occur. The tongue is covered with a white coating, and a sour odor emanates from the mouth. If left untreated, reflux disease can lead to massive bleeding from the esophagus, ulceration with subsequent scarring and narrowing of the passage.
The following factors contribute to the occurrence of disturbances in the functioning of the gatekeeper:
- high intra-abdominal pressure;
- significant physical activity;
- frequent straining;
- cough;
- excess body weight;
- pregnancy;
- incorrect diet.
Malfunction of the pylorus causes indigestion and constant aching pain in the epigastrium. Food begins to be poorly digested and an eating disorder occurs. With a long course of the pathology, metaplasia of the gastric epithelium may occur with the formation of cells of the intestinal mucosa. Such conditions are a precancerous condition and provoke peptic ulcers of the stomach and duodenum. Excessive activity of the pylorus leads to pylorospasm and stagnation of food. This causes nausea, vomiting and intoxication of the body.
Pylorospasm
It occurs as a result of increased tone of the lower gastric sphincter. As a result, the normal passage of food through the gastrointestinal tract is disrupted. The presence of pathology over a long period of time can lead to starvation and exhaustion of the patient. Violation of the movement of chyme through the intestines causes rotting of food in the stomach, nausea and vomiting in the patient, as well as toxic products entering the blood. A slight delay in the movement of food causes pain in the epigastrium, a feeling of fullness in the stomach and flatulence.
Esophageal achalasia
Represents spasm and excessive tension of the cardiac sphincter. As a result, food is unable to pass from the esophagus to the stomach. The accumulation of food particles causes food rotting, bad breath, dysphagia and exhaustion of the patient. As a result of constant trauma to the mucous membrane, scars form on the mucous membrane of the esophagus, which lead to narrowing of the opening, bleeding and ulceration. Stagnation of food disrupts its absorption and supply of nutrients necessary for the body. A man suffers from anorexia and is starving.
Gastroesophageal reflux
Insufficiency of the cardiac sphincter of the stomach, as a result of which dysphagia, regurgitation of gastric contents develops, and the patient complains of heaviness and pain in the epigastrium. The pathology is associated with impaired tone of the muscles that form the septum. In this case, the sphincter does not work strongly enough and does not close the hole. Hydrochloric acid entering the esophagus corrodes the walls and leads to bleeding, ulcers and scarring of the mucous membrane, followed by its narrowing.
Causes of deficiency
Obesity can cause illness.
There are two groups of reasons, which are defined as organic and functional. The former are not associated with anatomical defects of the body and occur due to hiatal hernias or postoperative complications. Due to functional disorders, the cardiac sphincter does not close tightly and works in the opposite direction. He is hampered by pressure in the stomach cavity or intra-abdominal pressure, pyloric spasm. The valve muscles themselves lose tone, become weak and unclench. These ailments are preceded by the following regime violations:
- binge eating;
- eating food immediately before bedtime;
- obesity;
- passive lifestyle;
- constipation;
- excessive physical activity.
The causes of weak valve muscles include previous surgeries, pregnancy and chronic stomach diseases. Some foods and habits are harmful to the normal tone of the sphincter muscles:
- tomatoes;
- chocolate;
- coffee;
- fatty foods;
- smoking;
- alcohol.
Return to contents
Diagnosis and treatment

You can suspect that a patient has a dysfunction of the upper or lower gastric sphincters based on the symptoms characteristic of this pathology. To confirm the diagnosis, it is necessary to perform radiography with contrast and fibrogastroduodenoscopy. It is also important to do pH measurements of gastric juice, the contents of the esophagus and intestines. It is recommended to conduct a general blood and urine test.
Magnetic resonance imaging is used as an additional diagnostic method.
The basis in the treatment of pathology is to eliminate the cause of increased intra-abdominal pressure or weakness of the sphincter muscles. To eliminate the symptoms of sphincter insufficiency, antacids are used. To eliminate achalasia and pylorospasm, antispasmodics will be needed. The most common among them are “No-shpa” and “Drotaverine”. In severe cases, surgery is indicated to restore the structural integrity of the sphincter or normalize its patency.
Benefits of reflux surgery
At the research stage, before sending a person to a surgeon, the doctor must determine such important indicators as:
- condition of the lower part of the passage to the esophagus;
- presence of diaphragm displacement;
- spontaneous relaxation of the sphincter.

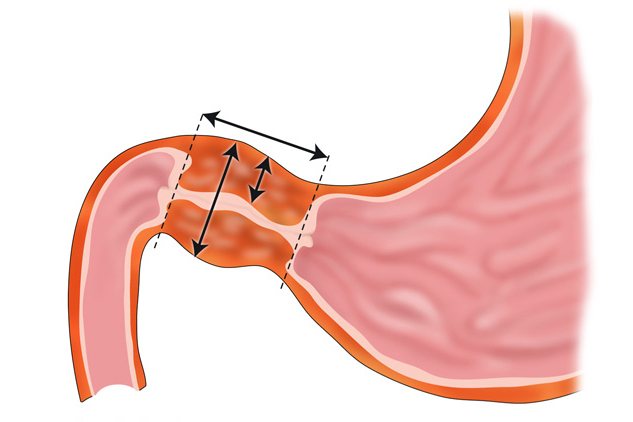
Arbitrary opening of the esophageal sphincter causes the reflux of substances into the esophagus and the development of the disease
The main provoking factor of reflux esophagitis is spontaneous relaxation of the sphincter. Insignificant, but indicating the severity of inflammation, are the stagnation of contrast in the esophagus and the duration of the lumen.
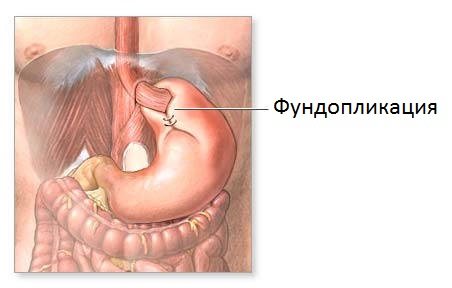
With the help of surgery, you can change the hernia and increase the tone of the sphincter.
After laparoscopic operations, 90% of patients are satisfied with the results, and this despite the occurrence of adverse events after the intervention. Typically, after this type of intervention, the patient must be observed by a doctor for several more years. An important point worth noting is the change in quality of life. Patients with severe reflux esophagitis after surgery note that their lives have become the same as those of healthy people.
Surgical intervention helps reduce heartburn, pain in the epigastric region, belching, nausea, cough at night, and wheezing.
After surgery, patients require less medical supervision. Although during the rehabilitation period (the first 3 months) you should undergo a full examination to ensure positive results. In the postoperative period, it is important to know whether signs of inflammation (esophagitis) remain in the esophagus.
After the operation, the patient needs to be monitored by a doctor to consolidate the results.
Patients spend no more than 4 days in the clinic after surgery.
Research and doctor's notes show that surgery produces better results than traditional treatment. This concerns not only the feelings of patients, but also the overall picture as a whole.
The arguments in favor of surgical intervention are as follows:
- surgery eliminates the cause of reflux esophagitis, and drug treatment only removes the symptoms;
- more than 85% of patients are satisfied with the positive dynamics;
- 86% of patients do not need to take medications after surgery;
- the need to see doctors is reduced.
The operation will not have a positive outcome if it is performed by an unqualified surgeon.

Surgery can cure the disease










