The essence of the procedure
Drainage of the gallbladder refers to routine surgical interventions, the purpose of which is to restore the bile flow, reduce the concentration of bilirubin in the blood, and evacuate bile from the liver tissue. If suturing the ducts is not indicated, such as after radical removal of the gallbladder (cholecystectomy), surgeons immediately begin to drain the organs of the hepatobiliary system. Installation of a drainage structure is often carried out laparoscopically, but if necessary, alternative methods that differ in surgical access are prescribed.
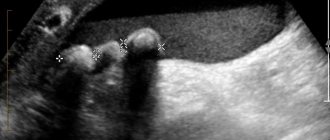
When the ducts are blocked, drainage is installed at the site of narrowing, which restores the patency of the lumens, improves the passage of bile, and relieves symptomatic manifestations such as acute pancreatitis. Endoscopic or laparoscopic operations are performed under the control of X-ray equipment or ultrasound, which ensures precision of manipulation and minimizes the risk of damage to healthy tissue.
How is obstructive jaundice of tumor etiology treated?
Currently, the most effective tactics to combat obstructive jaundice caused by compression of the bile ducts by tumors are drainage interventions on the bile ducts. As a rule, they are performed under the control of X-ray television and (or) ultrasound.
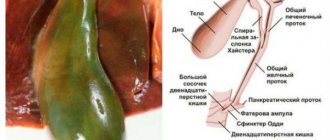
Most often, at the first stage, the bile ducts are punctured using a thin and long needle (Chiba needle) through the intercostal space. A special contrast agent is injected through a needle, which allows you to see the bile ducts themselves on an x-ray, as well as determine the level at which they are blocked. This intervention is called puncture cholangiography.
Then, using a special tool, it is possible to install a special drainage into the bile ducts. Drainage is distinguished:
- external - in which all bile is discharged only outside;
- and external-internal - in which the drainage is placed in such a way that the bile is evacuated both outward and in the natural direction, into the intestine.
As a rule, external-internal drainage is more physiological, since many important substances contained in bile, which are normally absorbed back in the intestine, are not lost.
In some cases, when tumor compression isolates several different segments of the biliary tree, multiple drains may be required.
Although drainage allows you to cope with the symptom itself, it significantly limits the patient’s quality of life - the drainage constantly irritates the abdominal wall, requires constant care, there is a risk of its displacement or even accidental removal, as well as the development of infectious complications at the site of erection.
To overcome these drawbacks of drainage, it was recently proposed to complete drainage interventions with bile duct stenting. The essence of stenting is to install a special (usually metal) endoprosthesis in the area of compression of the bile duct - a stent, which maintains the bile duct in an open state due to its high radial rigidity. In this case, the drainage tube can be removed completely, the outflow of bile will be carried out in the normal direction along the stent, or rather along the bile duct restored with the help of a stent.
Indications for drainage of the bile ducts
Speaking about drainage of the gallbladder and ducts, it is important to understand the advisability of performing the operation in a specific clinical case. Despite the routine nature, drainage is a full-fledged operation and includes a complex of treatment and rehabilitation measures. Indications for surgery are the following diseases and conditions:
- late stages of cholelithiasis with blockage of the lumens;
- neoplasms of an oncogenic or benign nature;
- exacerbation of cholecystitis;
- pathologies and developmental anomalies of the gallbladder and ducts.
Late stages of cholelithiasis are an indication for drainage of the bile ducts.
Drainage of the gallbladder for obstructive jaundice is prescribed for persons who are undergoing more serious operations on the gallbladder and organs of the hepatobiliary system as a whole. Also, drainage is indicated before intensive antibiotic therapy for chronic inflammation of the organ.
Drainage in patients with obstructive jaundice is justified in the absence of effectiveness from conservative treatment, although if the pathological process is reversible, adequate and timely drug therapy usually stabilizes bilirubin levels and normalizes the functional parameters of the gallbladder.
Gallbladder drainage
Often, pathologies of the biliary tract lead to a narrowing of the ducts that transmit bile to other organs and tissues.
In this regard, doctors resort to a method such as duct drainage, the main purpose of which is to expand them and help remove excess fluid.
What is gallbladder drainage, indications and contraindications for manipulation, its types are described in detail in this article.
The main purpose of duct drainage is to widen them and help remove excess fluid.
The essence of drainage of the bile ducts
Draining the gallbladder is the simplest and most reliable way to reduce the concentration of bilirubin in the blood, get rid of excess bile in the tissues and remove it from the liver.
If complete suturing of the duct is not indicated (for example, after cholecystectomy has been performed, after removal of the gallbladder), then proceed to drainage of the biliary system.
Most often, to install drainage, laparoscopy is performed - a surgical operation that involves inserting a catheter through specially designated points on the abdomen.
Drainage of the bile ducts involves creating drainage at the site of narrowing of the passage. This procedure is often performed under local anesthesia, less often performed under general anesthesia.
During an intervention on the gallbladder, sections of the ducts are removed using specially equipped systems, which are drained by specialists. To do this, methods such as radiography and ultrasound are used, which make it possible, using a contrast agent administered to the patient in advance, to accurately determine the location of the blockage of the passages.
After which, using a puncture, a needle is inserted into the patient’s common bile duct, which serves as a guide for installing a drainage tube. After performing this manipulation, mechanical cleaning is carried out through the installed device; how to clean these passages from excess fluid through the drainage is determined by the surgeon.
Indications for drainage of the bile ducts
Drainage of the common bile duct has its own indications and contraindications. So, start draining if necessary:
Drainage of the common bile duct has its own indications and contraindications
- Remove infected and stagnant fluid from the liver and passages.
- Eliminate narrowing of the lumen of the common bile duct and restore the passage of bile to other organs.
- Rinse the gallbladder and its passages with antiseptics or antibiotics.
- To avoid scar formation at the surgical site in the gastrointestinal tract.
- To prevent the formation of fistulas after surgery on the duct.
- To drain fluid from the liver to clean the bladder cavity.
The primary indications for surgical intervention are such pathologies and diseases of the gallbladder as:
- Gallstone disease - surgical intervention allows you to expand the lumen of the duct, which facilitates the passage of the stone. It is important to understand that after surgery to remove the gallbladder, drainage is not installed, but deep suturing of the ducts is performed.
- Cholecystitis in the acute stage - here intervention is indicated when the inflammatory process interferes with the drainage of fluid and its stagnation and infection occur.
- Obstructive jaundice - intervention is necessary to remove excess bilirubin and the outflow of enzymes from the liver.
- Tumors are the main cause of blocked passages.
- Pancreatitis - dilation of the ducts is indicated when swelling of the head of the pancreas occurs, which interferes with the flow of bile into the duodenum.
- Cholangitis and cysts on the ducts.
- An anomaly in the development of the gallbladder, which leads to congenital blockage of the ducts.
Also, expansion of the bile ducts can be carried out if it is necessary to introduce medications into the bile ducts, including antibacterial and antiseptics, and flush organs in order to improve the condition of the bile ducts.
Types of bile duct drainage
In the modern world, many types of drainage of the gallbladder have been developed. This allows surgical intervention to be performed in a variety of conditions, for various patient conditions.
Today, the classification of drainage installation procedures has the following structure:
- External drainage - in this case, the device is installed in such a way that excess bile is drained outside into the collection through conductors. Through this catheter, the gallbladder can be flushed and medications can be administered. Such drains can be easily removed when the indications resolve.
- External-internal - a method that allows most of the bile to be released into the intestines, while its excess enters the external receiver, removed through a catheter from the organ. This drainage requires a puncture; puncture of the tube can lead to serious consequences for the body.
- Internal (percutaneous) expansion is a modern internal prosthesis made of special material, which is installed in the ducts on a permanent basis, serves for constant expansion of the ducts and optimal removal of enzymes. At the same time, during the operation, the CBD duct is monitored to monitor how much bile is secreted in a person per day, and then the catheter is removed, and the endoprosthesis remains inside.
To determine the method of drainage, it is necessary to take into account all indications for drainage of the common bile duct, correctly assess the patient’s condition and the need to install one or another drainage.
External drainage of the bile ducts
In the modern world, many types of drainage of the gallbladder have been developed.
External drainage of the common bile duct consists of inserting a rubber tube into the bile ducts and liver, while the outer end of the drainage remains visible to the human eye. After inserting this tube, a receiver is attached to the outer end, collecting all the bile. If necessary, this receiver can be replaced and the drainage and ducts can be flushed.
External drainage is a method of temporary use that allows not only to prepare the patient for the procedure on the gallbladder , but also to remove the formed stones and scars from the ducts through this tube. The indication for insertion of an external catheter is also the preparation of the patient for insertion of an internal prosthesis into the ducts.
The advantage of this procedure is that this operation does not cause major trauma and can be performed on patients of any condition. Installation of such a catheter for bile drainage significantly reduces the risk of developing renal and liver failure and contributes to the rapid improvement of the patient’s condition after the procedures.
This method quickly leads to the removal of fluid from the body and the formation of dehydration in the organs, so its installation is possible only for a short time. The maximum time for which this catheter is inserted is 2 weeks, after which there is a high risk of complications, which requires removal or replacement of the drainage.
External and internal drainage
This method is the most preferable, since in this case part of the bile is excreted naturally because it enters the intestines, where a certain amount of useful substances is absorbed and absorbed by the body.
The essence of internal and external drainage is that a drainage tube is passed through the gallbladder into the intestine, while part of the catheter is left outside with a receiver connected to it. So, part of the bile enters the intestine, and the other part, if it is impossible to exit into the intestine, enters the receiver.
This type is most often used before preparing the patient for the procedure and for performing an operation to introduce permanent drainage, as well as when the bile ducts are under compression for a long time. Even if the bile is removed from the gallbladder, the tube remains forever in the gallbladder.
Percutaneous drainage
This type is often used to provide palliative care to patients with inoperable tumors and anomalies in the development of the biliary tract. In this case, a prosthesis is installed in the area of the organ stricture, which ensures optimal outflow of fluid from the ducts.
The essence of the internal endoprosthetics method is that a person under anesthesia and under the control of equipment is inserted into the duct through which an internal prosthesis is inserted into the duodenum and duct, installed above the site of blockage or narrowing of the duct. A drainage bag for bile is installed on this cutting. After about a day, this catheter is removed, and the prosthesis remains in the gallbladder so that the enzyme flows normally into the intestines.
In order to optimize bile output, the tube is securely secured . To drain excess fluid, the patient is asked to purchase a bile drainage bag that is attached to the outer end. Before removing the drainage tube, the bile bag is removed and removed along with the catheter.
Contraindications to drainage
Drainage of the gallbladder has a number of contraindications that limit the range of people eligible for this procedure.
So, installing drainage is possible if a person does not have:
Obesity is a contraindication for drainage installation
- Blood clotting disorders.
- Accumulation of fluid in the peritoneum and severe stage of liver failure.
- Oncological process in the stage of metastasis.
- The presence of tumor-like formations along the path of drainage installation.
- Pregnancy in late gestation.
- Obesity.
- Cardiac and respiratory disorders.
These contraindications must be observed, since performing the procedure in their presence can lead to the development of complications such as infections, bleeding and insufficient effectiveness of the procedure.
Drainage of the bile ducts in obstructive jaundice
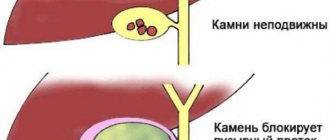
Obstructive jaundice occurs when bilirubin stagnates in the blood. Its causes may be narrowing of the passages, tumors, inflammatory and infectious diseases of the bile-forming organs.
In this case, a person develops symptoms characteristic of pathology - the skin and mucous membranes become yellow, itching and symptoms of intoxication occur.
This disease requires immediate medical intervention, including surgery.
Most often, with obstructive jaundice, to improve the outflow of fluid, they resort to a drainage method such as external, since when this pathology is cured, the drainage can be removed and the natural outflow of the enzyme can be ensured.
Drainage of the gallbladder in obstructive jaundice can be carried out using the same methods as in the case of other pathologies of the gallbladder. The doctor decides what type of drainage to install, depending on the patient’s condition and the cause of the disease.
Indications for drainage in obstructive jaundice
Obstructive jaundice does not always require drainage. Depending on how much fluid is excreted by the patient’s organ and the person’s condition, specialists may resort to conservative treatment of the pathology. If complications develop or the situation worsens, doctors decide whether surgery is necessary.
The main indications for drainage in obstructive jaundice are:
- Damage to the common duct.
- Pancreatitis and cholecystitis in the acute stage.
- Purulent processes in the gallbladder.
- Tumors.
- Stone formation.
Drainage of the bile ducts in obstructive jaundice is indicated when there is a violation of the outflow of fluid from the organ, with the accumulation of a large amount of bilirubin in the human blood.
During the procedure, it is important to monitor the patient’s condition to prevent the catheter from becoming dislodged or damaged - this can lead to serious complications, leading to irreversible consequences and death of the patient.
Gallbladder drainage.
Types and techniques of the drainage process
The main purpose of installing drainage is to restore the flow of bile to the duodenum. With congestion, acute pain occurs in the right hypochondrium, discomfort during meals, sour vomiting, and malaise. The key symptom is severe pain, especially as the stones begin to move through the ducts. If the stones do not pass through the flow paths on their own, and the condition is not controlled with medication, surgical intervention is prescribed.
External drainage
External drainage of the bile ducts is used in most cases. The advantage of this type of intervention is the ability to control the volume of bile secretion, evaluate the structure and presence of impurities (blood, pus). Guiding catheters are installed to the site of stenosis, which are removed through the peritoneum or the area of the right hypochondrium and fixed with a sterile bandage. Bile is discharged into special containers, which are also fixed externally. Any medications can be administered through the probe and rinsing can be carried out unhindered.
In patients with an external drainage system, enzyme medications are indicated, and to maintain normal digestive function, bile is introduced into the intestinal tract. After the conductivity of the ducts is restored, the catheter is removed and the hole is sutured.
External-internal
Drainage of the common bile duct is carried out using the external-internal method. The drainage is installed so that a certain volume of bile enters the intestinal tract. Excess bile secretion is discharged into the bile receptacle, fixed externally. The operation is performed using a targeted puncture method under ultrasound control. This method should only be performed by highly qualified specialists to avoid serious complications caused by damage to the drainage catheter.
Percutaneous drainage
Percutaneous drainage (otherwise known as internal endoprosthetics) is usually performed in inoperable cases, as a form of palliative care for seriously ill people, as well as in cases of abnormal development (shape, size, fusion) of the gallbladder and ducts. A special prosthetic frame is installed at the site of stenosis, through which the normal outflow of bile secretion occurs.
The method consists of inserting a prosthesis into the duodenum and duct and installing it just above the site of stenosis. A catheter is inserted through this prosthesis. A special bag is installed on the prosthesis to collect bile. After 1-2 days, the catheter is removed, and the prosthesis and bile reservoir remain for the normal flow of secretions into the intestinal tract.
The result of successful drainage of the bile ducts is considered to be the normalization of bilirubin levels due to the normalization of its indicators. In gastroenterology and hepatology, drainage provides the following positive results:
- formation of prerequisites for returning to the stage of the recovery period after operations, chemotherapy or radiation therapy;
- saving lives in acute cholecystitis and increasing hyperbilirubinemia;
- increasing the patient's life expectancy.
Early drainage of the bile ducts and bladder in case of an inoperable oncogenic tumor can increase the patient's life expectancy to 1.5-2 years.
Reasons for using your own bile

Obstructive jaundice is one of the serious diseases of the digestive tract. It is associated with a violation of the flow of substances from the bile ducts into the duodenum. Unable to get into it, the liver secretion leaks into the blood. The body is poisoned.
In blood tests, this is reflected by an increased level of bilirubin, an agent that utilizes dead red blood cells. Pathology can occur in anyone.
Most often, the disease is provoked by:
- Gallstone disease, when the formed stones interfere with the normal circulation of bile, blocking its flow.
- The presence of tumors and other neoplasms that also block the path to liver secretions.
- Pancreatitis, in which the pancreas increases in size.
- inflammatory processes or the presence of scars on the mucous membrane covering the duodenum.
- Presence of parasites in the liver
- Cholangitis, expressed by inflammation of the bile ducts and leading to their narrowing.
- Congenital pathologies leading to obstruction of the bile ducts.
Only some of the listed diseases (pancreatitis, parasitic diseases) can be treated with conservative methods. For this purpose, suitable enzymatic, antibacterial, anti-inflammatory, and anthelmintic drugs are selected. In other cases, the patient is indicated for gallbladder drainage.
There are several types of operation:
- External drainage, when the bile enters a special receiver. To replenish the necessary elements of the secretion, you need to take it internally.
- External internal drainage. The main part of the bile enters the duodenum, and a small amount of secretion flows out into the receiver. The remainder gives an idea of the patency of the bile ducts. Doctors estimate the amount of bile by drainage.
- Internal drainage involves endoprosthetics. It is usually used for inoperable tumor processes.
With external or external-internal drainage, as much bile is released into the system per day as could not enter the duodenum.
Drainage prevents fluid from entering the blood. However, not all the bile reaches the intestines, but it should. Therefore, when collecting it externally, it is often recommended to drink liquid. Why this is needed is clear. But how to make the process easier, because bile has a sharp, unpleasant taste...
Contraindications
Despite the routineness and effectiveness of the manipulation, any surgical intervention should be considered from the perspective of the risks of complications, foreseen and unforeseen consequences. There are a number of relative and absolute contraindications to the manipulation. In the first case, the operation is performed after drug preparation, at a suitable period or under the responsibility of the surgeon. In the second case, alternative ways to restore the bile duct are sought:
- poor blood clotting and other diseases of the hematopoietic system;
- severe liver damage, organ failure, cirrhosis;
- cancer tumor with metastases;
- overweight, obesity degree III-IV;
- heart defects, cardiomyopathies, heart failure;
- 3rd trimester of pregnancy.

Surgical intervention is not performed for obstructive jaundice after recent surgical procedures. Surgery is not performed on persons in serious condition, in medically induced coma, or in intensive care and resuscitation wards due to other pathological conditions. The drainage procedure is mainly planned; the patient is carefully examined for possible contraindications.
In any case, the need and advisability of drainage of the bile ducts is assessed by the doctor based on the medical history and current examinations, and the general condition of the patient.
Obstructive jaundice in oncology
The pathogenesis of jaundice in oncology is simple. The tumor grows and compresses the blood vessels and bile ducts. Stagnation of bile occurs. The patient will notice such a symptom as yellow skin. Then itching appears. The patient scratches the skin and creates an entry point for infection.
With this disease, the liver cannot cope with large amounts of bilirubin, it poisons the entire body. The development of obstructive jaundice in oncology leads to death. Such a patient requires surgical intervention, but no surgeon will perform an operation until the symptoms of jaundice are relieved.
Klatskin tumor is a rare oncological pathology that affects the bile duct. There are 4 stages. The first signs appear in the later stages. When diagnosing the fourth stage, treatment does not bring results. Symptomatic therapy is prescribed.
For cancer of the tail and body of the pancreas, these organs and the gallbladder are removed. Sometimes the spleen is removed along with them. They live on average 10-12 months after surgery. After the intervention, 10-12% of patients die.
Possible complications
Obstructive jaundice due to obstruction of the bile ducts is a life-threatening complication. In the absence of therapy, severe organ pathologies develop. Thanks to drainage, you can quickly free the bile lumens from stones, restore the normal passage of bile secretions, and reduce the load on the organs of the hepatobiliary system.
Usually, compliance with all the rules of surgical technique reduces the risk of complications, but they are not excluded during the course of the intervention. The negative consequences of the procedure are:
- hemorrhages, hematomas;
- peritonitis - acute inflammation of the membranes of the abdominal cavity, generalized sepsis;
- severe pain;
- development of postoperative cholangitis;
- displacement of the drainage unit, catheter, prosthetic frame;
- local suppuration in the area where the tube was inserted.
Normally, pain and hyperemia in the area of the puncture or incision persist for 5-7 days after the intervention, residual symptoms disappear by the tenth day. If the pain syndrome increases, the wound at the catheterization site suppurates, and bleeds, then it is important to consult a doctor for further investigations.
Symptoms
A medical history is a protocol for examining a patient, where a description of all symptoms is recorded. Clinical signs develop slowly. Often, inflammation of the biliary tract occurs first. The clinic includes:
- Pain in the area of the right hypochondrium.
- Increase in body temperature.
- General weakness.
- Poor appetite.
- Headache.
Then a yellow coloration of the skin and mucous membranes occurs. Other signs of pathology:
- Pain in the right hypochondrium.
- Dark urine and discolored stool.
- Itching.
- Dyspeptic disorders.
- Poor appetite and weight loss.
- Increased body temperature.
- Enlargement of the liver.

With obstructive jaundice, the patient must receive prompt medical attention. Otherwise, due to the massive death of hepatocytes, liver failure is possible. Symptoms appear:
- Severe weakness.
- Drowsiness.
- Coagulopathic bleeding.
The progression of liver failure leads to brain damage. Multiple organ failure is observed. If there is a blockage of the bile ducts, then spastic, sharp pain appears, radiating to the chest area, right armpit and shoulder blade.
External signs are revealed 1-2 days after the hepatic colic subsides. The liver is painful. If you press in the area of the right hypochondrium, an involuntary holding of breath occurs.
Pancreatic cancer causes a dull pain that radiates to the back. A distended bladder can be felt, pressing on which does not cause pain. The liver increases in size and becomes dense. Itching and poor appetite appear first.
An enlarged liver is a common symptom of prolonged obstructive jaundice. This occurs due to a large amount of bile and inflammation of the bile ducts.
One of the first signs is itchy skin. It cannot be treated. Scratches and bruises appear on the skin. Weight loss is observed with jaundice due to cancerous tumors.
Body temperature is elevated and does not fall. This is a specific sign of subrenal jaundice, distinguishing it from viral hepatitis.

Subrenal jaundice in a patient
Recovery period and care features
The early recovery period requires hospital conditions, where the patient is constantly monitored by medical personnel, providing the necessary local care and antibiotic therapy. In case of deterioration, the patient will receive immediate assistance. The early postoperative period includes the following activities and appointments:
- a course of antibiotic therapy to suppress the inflammatory process;
- regular dressings and rinsing to prevent infection;
- instillation of antiseptic solutions into the cavity of the gallbladder.
Much attention is paid to nutrition. For several days after the operation, pureed lean food and plenty of drinking are recommended to reduce the digestive load and gradually launch the digestive systems. In the first days, patients are given strict bed rest, so the bed should be comfortable, the sheets should be stretched so that folds do not form, which contribute to the development of bedsores.
After the operation, hygiene and antiseptics of the installed drainage catheter are required, which is removed after 14-17 days if the bilirubin level is satisfactory according to blood tests
The late recovery period requires compliance with an adequate diet, sleep and wakefulness. Physical activity is gradually introduced. Patients are advised to take walks in the fresh air. After surgery, patients are placed for follow-up with gastroenterologists, hepatologists, and, if tumors are present, with oncologists.
Preventive measures
The outcome of surgery is influenced by a number of external and internal factors, but usually obstructive jaundice gradually resolves. As you recover, it is necessary to eliminate the risks of relapse and follow clinical recommendations:
- nutrition correction;
- reduction of stress factor;
- exclusion of alcohol, smoking;
- creating conditions for moderate physical activity;
- weight loss with the help of nutritionists.

Patients are often prescribed a long course of choleretic drugs and enzymes to improve digestive processes. The course of drug therapy should be systemic and regular. Correction of conservative therapy is carried out only by the attending physician based on bilirubin level indicators.
What is obstructive jaundice and its causes?
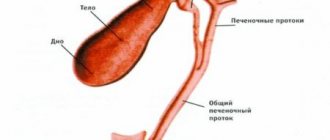
The hepatobiliary tract is a system that includes several organs: liver, bile ducts, gallbladder. Inside the liver, pigments and acids are secreted, which mix with water to form bile. This substance subsequently enters the bladder through the ducts, and from there into the intestines, where it takes part in digestion.
With obstructive jaundice, bile is not removed from the liver. This is caused by pathologies in which the patency of the biliary tract is impaired. As a result, the substance stagnates in the liver.
One of the functions of bile is to remove excess bilirubin from the liver. As part of this substance, bilirubin passes through the intestines and subsequently leaves it with feces. If the outflow is impaired, cholestasis develops - stagnation of bile in the liver. This inevitably leads to an increase in the level of bilirubin, which, penetrating into the blood, causes jaundice.
- Cholecystitis
- Pancreatitis
- Hepatitis
- Cirrhosis
- Tumor neoplasms (oncology, cysts, polyps)
- Parasitic infestation
- Inflammation of the lymph nodes in the area of the bile ducts
The mechanism of development of pathology is complex. In most cases, it is associated with an ongoing inflammatory disease. Due to inflammation, edema develops, affecting the patency of the bile ducts. As a result, stagnation occurs.
The nuances of drainage after cholecystectomy
Cholecystectomy is an operation to remove the gallbladder due to acute duct obstruction and severe digestive disorders. The operation, performed according to indications, significantly improves the quality of life of patients and does not significantly affect digestive functions. According to statistics, 95% of patients who have undergone cholecystectomy experience a disappearance of symptoms observed before surgery.
Surgical intervention to excise the gallbladder along with the ducts is performed laparoscopically or openly, as well as using minimally invasive techniques. The choice of removal method is based on multiple clinical criteria.
After cholecystectomy, surgeons resort to drainage against the background of acute cholecystitis, carcinoma, and cholelithiasis.
Drainage is performed laparotomically or laparoscopically. All drains after open cholecystectomy are removed 8-10 days after surgery, and in weakened patients or against the background of an oncological process - on 12-14 days. To reduce the risk of inflammation, bile is collected into a special reservoir through a catheter brought out. The area near the installation of the drainage tube is treated with zinc liniment and antiseptics. Fistulography is regularly performed through the drainage to assess the conductivity of the ducts. When draining during cholecystectomy, drainage is removed no earlier than 3 weeks after the procedure.
Drainage of the gallbladder is an important surgical intervention that restores the gallbladder, improves the general well-being of patients, and normalizes the quality of life. In the absence of treatment, against the background of acute stagnation of secretions in the bile ducts, life-threatening consequences develop, including death.
Types of operations
Nutrition starts on the second day. Eat simple food for the postoperative period. On this day you will have to limit yourself to low-fat light broth, fruits, light cottage cheese, yogurt.
It is recommended to take food in small quantities, with great frequency: 5-7 meals.
After three days, you can start eating everyday foods. Rough foods, fatty, fried foods, spices, and sauces are excluded. It is not recommended to consume products made from rye flour, or anything that promotes the secretion of bile or gas formation.
It is recommended to switch to nutrition according to therapeutic diet No. 5.
Completely postoperative pain disappears after 24-96 hours. If during this period the pain does not go away, but on the contrary, intensifies, a doctor’s consultation is necessary. Underwear should be soft, should not press or rub the puncture site.
Drainage
In most cases, drainage is required. Its main purpose is to ensure reliable outflow of bile and fluid. Drainage prevents stagnation. If the formation of fluid has decreased and restoration processes have begun, the drainage can be removed.
The sutures, unlike abdominal surgery, are small and compact. They do not exceed 1.5-2 cm in diameter. The sutures are removed as the incisions heal. If healing is good, the sutures are removed on the second day; if the speed of recovery processes is low, removal is carried out approximately on the 7-10th day. It all depends on the individual characteristics of the patient.
The scars after laparoscopy are insignificant, not exceeding 2 cm in size. Four scars remain after the operation. They heal quickly.
How long do you have to lie down after gallbladder removal surgery?
The patient should lie down for a 4-6 hour period. Then you can rise and make slow movements. Quite often they are discharged from the hospital even on the day of surgery.
After a routine uncomplicated laparoscopic cholecystectomy, the patient is transferred from the operating room to the intensive care unit, where he spends the next 2 hours of the postoperative period to monitor adequate recovery from the state of anesthesia.
In the presence of concomitant pathology or characteristics of the disease and surgical intervention, the duration of stay in the intensive care unit may be increased. The patient is then transferred to a ward where he receives the prescribed postoperative treatment.
During the first 4-6 hours after surgery, the patient should not drink or get out of bed. Until the morning of the next day after the operation, you can drink plain water without gas, in portions of 1-2 sips every 10-20 minutes with a total volume of up to 500 ml.
The patient can get up 4-6 hours after surgery. You should get out of bed gradually, first sit for a while, and, in the absence of weakness and dizziness, you can get up and walk around the bed.
It is recommended to get up for the first time in the presence of medical personnel (after a long stay in a horizontal position and after the action of medications, orthostatic collapse - fainting) is possible.
The next day after the operation, the patient can move freely around the hospital, begin to take liquid food: kefir, oatmeal, diet soup and switch to the usual regime of drinking liquids. In the first 7 days after surgery, the consumption of any alcoholic beverages, coffee, strong tea, drinks with sugar, chocolate, sweets, fatty and fried foods is strictly prohibited.
The patient's diet in the first days after laparoscopic cholecystectomy may include fermented milk products: low-fat cottage cheese, kefir, yogurt; porridge with water (oatmeal, buckwheat); bananas, baked apples; mashed potatoes, vegetable soups; boiled meat: lean beef or chicken breast.
In the normal course of the postoperative period, the drainage from the abdominal cavity is removed the next day after surgery. Removing the drainage is a painless procedure; it is performed during dressing and takes a few seconds.
In the first month after surgery, the functions and general condition of the body are restored. Careful adherence to medical recommendations is the key to full recovery of health. The main areas of rehabilitation are adherence to physical activity, diet, drug treatment, and wound care.
In the hospital, special stickers will be applied to postoperative wounds located at the places where instruments are inserted. It is possible to take a shower with Tegaderm stickers (they look like a transparent film), while Medipore stickers (a white patch) must be removed before showering.
You can shower starting 48 hours after surgery. Getting water on the seams is not contraindicated, but you should not wash the wounds with gels or soaps or rub them with a washcloth.
After taking a shower, you should lubricate the wounds with a 5% iodine solution (or Betadine solution, or brilliant green, or 70% ethyl alcohol). Wounds can be treated using the open method, without dressings.
Taking baths or swimming in pools and ponds is prohibited before the sutures are removed and for 5 days after the sutures are removed.
Sutures after laparoscopic cholecystectomy are removed 7-8 days after surgery. This is an outpatient procedure, the sutures are removed by a doctor or a dressing nurse, and the procedure is painless.
As soon as the patient has learned that surgery is indicated as the only effective treatment, and the date is already known, it is worth starting preparations. First, the doctor must explain how long the rehabilitation period after cholecystectomy will take. The length of your stay in a hospital bed may vary depending on the size of the incision.
Typically, the patient is provided with a list of things to prepare upon admission to the surgical department.
Diet after gallbladder laparoscopy is a major aspect of recovery. A well-structured diet helps prevent gastrointestinal upset, which is a common manifestation after cholecystectomy.
Up to 4 months you should stick to the following diet:
- lean meat, boiled or steamed;
- boiled white fish meat;
- vegetables, preferably potatoes, carrots and zucchini;
- fresh berries and fruits;
- weak tea, vegetable juices and fruit drinks.
You should forget about baking, fried foods, and fatty dairy products. It is better to eat “yesterday’s” bread. As a dessert, you can prepare yourself a baked apple with cottage cheese, compotes, and jelly. You need to eat in small portions, at least 5-6 times a day.
It is necessary to reduce the consumption of foods high in cholesterol. The daily portion of butter should not exceed 20 grams. You need to buy low-fat dairy products.
It is important to chew food slowly, this will awaken the enzymes necessary for digestion. All these recommendations are designed to help the liver.
However, many patients ignore these rules and begin to eat whatever they want. This attitude towards your body will not lead to anything good. In medical practice, there are cases when a patient after cholecystectomy was again admitted to the hospital for rehabilitation several months later. A return to a normal diet should take more than a year.
And, of course, you should forget about alcohol forever. Recovery after surgery is a long journey towards your health. Of course, this requires patience and endurance, however, in order to prevent serious complications, you need to try.
Physical activity plays an important role in restoring the body. Immediately after surgery, loads should be limited to subjective sensations, then you can include warm-up and walks in the fresh air. The core muscles should not be strained earlier than after a year. Pleasant emotions are the best medicine for a person undergoing surgery.
Currently, laparoscopic removal of gallstones is very rarely used. This phenomenon is due to the fact that the chronic course of cholelithiasis is associated with disorders in cholesterol metabolism and surgery does not make much sense, since a relapse will occur after a certain period of time.
Cholecystectomy is used to treat diseases such as:
- chronic calculous inflammation of the gallbladder;
- cholesterosis;
- gallbladder polyposis;
- acute inflammation of the gallbladder;
- asymptomatic stone carriers.
General contraindications to laparoscopy are diseases such as malignant tumors, cardiac and pulmonary decompensation, and general peritonitis. The minimally invasive method is not used in people who are overweight and in pregnant women in late gestation.
Also, laparoscopic cholecystectomy is not performed for people who have an abscess (purulent inflammation with the formation of a limited infiltrate) of the gallbladder, with severe scars in the area of the organ, or with acute pancreatitis (inflammation of the pancreas. The operation is not indicated for people with a pacemaker and obstructive jaundice.
Laparoscopy, despite the considerable trauma, is a serious surgical intervention, therefore, before the operation, preparations must be made for the removal of the gallbladder. It includes a full diagnostic examination of the body’s condition. The patient must donate blood for a general and biochemical analysis, which evaluates the functioning of the liver, kidneys, pancreas and the presence of inflammatory reactions.
The patient also needs to submit a urine sample for a general analysis, which helps analyze kidney function. Before the operation, the surgeon needs to know whether the patient has blood-borne infections: AIDS and HIV, syphilis, hepatitis. The patient must also donate blood for a coagulogram - a test characterizing the state of the blood coagulation system.

Among the instrumental examination methods, the obligatory ones are an electrocardiogram (assessment of heart function), fluorography (assessment of the condition of the lungs), FGS or EGDS (assessment of digestive function). The patient is carefully examined by a surgeon, therapist, and anesthesiologist. If he has chronic diseases, it is mandatory to see a doctor who treats the affected organ.
The day before surgery, eating after six o'clock in the evening is prohibited. The patient should not drink 8 hours before the upcoming laparoscopy. During a planned admission, the patient is given two enemas: in the evening the day before the intervention and in the morning before the operation. 7 days before the proposed laparoscopy, you should stop taking blood thinners and non-steroidal anti-inflammatory drugs, which will help avoid bleeding.
Typically, cholecystectomy is performed under general anesthesia using a special mask. This type of anesthesia helps to achieve a complete absence of unpleasant sensations and prevents unwanted movements of the patient during the operation.
After removal of the gallbladder, the patient is transported to the ward, where he recovers from anesthesia. At this time, he may be bothered by nausea, headaches, poor health, and a feeling of “overwhelm.” Bed rest is recommended for 8 hours, then the patient can sit down and perform simple manipulations in a lying position. Doctors advise not to get out of bed for the rest of the day. You can drink water 4-5 hours after laparoscopy.
The first few days the patient is often bothered by pain in the area of the surgical wounds; they usually go away after 3-5 days. Any physical activity after removal of the gallbladder is allowed only after a week; until this point the patient is prohibited from lifting weights.
In the absence of complications, the temperature after removal of the gallbladder remains normal, or rises on the first day to 37.5 degrees, and then drops to 36.6.
To prevent postoperative infectious complications, the patient is prescribed broad-spectrum antibiotics. Analgesic non-narcotic drugs are used to relieve pain. According to indications, doctors may prescribe intravenous infusions. The time for removing sutures depends on the type of material; most often this manipulation is performed after 1-2 weeks.
| Advantages | Laparoscopy of the gallbladder | Operation through an incision |
| Less traumatic intervention | 4 punctures of 1 cm each. | The incision is 20 cm long. |
| Lower blood loss | During laparoscopy of the gallbladder, the patient loses on average 30-40 ml of blood. | Blood loss is significantly greater. |
| Shorter rehabilitation times | The patient is discharged from the hospital after 1-3 days. | The patient is discharged from the hospital after 1-2 weeks |
| Faster recovery | Performance is fully restored within a week. | Recovery takes 3-6 weeks. |
| Less pain after surgery. | As a rule, ordinary painkillers are sufficient to relieve pain. | Sometimes the pain is so severe that the patient has to be prescribed narcotics. |
| Lower incidence of postoperative complications. | Adhesions and hernias form much less frequently after laparoscopy. |
Currently, the following types of surgical interventions are performed for diseases of the gallbladder:
- Laparoscopic cholecystectomy – removal of the gallbladder laparoscopically. This is one of the most common interventions in endoscopic surgery.
- Choledochotomy is a dissection of the common bile duct.
- Anastomosis is the creation of communications between the bile ducts and other organs of the digestive system to improve the outflow of bile.
Indications for laparoscopic cholecystectomy
Indications for making an incision and performing an open operation:
- On the day of surgery, the patient is usually allowed to stand up, walk and eat liquid food.
- The next day you can eat normal food.
- Approximately 90% of patients can be discharged within 24 hours after surgery.
- Within a week, performance is restored.
- Small bandages or special stickers are applied to postoperative wounds. The stitches are removed on the 7th day.
- After surgery, you may experience pain for some time. To relieve them, regular painkillers are used.
Complications are possible with any operation, and laparoscopy of the gallbladder is no exception. Compared to open surgery through an incision, interventions using endoscopy have a very low risk of complications - only 0.5%, that is, in 5 out of 1000 operated on.
Regardless of the type of planned intervention, be it laparoscopy or abdominal removal of the gallbladder, the indications for surgical treatment are:
- Cholelithiasis.
- Acute and chronic inflammation of the bladder.
- Cholesterosis with impaired bile excretion function.
- Polyposis.
- Some functional disorders.
Gallstone disease is usually the main reason for most cholecystectomies. This is due to the fact that the presence of stones in the gall bladder often causes attacks of biliary colic, which recurs in more than 70% of patients. In addition, stones contribute to the development of other dangerous complications (perforation, peritonitis).
In some cases, the disease occurs without acute symptoms, but with heaviness in the hypochondrium and dyspeptic disorders. These patients also require surgery, which is performed as planned, and its main purpose is to prevent complications.
Gallstones can also be found in the ducts (choledocholithiasis), which poses a danger due to possible obstructive jaundice, inflammation of the ducts, and pancreatitis. The operation is always complemented by drainage of the ducts.
The asymptomatic course of gallstone disease does not exclude the possibility of surgery, which becomes necessary with the development of hemolytic anemia, when the size of the stones exceeds 2.5-3 cm due to the possibility of bedsores, with a high risk of complications in young patients.
Cholecystitis is an inflammation of the gallbladder wall, occurring acutely or chronically, with relapses and improvements replacing each other. Acute cholecystitis with the presence of stones is a reason for urgent surgery. The chronic course of the disease allows it to be carried out plannedly, possibly laparoscopically.
Cholesterosis is asymptomatic for a long time and can be detected by chance, and it becomes an indication for cholecystectomy when it causes symptoms of gallbladder damage and disruption of its function (pain, jaundice, dyspepsia). In the presence of stones, even asymptomatic cholesterosis serves as a reason to remove the organ. If calcification occurs in the gallbladder, when calcium salts are deposited in the wall, then surgery is mandatory.
The presence of polyps is fraught with malignancy, so removal of the gallbladder with polyps is necessary if they exceed 10 mm, have a thin stalk, or are combined with cholelithiasis.
Open surgery
For the best treatment outcome, it is important to conduct adequate preoperative preparation and examination of the patient.
For this purpose, the following is carried out:
- General and biochemical blood and urine tests, tests for syphilis, hepatitis B and C;
- Coagulogram;
- Clarification of blood type and Rh factor;
- Ultrasound of the gallbladder, biliary tract, abdominal organs;
- ECG;
- X-ray (fluorography) of the lungs;
- According to indications – fibrogastroscopy, colonoscopy.
Some patients need consultation with specialized specialists (gastroenterologist, cardiologist, endocrinologist), all – with a therapist. To clarify the condition of the biliary tract, additional studies are carried out using ultrasound and radiopaque techniques. Severe pathology of internal organs should be compensated as much as possible, blood pressure should be brought back to normal, and blood sugar levels should be monitored in diabetics.
Preparation for surgery from the moment of hospitalization includes eating a light meal the day before, completely refusing food and water from 6-7 pm before the operation, and in the evening and morning before the intervention the patient is given a cleansing enema. In the morning you should take a shower and change into clean clothes.
If it is necessary to perform an urgent operation, the time for examinations and preparation is much less, so the doctor is forced to limit himself to general clinical examinations and ultrasound, allocating no more than two hours for all procedures.