What is amoebiasis?
Amebiasis , or amoebic dysentery , is an intestinal infection caused by a single-celled protozoan parasite (amoeba), which is characterized by deep ulcerative damage to the wall of the large intestine, and sometimes the liver and other organs. The disease is widespread, but is endemic in areas with hot climates.
Amebiasis is mainly common in areas with low levels of sanitary and hygienic standards. Most cases of infection are recorded in some areas of Africa, on the Hindustan Peninsula, as well as in some regions of Central and South America.
Worldwide, approximately 50 million people develop amoebiasis each year, and up to 100,000 of them die.
Treatment of amebiasis in children and adults
Treatment methods for amebiasis should be aimed at destroying all parasites in the body, restoring the loss of blood, electrolytes, fluid, as well as stopping the manifestations of the disease.
If treatment is incorrect, relapse is possible; if prevention is not followed, reinfection can occur. Treatment is carried out comprehensively, using combinations of drugs to destroy the pathogen throughout the body.
When treating a disease in children, hemoglobin levels should be monitored, since its decrease significantly aggravates the child’s condition. It is also necessary to constantly replenish fluid loss - children have a hard time with dehydration.
Drugs for the treatment of amoebiasis
Treatment of this disease is based on 3 types of drugs:
- Luminal (direct) amoebocytes - drugs that have a detrimental effect on the luminal forms of amoebae (Quiniophone, Yatren, Diiodoquinone, antibiotics of the tetracycline group). They are used to treat the disease in carriers and to prevent relapses.
- Universal amoebicides - affect all types of amoebae (Tinidazole, Furamide, Flagyl). They act at the cellular level, destroying the parasite from the inside.
- Tissue amoebocytes - have a detrimental effect on amoebae that are located on tissues and mucous membranes (Hingamin, Ambilgar, Dihydroemitin, Emetin). Used in the treatment of acute forms of the disease.
Cause and risk factors
The cause of amoebiasis is the entry into the human digestive tract of one of the varieties of amoebas, Entamoeba histolytica.
It exists in 2 forms:
- active vegetative form , which can exist in two types: large vegetative form (LVF) and small vegetative form (MVF). BVF resides in the thickness of the intestinal wall and consumes red blood cells; when BVF enters the intestinal lumen, it undergoes degenerative changes and turns into IMF, which is often found in the stool of a sick child.
- inactive form - cysts: the amoeba turns into this form under any unfavorable conditions; Amoebiasis spreads with the help of cysts.
BVF, or tissue form, is present only in the patient. IMF and cysts are present in amoeba carriers. The source of an amoebic infection is a person with amebiasis and a practically healthy carrier of amoebae. The disease is spread by food and water.
More significant is the waterway, in the absence of proper sanitary supervision of the water supply. The cause of infection may be a salad made from vegetables washed with water from a pond. Infection also occurs through ingestion of contaminated water while swimming.
Flies are carriers of infection.
If the vegetative form of amoebas gets into the products, the disease does not develop, since the amoebas die under the influence of hydrochloric acid contained in the gastric juice. Amebiasis develops when a product is infected with amoeba cysts.
Treatment
Amebiasis today is successfully treated with antibiotics. Additionally, mineral-containing drugs or droppers are prescribed to compensate for the lack of fluid. Sometimes a relapse of the disease is possible.
In case of relapse, intestinal obstruction may occur, which threatens the patient’s life, so it is necessary to operate.
The risk of contracting amoebiasis can be reduced by observing basic hygiene rules, drinking only boiled water and eating in trustworthy catering establishments.
If diarrhea begins with nagging abdominal pain, you should consult a doctor. In our area, amebiasis is rare. However, any infectious disease of the digestive tract can be serious and dangerous.
The doctor will conduct a laboratory examination of the stool using a microscope and culture the stool by placing it in an environment in which the pathogens will begin to grow. Then, after identifying the pathogen, he will prescribe treatment.
Signs and symptoms
The incubation period of amoebiasis is quite long: it lasts from 7 days to 3 months. The onset of the disease is acute. The patient may be bothered by a headache and severe pain in the left half of the abdomen. The temperature is normal. An increase in temperature may occur with a mixed infection (amoebiasis and bacterial infection).
One of the first characteristic signs of amoebiasis is the appearance of bloody diarrhea and an excruciating painful urge to defecate. The stool is liquid or pasty, very frequent, with mucus and blood in large quantities. The mucus has a glassy or jelly-like appearance. Blood mixes with mucus and as a result, the stool resembles “raspberry jelly.”
The patient's appetite is significantly reduced, people quickly lose weight and look emaciated. The skin becomes dry, wrinkled, and the stomach becomes sunken. With deep damage to the intestinal wall, intestinal bleeding may occur, sometimes severe, even leading to death of the patient.
The acute period of amebiasis can last up to 1.5 months and then become chronic. Amoebiasis is characterized by a tendency to chronicity of the process. In this case, the alternation of periods of exacerbation with periods of well-being continues for a number of years. Diarrhea alternates with constipation, and periodically there is bleeding in the feces. The body of children and the elderly is depleted much more than adults, severe malnutrition is noted, and anemia develops.
Intestinal amebiasis: diet for the intestines
Bifiform - stabilizes intestinal microflora.
After the full course of treatment for amoebiasis, the patient should remain under observation at the dispensary for another two weeks.
An important condition for the recovery period of the body after treatment is strict adherence to the diet and proper nutrition.
Most patients are under the misconception that if there is no diarrhea and no pain, then there is absolutely no need for a diet. This is a false conclusion.
It is important to realize that in an organism weakened by disease, the capabilities of the gastrointestinal tract are significantly reduced and their restoration occurs little by little. Despite the fact that the disease has been defeated, the patient still has disturbances in intestinal activity and enzyme secretion.
At this stage, it is mandatory to take medications that help stabilize the intestinal microflora that has been affected by the disease. These may be the following drugs: lactofiltrum, bifiform, acipol, etc.
Is milk allowed? Drinking milk is prohibited. This is due to the fact that many cannot digest it normally. But it is recommended to take fermented milk products, which are very rich in beneficial bacteria.
There are no contraindications for physical exercise. But, nevertheless, as after any infection, the body is quite weakened, and it is advisable not to do strong physical activity for several weeks.
In the period after intestinal amebiasis, you need to follow fractional meals. This means eating at least four small meals a day. Most people eat twice a day, but take large portions of food at one time.
You need to realize that the portion of food that was normal for your stomach and intestines before the period of illness will become excessively large after the illness and it will be difficult for the intestines to cope with it. The best option would be to divide a dish familiar to a person into several meals. This way the food will be absorbed much better.
The causative agents of the disease, amoebas, enter directly into the gastrointestinal tract.
People who have had intestinal amebiasis may experience constipation if they quickly return to their usual diet. For this reason, diet table No. 4, the so-called “intestinal table,” becomes a frequent prescription for doctors after this disease.
Diet restrictions apply to carbohydrates (baked goods, sweets) and fats. They are difficult to digest for a weakened body. A categorical ban on foods that irritate the stomach, namely spices, pickles, spicy foods, carbonated drinks. You should refrain from eating large amounts of fresh vegetables and fruits. The body, of course, needs vitamins, but after an illness the intestines have a hard time digesting fiber.
During the period of exacerbation of the disease, both fruits and vegetables are completely prohibited. Their return to the diet should happen little by little, starting with apples and eventually ending with melons. For several weeks after the patient has recovered, it is forbidden to supplement the diet with foods that the person has never consumed before.
It is allowed to eat soups, white and gray unsweetened bread, boiled vegetables, porridge (buckwheat, oatmeal, rice). You can eat lean meats and poultry without skin. Beef is preferable to pork. You should avoid barbecue for the first few weeks.
Read along with this article:
- Treatment of rotavirus infection and diet for intestinal flu
- Thrush in guys. The reason is dysbacteriosis???
- How is hepatitis B transmitted? What should you watch out for?
- Causes of appendicitis, as well as forms and symptoms...
- Rotavirus infection: signs of intestinal flu
- Symptoms of intestinal candidiasis, which contributes to the proliferation...
- Symptoms of salmonellosis in children, main features
- Protozoan cysts were found in the stool, what does this mean and how is it treated?
- Acute appendicitis: causes, types, symptoms
Complications
In addition to intestinal bleeding, anemia and malnutrition, amebiasis can lead to the following complications:
- appendicitis: develops when parasites penetrate the appendicular process;
- peritonitis: can develop when an amoeba penetrates the intestinal wall into the abdominal cavity; inflammation of the peritoneum occurs;
- abscess of the lungs, liver and/or other internal organs: can develop with any severity of amebiasis and during any period of the disease; abscesses can be single or multiple;
- paraproctitis: inflammation of the tissue around the rectum;
- narrowing of the intestinal lumen due to scarring of ulcers;
- ameboma: a tumor-like formation that in some cases forms in the intestinal lumen and leads to intestinal obstruction.
Diagnostics
To diagnose amoebiasis, the doctor needs to take stool samples from the patient. The best approach is to test the stool for protein produced by the amoebae (antigen test) or to detect the genetic material of the amoebae using polymerase chain reaction (PCR). The PCR method reproduces multiple copies of the amoeba's genetic material and thus makes amoebas easier to detect. These tests are more effective than examining stool samples under a microscope, the results of which are often questionable. In addition, microscopic examination may require three to six stool samples to detect amoebae, but even when detected, Entamoeba histolytica cannot always be distinguished from other species of amoebae, such as Entamoeba dispar, which have a similar appearance but a different genetic structure and are not causing diseases.
A flexible viewing tube (endoscope) may be used to view the colon. If sores or other signs of infection are found, an endoscope is used to obtain a sample of fluid or tissue from the infected area.
When amoebas travel beyond the intestines (for example, into the liver), they may no longer be found in the stool. Ultrasound, CT, or MRI tests may be ordered to confirm a liver abscess, but these types of tests do not indicate the cause. A blood test is performed to check for antibodies to amoebas. (Antibodies are proteins produced by the immune system to protect the body from attacks, including parasites.) Or, if the doctor suspects a liver abscess caused by amoebas, the patient may be prescribed drugs that destroy these microorganisms (amebocides). If the patient gets better, the most likely diagnosis is amoebiasis.
Dysenteric amoeba (Entamoeba histolytica)
Dysenteric amoeba
(lat.
Entamoeba histolytica
) - a type of amoeba, the causative agent of amoebiasis (amebic dysentery, amebic colitis).
Like other amoebas, Entamoeba histolytica
are single-celled organisms characterized by the presence of pseudopods that constantly change their shape, thanks to which the amoeba moves and captures food. Amoebas are characterized by the absence of a hard body shell. The amoeba cell is surrounded by a plasma membrane - an integral part of the living cytoplasm.
Dysenteric amoeba in the taxonomy of protozoa
The dysentery amoeba species belongs to the genus Entamoeba
, family
Entamoebidae
, order
Amoebida
, class
Archamoebae
, phylum
Amoebozoa
, kingdom protista (protozoa).
Various forms of dysenteric amoeba
Dysenteric amoeba can exist in three forms: tissue, luminal and cyst. The tissue form is found only in patients with amoebiasis, others are also found in carriers. Dysenteric amoeba cysts enter the human gastrointestinal tract with water or food. In the small intestine, under the influence of enzymes, the cyst shell dissolves and eight mononuclear amoebae are formed. As a result of subsequent divisions, they turn into vegetative luminal stages, trophozoites, ranging in size from 10 to 60 microns, on average 25 microns, having a single nucleus, the habitat of which is the lumen of the upper parts of the colon. As they move through the intestine, trophozoites transform into one to four-nucleated cysts (on average 12 μm in diameter), which are excreted in the feces.
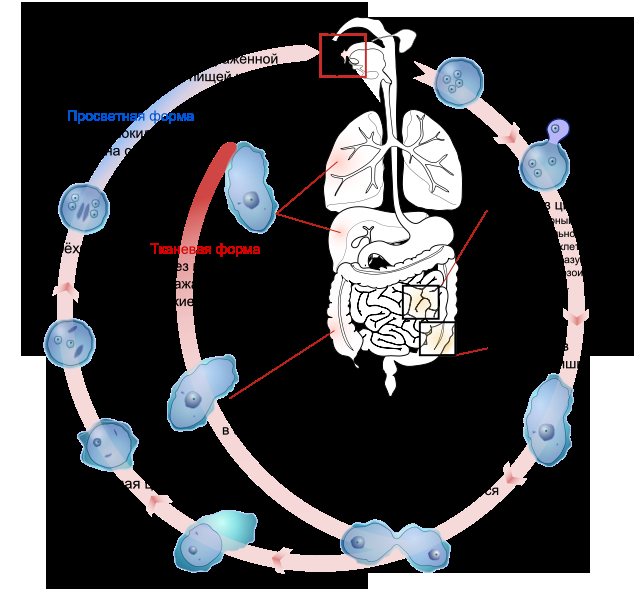
When entering the human body, dysenteric amoeba cysts can form invasive forms. In the development of invasive forms, parasite and host factors are important, such as: intensity of invasion, physicochemical environment of the intestine, immunodeficiency, starvation, stress and others. The invasive or so-called tissue stages of amoebas are larger than the luminal stages and are capable of attaching to the intestinal mucosa.
Dysenteric amoeba is a causative agent of human diseases.
Most strains of dysentery amoeba do not cause any disease in humans. At least 90% of dysentery amoeba infections are asymptomatic and should not be treated. Entamoeba histolytica
enters the intestine , in most cases it multiplies in the contents of the large intestine, without penetrating into tissues and without causing intestinal dysfunction (the person is healthy, but serves as a carrier of dysenteric amoeba).
Dysenteric amoeba can penetrate the mucous membrane of the colon, where neurohumoral substances are presumably produced that cause secretion in the intestine and its damage, resulting in inflammatory diarrhea. Diagnosis of the invasive form of the disease requires identification of hematophagous trophozoites in stool or colon ulcers. Manifestations of symptomatic amoebiasis include diseases such as mild refractory diarrhea, fulminant dysentery and liver abscess.
Amoebiasis is an uncommon cause of bloody diarrhea in young children, typically accounting for less than 3% of the disease. It is generally not recommended to treat young children with bloody diarrhea for amoebiasis. Such treatment is only possible based on the results of microscopic examination of fresh stool samples obtained in a reliable laboratory and identification of Entamoeba histolytica
in red blood cells, or when two different antibacterial drugs that are usually effective against
Shigella dysenteriae
in a given country are not clinically effective.
Some researchers believe that the difference between the high frequency of isolation of dysentery amoeba and, at the same time, the relatively low frequency of clinical manifestations is associated with the presence in the dysentery amoeba population of two types of amoebas - potentially pathogenic strains of Entamoeba histolytica
, and non-pathogenic
Entamoeba dispar
, which can only be distinguished by DNA analysis.
The main virulence factor in dysentery amoeba is cysteine proteinases, which are absent in Entamoeba dispar
.
At the same time, the differences in the pathogenicity of strains of dysenteric amoeba remain insufficiently studied. Nine potentially pathogenic strains of dysentery amoeba, and 13 non-pathogenic strains with different DNA, were identified.
WHO recommends for the treatment of diarrhea caused by Entamoeba histolytica
(dysenteric amoeba), take metronidazole three times a day for five days (for severe forms - 10 days) at 750 mg for adults and based on 10 mg per kg of weight for children
By Order of the Ministry of Health and Social Development of Russia No. 1664n dated December 27, 2011 “On approval of the nomenclature of medical services”, medical care is included in the nomenclature of medical services, section 26.
On the website GastroScan.ru in the “Literature” section there is a subsection “Parasitic and infectious diseases of the gastrointestinal tract”, containing publications for healthcare professionals on this topic.
Medicines active against dysenteric amoebas
Antiamoebic drug, intestinal antiseptic, acting on vegetative forms of amoebae - Intetrix.
The direct antagonists of dysentery amoeba are the unicellular fungi Saccharomyces boulardii
), used as an antimicrobial drug.
Antibiotics active against dysenteric amoeba (those described in this reference book): metronidazole, tinidazole, nifuratel, tetracycline, doxycycline. Lincomycin is not active against dysenteric amoeba.
Entamoeba histolytica and amoebiasis in ICD-10
Amoebiasis and Entamoeba histolytica
are mentioned in the International Classification of Diseases ICD-10 in “Class I. Some infectious and parasitic diseases” where in the block “A00-A09 Intestinal infections” for amoebiasis caused by
Entamoeba histolytica
, a three-character heading “A06 Amoebiasis” is allocated, containing the following four-character categories:
- A06.0 Acute amoebic dysentery. Acute amoebiasis. Intestinal amoebiasis, not otherwise specified
- A06.1 Chronic intestinal amoebiasis
- A06.2 Amebic non-dysenteric colitis
- A06.3 Intestinal ameboma. Ameboma, unspecified
- A06.4 Amoebic liver abscess. Hepatic amoebiasis
- A06.5 Amoebic lung abscess. Amoebic abscess of the lung (and liver)
- A06.6 Amoebic brain abscess. Amoebic abscess of the brain (and liver) (and lung)
- A06.7 Cutaneous amoebiasis
- A06.8 Amoebic infection of another location. Amoebic appendicitis. Amoebic balanitis
- A06.9 Amoebiasis, unspecified
Back to section
Forecast
If left untreated, amoebic infections have very high morbidity and mortality. In fact, the death rate is second only to malaria. Amebic infections tend to be most severe in the following populations:
- pregnant women;
- postpartum women;
- newborns;
- malnourished people;
- persons taking corticosteroids;
- persons with malignant neoplasms.
When the disease is treated, the prognosis is good, but in some parts of the world recurrent infections are common. Mortality after treatment is less than 1%. However, amoebic liver abscesses may be complicated by intraperitoneal rupture in 5–10% of cases, which may increase the mortality rate. Amoebic pericarditis and pulmonary amoebiasis have a high mortality rate exceeding 20%.
Today, with effective treatment, the mortality rate for patients with uncomplicated disease is less than 1%. However, rupture of an infected amoebic liver abscess leads to high mortality.
Intestinal amoebiasis: symptoms of the disease
To dispel doubts, you can do an ultrasound.
The basis for suspicion of amoebiasis can be considered the patient's fever, pain in the liver, or manifestations of jaundice. This kind of pain does not occur with typical liver inflammation.
If the liver abscess is superficial, it can be detected by palpation. The patient will feel sharp pain in the area where the abscess is located.
It is necessary to remember the primary symptoms of intestinal amebiasis. To avoid friction in the diagnosis, it is also necessary to do an ultrasound, because, for example, with inflammation of the bile ducts, similar pain and the presence of jaundice are possible.
Direct signs of intestinal amoebiasis are bloody stools and high fever. If you have the above symptoms, you should immediately seek medical help. The most appropriate thing to do would be to call an ambulance.
Amebiasis that is not treated can cause extremely sad consequences. In practice, cases that resulted in the death of the patient have not yet been recorded.
Prevention
A reliable method of preventing amoeba infection is to follow the rules of hygiene and sanitation.
Drinking water can be protected by boiling and using filters. Water should be stored in closed containers. Controlling flies and protecting food products from them is important for disease prevention. When swimming in bodies of water, do not swallow water. In endemic regions, boiled water should also be used when brushing teeth, washing dishes, and making ice cubes.
Don’t residents of Russia develop immunity to this disease?
In Russia we have not encountered histological amoeba.
When an individual encounters a new type of infection, falls ill and suffers this disease, the immune system “fixes” the pathogen that caused it and produces specific antibodies to fight it.
If the same infection enters the human body again, his immune system will already have a means of fighting it.
This means that the patient will either suffer a mild form of the disease or not become infected at all. Unfortunately, most of the residents of Russia have not encountered histological amoeba. For this reason, the disease is developing quite rapidly.