Last updated June 25, 2020 at 05:47 pm
Reading time: 5 min
Pregnancy for any woman is the most significant, requiring unquestioning seriousness, and at the same time the happiest period of life. Every expectant mother wishes her baby to be born and grow up strong and healthy, and this largely depends on taking care of her personal condition during the period of gestation.
What should be done if a woman is diagnosed with worms during pregnancy?
The most important thing is not to self-medicate. It is important to remember that any careless action can negatively affect the future development of the child.
Worms in pregnant women are a removable phenomenon, and in order not to cause harm to your baby, you should immediately contact a specialist and begin proper therapy.
The nature of helminthiasis
The opinions of scientists boil down to the fact that human existence is impossible without parasites. Along with many other microorganisms, they are an integral part of the human biosystem. The difference is that most of them are harmless, and only certain types of helminths that are in the active reproduction phase can poison human health with the products of their vital activity, and therefore require responsible treatment.
The more common worms in the human body are roundworms and pinworms, but there are also such as trichinella, whipworms, bovine and pork tapeworms. Basically, parasites concentrate in the intestines, but they can also affect any other organs, existing and developing at the expense of someone else’s body.
Prevention of worms during pregnancy and during planning
- Pregnant and planning women should know a number of preventive rules of personal hygiene:
- wash your hands with soap after walking, contacting animals, or touching public things;
- wash vegetables and fruits thoroughly;
- eat meat or fish only after high-quality heat treatment;
- store food products protected from animals, rodents, insects;
- Wash bed linen, towels, clothes regularly, be sure to iron or steam after washing;
- wash yourself using intimate hygiene products every day;
- Do not bite your nails, pens, pencils.
Drug prevention of worms for pregnant women is contraindicated, and if you are planning a pregnancy, then inform the doctor who prescribes the medicine about this - depending on the drug used for prevention, a break in planning may be necessary. The fact is that, in fact, these drugs are poison. Some of them are very dangerous for the fetus in the early stages and can lead to miscarriage or the development of pathologies.
- Indications for prophylactic use of anthelmintic drugs are:
- contact with domestic animals, caring for livestock;
- working with land;
- sandbox games;
- visiting exotic countries;
- fishing, hunting and outdoor sports (beach volleyball, football, etc.).
Worms are expelled with feces, so after each trip to the toilet you need to wash yourself thoroughly with soap.
The danger of helminthic infestations for the expectant mother

During pregnancy, worms have an extremely negative effect on the woman’s condition as a whole. The invasion increases the manifestations of toxicosis, as a result of which the female body does not receive the required amount of nutrients and very soon weakens.
Adverse consequences for pregnant women are caused by enterobiasis, a disease caused by worms from the genus pinworms that live in the intestines. Pinworms can invade the birth canal, cause damage to their mucous membrane and thereby open the way for various infections. In addition, they cause severe irritation, which leads to insomnia and disorders of the nervous system of the expectant mother.
Diseases such as necatoriasis and hookworm also pose a danger when carrying a child. Their causative agents are round helminths that settle in the duodenum. They can harm its cavity, thereby causing continuous bleeding, which, as a consequence, leads to hypochromic anemia.
What is the danger of helminthiases for humans?
Nematodes that live in the small intestine of their victims cause iron deficiency anemia and malnutrition. Lymphatic filariasis is characterized by lymphedema (lymphostasis) and elephantiasis. Roundworms living in the colon can lead to colitis, dysentery-like stools, and rectal prolapse. Widely known ascariasis is the cause of intestinal obstruction, blockage of the biliary tract, and malnutrition.
Schistosomiasis trematodes are a source of inflammation of the intestines, urinary and biliary tracts. The eggs of this helminth penetrate the cervix and body of the uterus, the bladder, and the vagina, causing cystitis, blockage of the ureters, pyelonephritis and kidney failure. Blockage of the fallopian tubes subsequently becomes the cause of their chronic inflammation and ectopic pregnancy.
Consequences of helminthic infestations for the unborn baby

For the baby in the mother's womb, ascariasis and toxoplasmosis are the most fraught with harmful consequences. The entry of roundworm larvae into the baby's brain through the placenta threatens changes in its development and can also cause a difficult birth.
When helminths penetrate the lungs, the baby will become resistant to colds of the respiratory system from birth.
Toxoplasmosis is the most merciless parasite during pregnancy, since it can provoke the death of the baby in the womb or at birth. In other cases, there is a possibility of inhibition of the child’s development, the appearance of epilepsy or cerebral palsy.
How to get rid of worms during pregnancy
Before starting treatment for worms in pregnant women, it is necessary to conduct a thorough diagnosis in the laboratory. After all the necessary research, the doctor prescribes medications in accordance with the type of helminthic infestation and the stage of pregnancy. Medicines or traditional medicine are prescribed that are safe for the fetus and the expectant mother. Worms during pregnancy deprive the body of many beneficial nutrients, cause severe discomfort, and often cause serious complications. For this reason, helminthiasis requires mandatory treatment.
Pinworms
This type of worm lives in the large and small intestines, which leads to a woman experiencing constant itching in the anus and genital area.
Pinworms can move throughout the intestines and cause attacks of appendicitis. The nervous state of a sick woman is sure to be passed on to the baby.
Roundworms
If worms of this category enter the mother’s bloodstream, then after birth the child may have problems with the bronchi and lungs, and all sorts of allergic reactions will appear. When the disease is advanced, worms can even penetrate the placenta, as a result of which the child may die from insufficient blood supply.
Round parasites
These worms reproduce in the duodenum and feed exclusively on blood. The danger of helminths is quite high, since they damage the wall of the duodenal cyst, thereby causing bleeding, and this is iron deficiency anemia.
This is dangerous not only for the woman, but also for the fetus.
Lack of oxygen and low hemoglobin are the path to termination of pregnancy and all sorts of complications in the development of the child.
Breeding grounds for parasites
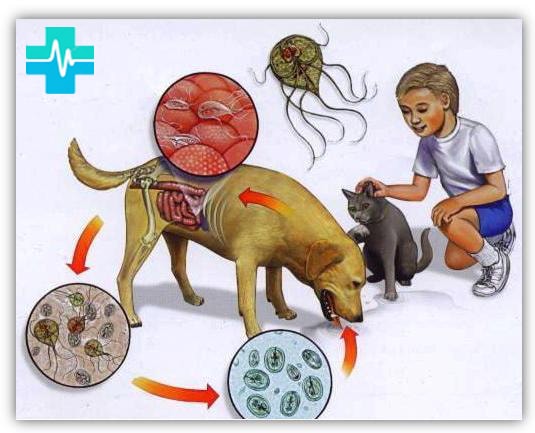
It is very easy for anyone to become infected with helminths, not just pregnant women. You can become a hostage to various parasitic organisms either through your own fault or under circumstances that cannot be controlled.
Main sources of worm infection:
- the soil for growing vegetables and fruits in vegetable gardens and garden plots is usually fertilized with animal feces, which may contain parasite larvae;
- food from the garden, which does not require heat treatment before consumption, does not exclude the possibility of infection even after washing with water;
- worm eggs can be introduced into your body simply by inhaling air contaminated by them;
- money is a household item for countless people, including helminth owners;
- bodily contact with an infected person or objects used by him can cause infection;
- playgrounds for children are often used by street animals as places where they can relieve themselves, as a result of which all the larvae of worms that are contained in the products of their vital activity end up in the children's sandbox;
- freshwater bodies of water are also filled with parasite eggs, which can easily enter the human body while swimming;
- infected pets are carriers of worms contained not only in their feces, but also on their skin and fur;
- With insufficient heat treatment, meat and fish products can become foci of helminth infection.
Symptoms of worms in pregnant women
A woman must take anthelmintic measures even at the time when pregnancy first appeared in the family plans. But worms during pregnancy are not at all uncommon and are an everyday occurrence. Pregnant women can become infected with helminths by contacting a sick person while eating contaminated, unwashed fruits and vegetables, from communicating with pets (dog, cat), in public places, or when counting money.
The main manifestations of the presence of parasites in the body of the expectant mother are expressed as:

Drowsiness
- unbearable itching of the anus;
- sudden weight loss or weight gain;
- drowsiness;
- nausea and vomiting;
- weakness and digestive disorders;
- irritation of the skin of the fingers, eyelids;
- grinding teeth in sleep.
In the presence of the above conditions, pregnant women must undergo the necessary tests to confirm or refute infection with worms.
Signals of worm infection during pregnancy
Worms of various types in a pregnant woman, alas, are not uncommon. Hormonal changes and a decrease in the body's protective functions when carrying a child increase the risk of helminthiasis.
It is no secret that the pregnancy process under normal conditions occurs with certain negative symptoms, such as:
- nausea;
- dizziness;
- asthenicity;
- instability of emotional state.
When parasites appear during pregnancy, similar signs can signal this, so it can be extremely difficult to spot a hint of helminthic infestation among them.
In addition, a number of symptoms are inherent in helminth infection:
- temperature increase;
- indigestion;
- loss of appetite;
- weight loss;
- pain in the liver area;
- skin rashes;
- dry cough;
- itching in the anus and birth canal;
- insomnia.
With prolonged parasitism in the human body, worms begin to actively appear in the stool, sometimes on underwear. Pinworms look like small white worms about 1 cm in length. Roundworms reach up to 40 cm in length with a diameter of 0.3-0.6 cm and are much less often visible, but if they appear, it is impossible not to notice them.
What are the dangers of parasites during pregnancy?
Every third pregnant woman infected with helminths (hookworms, strongyloidiasis, trichuriasis) develops hypochromic anemia at the beginning of pregnancy, which progresses in the second and third trimesters. B12-deficiency (megaloblastic) anemia is observed in diphyllobothriasis. Attempts to eliminate anemia without deworming are unsuccessful. Helminths often increase vascular permeability, cause albuminuria, and cause irritation of the epithelium of the urinary tract, clinically manifested by cystitis and pyelonephritis.
With ascariasis and strongyloidiasis, attacks of bronchial asthma may occur as a result of the migration of their larvae into the pulmonary circulation and airways. With strongyloidiasis, skin lesions occur due to the migration of their larvae into the skin. With trichinosis and cestodes (taeniasis, teniarinchiasis, diphyllobothriasis, hymenolepiasis), transient fever often occurs. Ascariasis can cause obstructive jaundice. Steatorrhea is characteristic of strongyloidiasis.
Women suffering from helminthiasis often face the threat of miscarriage , premature birth , and spontaneous abortion in the early stages of pregnancy. Some patients experience recurrent miscarriage without clear reasons. This pathology of pregnancy often develops with trichuriasis (14.8%) and ascariasis (10%).
Helminthic infestation affects the blood coagulation system by changing the enzymatic function of the liver, which is associated with bleeding observed in the postpartum period in every 6th postpartum woman, which cannot be explained by obstetric pathology.
In 1/3 of pregnant women with helminths, especially trichuriasis and ascariasis, carbohydrate metabolism disorders (hyper- and hypoglycemia) were established. After deworming, carbohydrate metabolism is normalized. With hymenolepidosis and enterobiasis, damage to the urinary tract may occur, leading to azotemia. Treatment of helminthiasis eliminates renal failure.
Helminthiasis is often accompanied by eosinophilia. The number of eosinophils reaches 0.44-109/l. The number of eosinophils should be expressed in absolute numbers and not as a percentage. Eosinophilia is the most common marker of helminthiasis. However, the only specific method for diagnosing helminthiases is examining stool for worm eggs or cysts . Feces should be delivered to the laboratory within the first 24 hours, since the eggs of some helminths contained in them quickly become deformed.
The waste products of helminths can have a harmful effect on the fetus, which is manifested by disruption of its development, sometimes by asphyxia. Intrauterine infection of fetuses, proven in animal experiments, is not always established in newborns, either soon after birth or in the coming years. However, metabolic products of parasites are transmitted through mother's milk to the child, causing dyspeptic symptoms that cannot be treated, but quickly disappear after deworming of the mother .
All authors studying helminthiasis in pregnant women are unanimous in the opinion that deworming is necessary at any stage of pregnancy, as it significantly improves the outcomes of pregnancy and childbirth. All pregnant women should have their stool tested for worm eggs at the antenatal clinic . Patients with helminthiasis should be registered at a dispensary and sent to a hospital for treatment.
The most common helminths in pregnant women:
- Hookworms parasitize the small intestine, often the duodenum. Infection occurs when the pathogen is ingested with unwashed fruits, vegetables, or raw water. Helminths become fixed in the intestinal mucosa, causing hemorrhages, bleeding, and anemia. The disease is manifested by nausea, vomiting, salivation, constipation or diarrhea, itching, eosinophilia, hypochromic anemia, asthmatic conditions, fever. The diagnosis is confirmed by the detection of hookworm eggs in the stool. The lifespan of hookworms is up to 20 years. Treatment for severe anemia begins with the use of iron supplements. With hypertension and pregnancy, a short-term drop in blood pressure may occur.
- Roundworms parasitize the human small intestine. Infection occurs when ascaris eggs are ingested with unwashed fruits, vegetables, or raw water. The lifespan of roundworms is up to 1 year. Clinically, ascariasis is manifested by salivation, loss of appetite, nausea, vomiting, cramping pain around the navel, weakness, decreased blood pressure, dizziness, headache, fatigue, and insomnia. Many symptoms can be mistaken for those of early toxicosis in pregnant women. The diagnosis is based on the detection of roundworm eggs in the feces.
- The whipworm parasitizes the human colon. Infection occurs when eggs are ingested with vegetables, berries, or water. The lifespan of the parasite in the intestines is 5 years. The disease may be asymptomatic, or may manifest itself as salivation, loss of appetite, pain in the right half of the abdomen and epigastrium, nausea, vomiting, constipation or diarrhea. With diarrhea, there may be mucus and blood in the stool. Possible headaches, dizziness, restless sleep, hypochromic anemia and leukocytosis. Eggs in feces can often be detected only with repeated tests.
- Enterobiasis . Pinworms parasitize the lower part of the small and large intestines. Eggs are laid by females on the skin of the patient. Infection occurs through ingestion of eggs. The lifespan of pinworms is 28–56 days. The main clinical symptom is itching of the skin in the anal area at night. Often there is nausea, loss of appetite, dry mouth, cramping abdominal pain, diarrhea with mucus, insomnia, irritation of the skin around the anus (dermatitis), in the perineum and genital area, vulvovaginitis, pyelonephritis, cystitis, bedwetting. Pinworm eggs should be looked for not in feces, but in scrapings from the mucous membrane and the anal area. Treatment is effective with simultaneous deworming of all infested family members.
- Hymenolepidosis . The dwarf tapeworm parasitizes the small intestine, where it causes inflammation of the mucous membrane with copious mucus secretion. Life expectancy is unknown. Patients complain of decreased appetite, nausea, abdominal pain, diarrhea or constipation, dizziness, fatigue, and restless sleep. Sometimes there is anemia and eosinophilia. The diagnosis is made by detecting dwarf tapeworm eggs in the stool.
- Diphyllobothriasis . The broad tapeworm lives in the intestines for decades. Infection occurs by eating raw river fish or fresh, poorly salted caviar. The tapeworm absorbs vitamin B12 from the intestinal wound, and patients may develop pernicious-like anemia. Women complain of weakness, dizziness, and abdominal pain. The diagnosis is made by detecting tapeworm eggs in feces. Treatment consists of prescribing vitamin B12 300–500 mcg intramuscularly every other day for 1 month, and iron supplements.
- Teniarinhoz. Bovine tapeworm lives in the intestines for many years. Infection occurs by eating raw beef. Patients are concerned about weakness, sometimes nausea, vomiting, abdominal pain, Minière's syndrome, and epileptiform seizures. The segments of the bull tapeworm can be independently released from the anus, and their detection confirms the diagnosis, as does the identification of parasite eggs in stool or scrapings from the skin around the anus.
- Taeniasis . Pork tapeworm has been a parasite in the human small intestine for many years. Infection occurs by eating half-cooked pork. The clinical picture is the same as for bovine tapeworm infestation, but the segments do not come out of the anus on their own. The diagnosis is made based on the detection of tapeworm eggs in the stool or scraping of mucus from the perianal folds.
We have provided a brief description of the most common helminths in pregnant women. We observed other helminthiases (trichinosis, opisthorchiasis, echinococcosis, etc.) only in a few patients.
Treatment is not carried out in the first trimester of pregnancy, since the drugs used for this purpose are contraindicated for pregnant women.
From the second trimester, praziquantel 20 mg/kg once can be used. In some patients, Fenasal, prescribed as for hymenolepiasis, is effective. Levamisole, mebendazole (Vermox), medamin, pyrantel (combantrin), tansy flowers are contraindicated for pregnant women . It must be remembered that most drugs used in the treatment of helminthiases are strictly contraindicated in the first trimester of pregnancy. Particular attention should be paid to the restoration of colon microbiocenosis in patients with intestinal helminthiases. In order to increase the effectiveness of treatment, it is recommended to prescribe bificol, milk bifidum-bacterin.
The anthelmintic effect is exerted by:
- carrots and carrot juice,
- Walnut,
- wild strawberry,
- pomegranate (especially pomegranate juice) and garlic.
Although the effectiveness of herbal medicine for helminth infections is low, the introduction of foods with anthelmintic effects into the diet increases the effect of medications prescribed by a doctor and is a good preventive measure. During pregnancy, a woman needs to support her immune system . For this, the “Balance Formula Plus” is indicated (1 capsule 2 times a day). It will help the child develop harmoniously and will resist the harmful effects of parasites on the body of mother and baby. “Balance Formula Plus” is also recommended to be given to the child from the first day of life . To do this, you need to open the capsule and sprinkle the contents onto the nipple while breastfeeding. The substance saturates the child’s body with all the necessary vitamins, calcium and colostrum with a 30% content of immunoglobulin G (immulac).
Recommended course of use during pregnancy:
Course 1
- In the morning: 2 capsules of “Marina-Plus”,
- During the day: 1 Vitacompa capsule,
- Evening: 1 capsule of Element 1. Balance Formula Plus.
Course 2
- In the morning: 1 bag of Poseidon tea,
- During the day: 2 capsules of “Gortex”,
- Evening: 1 capsule of Element 1. Balance Formula Plus.
In the life of every pregnant woman, sooner or later there comes a time when the gynecologist hands her a stack of referrals for laboratory tests . But if the need to take a general blood and urine test usually does not raise any complaints, expectant mothers are often suspicious of tests for sexually transmitted infections (STIs) or TORCH complex .
“Our grandmothers did not undergo any tests, gave birth in the field and felt great!” - Some people wave it off. “I’m a decent woman, why do I need your HIV test?” - others are indignant. Why are these studies carried out and how much do a pregnant woman and her unborn baby need them?
It has long been known that the human body is by no means sterile, and a wide variety of microorganisms, both opportunistic and pathogenic, can live in it, and there are often cases when such coexistence is practically asymptomatic, without clinical signs of infection. However, even an asymptomatic infection that does not cause inconvenience to a pregnant woman can be dangerous for the fetus, causing a host of pathological conditions : from malformations to spontaneous abortions and stillbirths.
Infections, predominantly sexually transmitted
- Syphilis. Intrauterine infection with this classic venereal disease is extremely dangerous for a child; it can cause chorioretinitis, hepatosplenomegaly, damage to the skeletal system, syphilitic pemphigus, intrauterine death and spontaneous abortion. The most dangerous is the secondary period of syphilis, which develops in a woman approximately 10 weeks after infection and can last up to 3-4 years; it is during this period that the causative agent of syphilis (treponema pallidum) can easily spread through the blood vessels and infect the fetus. Infection usually occurs no earlier than the 4th–5th month of pregnancy, when the placenta is formed, through the vessels of which the pathogen enters the fetus. Therefore, primary screening of pregnant women (by enzyme immunoassay or microprecipitation reaction) is carried out repeatedly: in the first trimester (usually upon registration), the second and third trimester, which makes it possible to prevent congenital syphilis of the fetus through timely detection and treatment of the mother. If the screening results are positive, then the pregnant woman is subject to mandatory examination in order to clarify the diagnosis and, if necessary, carry out the necessary treatment. Interesting fact : due to changes in the protein composition of the blood in pregnant women, false positive test results for syphilis occur, but you should not be afraid of this, since there are highly specific confirmatory tests that allow you to exclude a false positive result.
- Gonorrhea. One of the most common causes of infertility in women. If pregnancy does occur, it is often complicated by spontaneous abortion, premature birth, and postpartum infections of the uterus and appendages. The fetus usually becomes infected in utero (chorioamnionitis or sepsis develops) or during childbirth (gonococcal conjunctivitis, otitis media, and in girls – vulvovaginitis). Therefore, pregnant women must be examined for gonorrheal infection by bacteriological method (culture) upon registration and further according to indications (for example, with a large number of leukocytes in the smear).
- HIV infection. The risk of HIV transmission from mother to child during pregnancy and breastfeeding is very high, but with timely treatment it is significantly reduced. Since the incubation period for HIV infection is quite long, pregnant women are examined 2 times: upon registration and in the third trimester of pregnancy.
- Chlamydia. 35% of newborns whose mothers have chlamydial infection develop conjunctivitis, and 10–20% develop pneumonia. Infection usually occurs during childbirth. Therefore, pregnant women are screened for chlamydia once, usually in the second trimester. It should be noted that the most sensitive and specific methods are the cell culture method (rarely used due to complexity and labor intensity) and the real-time polymerase chain reaction (PCR) method. Other methods give a large percentage of false results and should not be used for diagnosis in pregnant women.
- Mycoplasmosis. As with chlamydia, infection with mycoplasmas occurs during childbirth. It manifests itself in newborns in the form of severe pneumonia, the mortality rate of which can reach 15%. Material for testing for mycoplasma and chlamydia is usually collected simultaneously.
- TORCH syndrome is an abbreviation for the most common intrauterine infections (T - toxoplasmosis, O - others, which includes various infections, including those mentioned, R - rubella, C - cytomegalovirus, H - herpes).
- Toxoplasmosis - a pregnant woman can become infected with toxoplasmosis by communicating with animals that secrete toxoplasma oocysts (cats, dogs, rabbits), as well as by eating raw or undercooked meat, especially pork ( this also applies to the habit of tasting raw minced meat ). In the fetus and newborn, the infection manifests itself as damage to the eyes (congenital cataracts, glaucoma, optic nerve atrophy), liver (hepatitis) and brain (meningoencephalitis), as well as generalized toxoplasmosis. Infection usually occurs when a pregnant woman encounters a toxoplasma infection for the first time, so the determination of class M immunoglobulins (in the second or third trimester) is diagnostically significant.
- Herpes. All types of herpes viruses can cause infection in a newborn, but the most dangerous type for a child is type 2 (which causes genital herpes in the mother). The likelihood of infection of the fetus, as in the case of toxoplasmosis, depends on how long the pregnant woman has been infected. The “fresh” the infection, the more likely the child is to become infected. Herpes viruses cause damage to the eyes and mucous membranes of newborns, herpetic encephalitis (up to necrosis of brain tissue), hemorrhagic syndrome and even herpetic sepsis. Among laboratory diagnostic methods, the “gold standard” is the isolation of the virus in cell culture or the real-time PCR method (in the second or third trimester). Determining the level of class M immunoglobulins is also indicative (a high level indicates an acute infection).
- Rubella. This is a classic teratogenic virus. If a mother becomes infected with rubella in the 1st trimester, then the probability of the disease in the fetus is 25%, after the 5th month - 1–2%. Considering the high probability of developing congenital rubella after a mother has had a rubella infection (Greg's triad - heart defects, eye damage, deafness), it is advisable to be examined for the presence of antibodies to rubella before pregnancy, and if the mother is seronegative, vaccinate with rubella vaccine.
Thus, timely examination of a pregnant woman for the presence of pathogens of infectious diseases will not only not harm the course of pregnancy, but will also help to promptly identify or prevent infection and its serious consequences in the child.
The key stages in the diagnosis of helminthiasis, along with clinical manifestations, include :
- geographical and migration history;
- food history (eating behavior, eating habits);
- epidemic risk factors (contact with soil, domestic animals, etc.).
These diagnostic stages allow us to assume a parasitic etiology of the disease and plan subsequent clinical, instrumental and laboratory studies. Biological material for research on the presence of helminths , their fragments, larvae and eggs are feces, urine, duodenal contents, bile, sputum, rectal and perianal mucus, blood, and muscle tissue. The most common object of study is feces.
In order to diagnose helminthiasis and pathology caused by tissue helminths or larval stages (echinococcosis, cysticercosis, trichinosis, toxocariasis), serological methods are widely used. An increase in the level of eosinophils several times higher than normal in clinical practice often serves as a hematological marker that allows one to suspect the presence of helminthiasis. For topical diagnostics, ultrasound examination of internal organs, computed tomography, and endoscopy with biopsy are used.
Diagnosis of helminthiasis during pregnancy

In order to find out the nature of the origin of unnatural symptoms, you need to contact a specialist and undergo laboratory tests of stool and blood. Their results will prove or disprove the conclusion of helminthiasis in a pregnant woman.
If a disease such as ascariasis is confirmed, there will be a need to conduct additional studies of the condition of the unborn baby: ultrasound and analysis of amniotic fluid.
Do we treat or cripple?
If test results are positive for the presence of harmful microorganisms during pregnancy, logical questions arise:
what to do and how to treat pregnant women for worms?
In modern medicine there is no unanimous opinion whether it is worth treating worms during pregnancy, or whether the harm from drug intervention will exceed the benefits for the development of the fetus.
Some experts are of the opinion that during pregnancy, treatment of helminthiasis is a necessary measure. But therapy can be started no earlier than in the penultimate trimester, since the first 12 weeks are fundamental in the formation of all the internal organs of the baby. Other doctors deny the adequacy of treatment for infected pregnant women until the birth of the child, arguing that this is possible damage to his health due to the mother taking medications.
Pregnancy and various parasites are an unpredictable combination, so each specific case is individual. When a doctor prescribes treatment for various worms in pregnant women, the type of worms found, the general state of health and the symptoms of the disease are taken into account.
Waiting until the baby is born is sometimes the right decision, but in some cases you need to act immediately.
Prevention
Any disease is easier to prevent than to treat. Therefore, in order not to worry about helminth infection, pregnant women and her family members should follow simple preventive rules:
- wash your hands thoroughly with soap - before eating, after going outdoors, after visiting the restroom, interacting with animals, or money;
- exclude any potential interaction of rodents, insects with food and food products;
- subject to thermal and chemical treatment all kitchen utensils that have been in contact with meat or fish;
- Thoroughly wash fruits, herbs and vegetables. Use heat treatment when preparing them;
- use underwear (panties) that fit tightly to the body;
- wash bed linen and towels often and in very hot water. Washed items must be ironed on both sides;
- forget about bad habits - biting your nails;
- undergo periodic tests for helminthiasis.
Getting rid of worms during pregnancy is problematic, but not difficult. All recommendations of the preventive plan that help prevent parasites from entering the body are quite easy and accessible. It is necessary to maintain personal hygiene, thereby protecting yourself from the scourge of worms.
Drug treatment for expectant mothers

It is important to understand what tablets the pharmacist at the pharmacy might suggest - you can treat worms while carrying a child strictly with the medications prescribed by the attending doctor.
Taking into account all the characteristics of the patient’s disease, the doctor selects the most appropriate anthelmintic drugs for the given case. It is necessary to strictly adhere to the prescribed dosage and take the correct medicine.
Throughout the entire course of treatment for helminthiasis, the expectant mother should be under the close supervision of a doctor. A responsible and reasonable approach to the treatment of helminthic infestation while waiting for a child will be the key to a speedy recovery and a guarantee of future health for both the mother and her baby.









