Every person has at least once encountered patients with diabetes mellitus and knows that this pathology requires replacement therapy with a special substance - insulin. But what is insulin, and why is it beneficial for high blood sugar?
Insulin (hormone) is a biologically active protein substance produced by the pancreas to regulate metabolism in tissues. This hormone is mainly responsible for lowering blood glucose levels by accelerating glycogen synthesis.
Protein structure and composition
Insulin is a protein hormone. The molecular structure of this protein consists of two polypeptide chains, which are formed from amino acid residues. In total, both chains contain 51 amino acid residues: 21 of them are contained in the A-chain, 30 in the B. For the first time, the exact sequence of amino acid parts was determined by the English molecular biologist Frederick Sanger.
The chains are connected to each other by two covalent bonds between sulfur atoms (disulfide bridges), which are part of the amino acid cysteine. Another disulfide bond is found in the smaller chain of insulin. The spatial structure of the substance was determined using X-ray diffraction by biologist Dorothy Crowfoot-Hodgkin.
Not only was insulin the first hormone for which a complete primary structure was determined, but it is still the most studied of all endocrine gland products.
The structure of insulin is similar in animals, but even small differences affect how humans perceive the hormone. For example, the hormone that regulates glucose levels in the pig differs in only one amino acid residue located at the terminal (30th) position of the B-chain, namely alanine, which replaces threonine.
Insulin from animals belonging to cattle (for example, bovine) differs in three amino acids. Protein produced by other animals (including whale) is even less similar in primary structure.
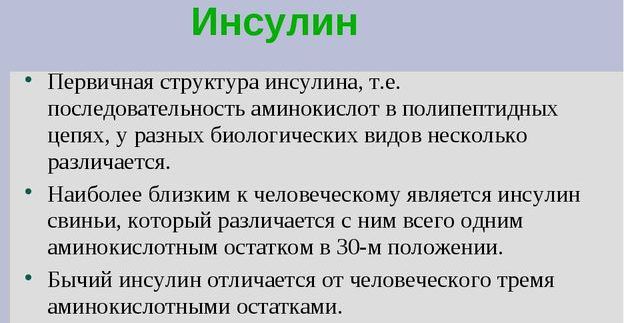
Due to the content of foreign amino acid residues, insulin from other biological species can cause an allergic reaction. Its intensity depends on the degree of difference between the proteins.
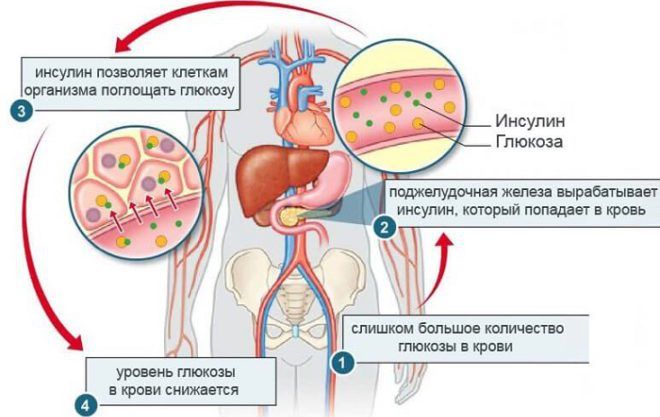
How glucose levels are regulated

Beta cells respond to blood glucose levels. When glucose levels rise, beta cells stimulate the production of insulin. Insulin-dependent muscle and fat tissues are especially sensitive to the amount of glucose. They account for about two-thirds of the cellular mass in the human body.

If insulin is a pancreatic hormone that functions to lower blood glucose levels, then all other hormones perform the opposite function, increasing it.
Hormonal regulation is also carried out by:
- glucagon;
- adrenalin;
- glucocorticoids;
- somatotropin.
In addition to the most important task of lowering sugar levels, the effect of insulin on the body is as follows:
- Increases cell permeability for glucose to penetrate into them.
- Promotes the absorption of proteins.
- Provides synthesis of fatty acids in the liver.
- Helps regeneration processes.
- Helps absorb microelements.
- Prevents fatty acids from entering the bloodstream.
How is this hormone produced?
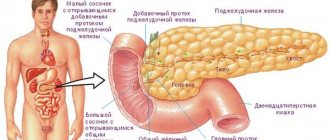
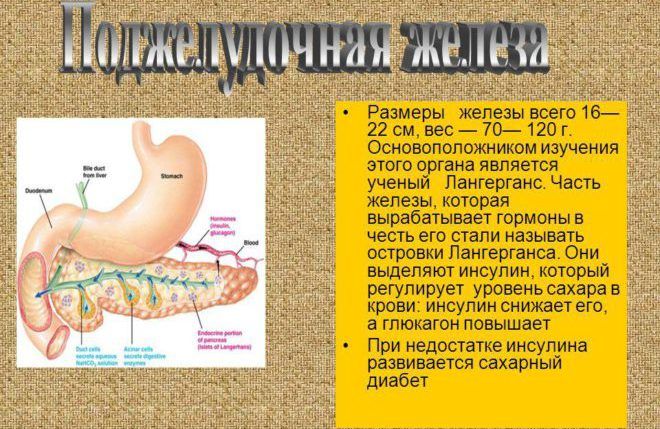
Insulin is produced in certain structures of the pancreas called the islets of Langerhans-Sobolevsky (sometimes only the first researcher is mentioned). This explains the etymology of the name of the hormone: translated, the Latin word Insula means “island”.
Initially, insulin synthesis is encoded by a gene located on the short arm of the eleventh chromosome. However, the peptide substance produced on ribosomes is a precursor of proinsulin - the so-called. immature form of the hormone. In addition to the necessary A and B chains, the preproinsulin molecule contains L- and C-peptides, consisting, respectively, of 24 and 31 amino acid residues.
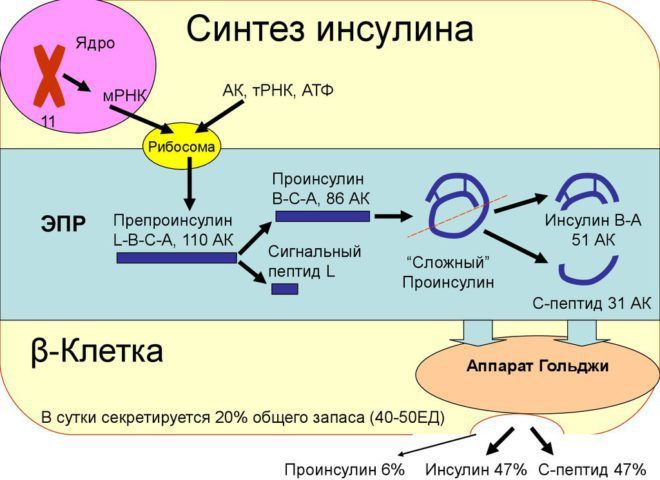
The L-chain is necessary for the free passage of the synthesized hormone through the lipid barrier (membrane), therefore proinsulin is formed almost immediately after the synthesis of the precursor.
After this, the molecules of the formed substance are transported to the Golgi complex, in which the so-called maturation of insulin. This stage is the longest in the process of formation of the active hormone. During maturation, the C-chain is cut out of the proinsulin structure, which connects the A- and B-peptides: thus, the molecules are separated into an inert residue and insulin.
The finished substance is stored in the secretory granules of the islets of Langerhans: combining with active zinc ions, insulin forms solid hexameric aggregates with a crystalline structure.
The beta cells of these formations are sensitive to increased glucose concentrations in the bloodstream. Secretion of the hormone insulin by the pancreas occurs in stages:
- Glucose is transported into β-cells by a special protein.
- The monosaccharide is oxidized to form ATP (a substance that is a source of energy for body systems). The amount of ATP synthesized depends on the amount of glucose.
- The generated ATP stimulates the closure of potassium channels in cells and the opening of calcium channels.
- An increase in calcium levels activates one of the types of phospholipases, which leads to an even greater increase in calcium concentration in the cell.
- A sharp increase in the amount of calcium ions stimulates the release of insulin stored in secretory granules.
The granule is degraded during passage of the plasma membrane. Changing the properties of the medium leads to the detachment of zinc and inactive parts.
When there is too much insulin
When the pancreas produces an increase in the hormone, the cells produce too much of the substance, which leads to health problems. Therefore, it is necessary to reduce the resulting productivity of the hormone in the body.
The formation of pancreatic production in a large volume of insulin is recorded when there are severe liver diseases, Cushing's pathologists.
It is possible that at a high level, painful changes are stimulated, for example, polycystic ovary syndrome in women. A characteristic sign of pancreatic disease is increased deposition of fat reserves in the peritoneal area, and abdominal obesity is formed.
If the indicator is in excess, wounds, cracks, and scratches take a long time to heal, so it is important for diabetic patients not to damage the skin. The tissues will take a long time to recover, hurt, and the wounds will become inflamed and fester. Also, according to this scheme, an excess of the indicator leads to the appearance of gangrene of the legs due to varicose veins and trophic abscesses.
If the indicator is too high, glucose drops to a minimum, the patient will experience outbreaks of hunger, frequent pulsation, rapid heartbeat, and fainting.
Insulin is a hormone that regulates the presence of sugar and is involved in the production of enzymes. If there is a discrepancy with the norm, then this signals the presence of a disease that requires urgent elimination.
The content of the article:
Insulin is a protein hormone produced by the pancreas. Its main role is to transport glucose to the body tissues and maintain its level in the blood at an optimal level. Insufficient insulin production leads to disruption of metabolic processes in the body and the development of diabetes mellitus. We will learn further how to organize proper nutrition to prevent disease and what foods will help the pancreas produce insulin.
Functions of peptide hormone
The main functions of insulin in the human body:
- Enhancing the absorption of glucose and other essential substances by the cells of insulin-dependent organs (liver, muscle tissue, fat layer).
- Activation of enzymes playing key roles in monosaccharide oxidation. Many of the effects of insulin in the human body are realized solely due to the hormone’s ability to influence enzyme activity.
- Increasing the intensity of glycogen production - a polysaccharide that stores glucose in liver and muscle cells for further use. Insulin stimulates the storage of monosaccharide by polymerizing it.
- Inhibition of gluconeogenesis (formation of glucose in the liver from proteins and fatty acids).
When there is a lack of insulin, signals from the control organ (brain) stimulate the production of glucose from existing reserves of fatty acids and protein tissue. The process is energetically unfavorable for the body, so tissues capable of absorbing ketone bodies are transferred to this food source, and the resulting glucose goes to the brain and other tissues, which can only receive energy from the oxidation of the monosaccharide.
The inability to absorb glucose by the cells of insulin-dependent organs leads to their starvation and increased synthesis of ketone bodies. This explains the smell of acetone from the mouth due to a lack of carbohydrates in the diet or pathologies associated with low insulin production. Increasing the concentration of insulin to an acceptable level in combination with a nutritious diet suppresses the synthesis of ketone bodies, which have a toxic effect on the tissues of the central nervous system.
With a large amount of simple carbohydrates in the diet, blood sugar rises and falls sharply. The production of insulin and the inhibition of its secretion after a decrease in glucose levels to an acceptable level occurs with some delay. As a result, frequent jumps in the concentration of the hormone can provoke a violation of tissue sensitivity to insulin, which is extremely undesirable.

The functions of insulin in the human body are not limited to the regulation of glucose metabolism. This hormone also has anabolic and anti-catabolic effects: it suppresses the degradation of proteins and the breakdown of fats, enhances the absorption of certain amino acids and the transport of phosphate, magnesium and potassium ions into cells, and stimulates the synthesis of protein and fatty acids.
Disease Prevention
Having figured out where insulin is produced, how insulin is produced in the human body, you should learn to take measures to prevent diseases associated with the pancreas.
Insulin is a hormone of the pancreas, in humans it is formed in response to an increase in sugar levels in the bloodstream, therefore, to prevent disorders, it is necessary to prevent changes in glycemia and adhere to the rules of a healthy diet.
It is noteworthy that with a well-chosen diet, it is possible to restore the functioning of a weakened organ and maintain its natural functioning in order to prevent health problems.
Endocrinologists and nutritionists recommend avoiding or limiting as much as possible unhealthy foods that negatively affect the condition of the pancreas:
- semi-finished products;
- fried foods;
- conservation;
- sweets;
- hot spices.
You need to rely on fresh vegetables, fruits, natural unsweetened fruit juices, cereals and dairy products. Improves body function if you drink up to 2.5 liters of water per day.
Quitting bad habits, namely smoking and drinking alcohol, helps greatly facilitate the functioning of the pancreas. With prolonged exposure to negative factors, the body becomes heavily clogged with toxic substances; a person suffers from seemingly unreasonable hormonal imbalances, which threaten not only diabetes, but also no less dangerous diseases.
Doctors advise from time to time to cleanse the body of harmful substances, carry out general health improvement, and reduce the negative impact on the pancreas. For these purposes, folk remedies and medications are indicated that significantly simplify the task.
Patients are often diagnosed with an inflammatory process in the organ (pancreatitis), the course of the disease is unpleasant, and the outcome can be sad. Inflammation can occur in chronic and acute forms; destructive processes are observed in the tissues of the organ itself, obstructing the functioning of the kidneys, lungs, liver, heart and brain.
In the acute course of the pathology, there is a threat to the patient’s life; inflammation occurs unexpectedly and often results from:
- excessive consumption of alcoholic beverages;
- the presence of stones in the ducts.
Symptoms of the disease in this case will be: upset stool, vomiting, attacks of nausea, severe pain in the back, lower hypochondrium of the abdominal cavity.
If the patient is bothered by such symptoms, he needs to refuse to eat and go to the clinic for diagnostics of the body.
It is important to remember that the cells that produce insulin die forever.
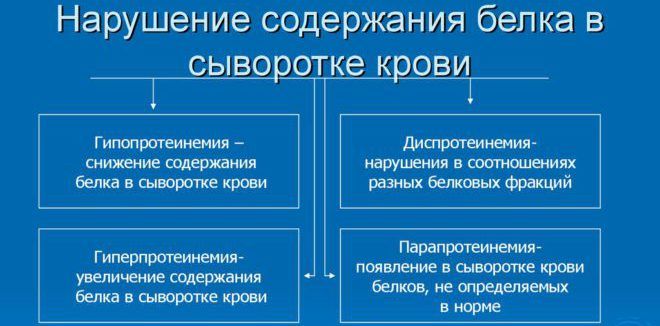
Disorders associated with a lack or excess of protein
The main diseases that are in one way or another associated with the production of insulin include diabetes mellitus, insulinoma and chronic overdose syndrome, which is characteristic exclusively for patients who have taken drugs of this hormone in excess doses for a long time.
Type 1 diabetes mellitus is a disease characterized by abnormally low insulin production and impaired carbohydrate metabolism as a consequence of the underlying pathology. The disease develops due to the destruction of pancreatic β-cells by the patient's immune system. At the moment, there are no active treatments for type 1 diabetes; drug courses are limited to nutritional control, supportive insulin therapy, taking vitamin-mineral complexes and restorative antidiabetic drugs.
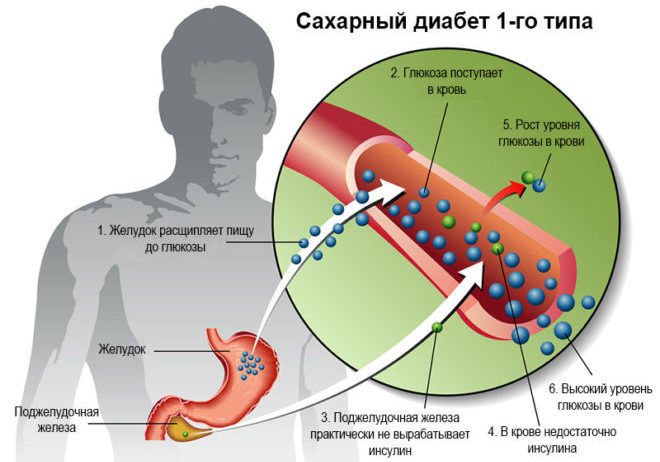
Type 1 and type 2 diabetes should not be confused. In the first case, the disorder is a consequence of insufficient production of the hormone, and in the second, a reduced sensitivity of insulin-dependent tissues to its action. In type 2 diabetes, constant insulin therapy is often not necessary.
If an excess of the drug is administered, the patient may develop insulin shock - a set of symptoms indicating hypoglycemia (excessively low blood glucose levels). More often, the pathological condition caused by an excess of administered insulin is called hypoglycemic coma.
Within a few minutes after a sharp drop in blood sugar levels, loss of consciousness and even paralysis of some brain centers may occur. Because of its potent effects on the central nervous system, insulin shock therapy has been used in the last century to treat several psychiatric conditions.
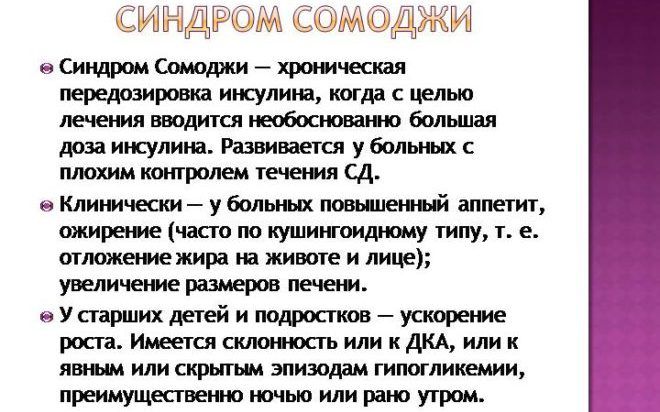
Somogyi syndrome, unlike insulin shock, does not occur with a single injection of an excess amount of insulin, but with regular excess of the hormone dosage. In medical practice, this symptom complex is also called “chronic insulin overdose syndrome.”
Insulinoma is a benign neoplasm of the beta cells of the gland that produces this hormone. The tumor tissue produces an excess amount of insulin, which can lead to all the symptoms of hypoglycemia, including loss of consciousness due to a lack of glucose in the tissues of the central nervous system.
DIAGNOSTICS OF PANCREAS FUNCTION
LIST OF STUDIES:
- Insulin (IRI)
- Autoantibodies to insulin A-IAA
- C-peptide
- Leptin (eating behavior hormone)
- Glycosylated hemoglobin (HbA1C)
- Cholesterol
- Cholesterol-HDL
- LDL cholesterol
Leptin
Hormone that regulates energy metabolism and body weight
Leptin is a peptide hormone that is secreted by fat cells and is thought to be involved in the regulation of body energy metabolism and body weight. It reduces appetite, increases energy expenditure, alters fat and glucose metabolism, and neuroendocrine function either by direct influence or by activation of specific structures in the central nervous system.
The level of leptin in the blood increases with increasing obesity and decreases with a decrease in the amount of adipose tissue. Normally, an increase in leptin levels suppresses the secretion of neuropeptide Y in the hypothalamus, which is involved in the formation of hunger, and stimulates the activity of the sympathetic nervous system. A decrease in leptin levels after significant weight loss causes an increase in appetite and subsequent weight (body weight) restoration.
Changes in leptin levels are associated with the mechanisms of development of amenorrhea caused by anorexia nervosa, bulimia nervosa, as well as excessive physical activity in female athletes. In these situations, leptin levels are reduced.
It is assumed that leptin concentration plays the role of a physiological signal about the sufficiency of the body's energy resources to perform the reproductive function and affects steroidogenesis in the ovaries. During puberty, the concentration of leptin in the blood increases.
Genetic deficiency of leptin (the synthesis of which is associated with the ob-gene - the obesity gene) in rare cases of hereditary leptin deficiency in humans causes morbid obesity, which can be treated with the use of exogenous leptin.
In other cases, obese people are characterized, on the contrary, by an increase in leptin concentration, which is not accompanied by a corresponding change in eating behavior and energy metabolism. Presumably, this is due to “leptin resistance,” which is associated with impaired transport of the hormone by transport proteins or soluble leptin receptors. Currently, it is considered as one of the factors in the pathogenesis of non-insulin-dependent diabetes mellitus. Excess leptin leads to suppression of insulin secretion, causes resistance of skeletal muscles and adipose tissue to its effects, suppresses the effect of insulin on liver cells, which leads to an even greater increase in glucose levels in type II diabetes.
However, obesity itself does not lead to diabetes with normal pancreatic function.
In addition, high leptin levels create a high likelihood of thrombosis. Research shows that a blood clot begins to form as a result of a special interaction between leptin and its receptors located on platelets, the cells responsible for blood clotting.
It has been established that the connection between the amount of leptin and diseases of the cardiovascular system exists regardless of other risk factors such as smoking, high cholesterol and high blood pressure.
Indications for the purpose of analysis:
- Suspicion of genetic leptin deficiency (previous occurrence of severe obesity);
- In a complex of studies on the problems of weight gain or loss;
- Reproductive function disorders due to reduced nutrition and excessive physical activity;
- In a complex of studies related to the identification of risk factors for cardiovascular diseases;
- Differential diagnosis of type II diabetes mellitus and obesity;
- Recurrent thrombosis.
Preparing for analysis:
At least 8 hours pass between the last meal and blood collection (preferably at least 12 hours). Juice, tea, coffee (especially with sugar) are not allowed. You can drink water.
Material: serum or blood plasma (without hemolysis and lipemia).
Units of measurement: Units of measurement in BioTest: ng/ml.
Reference values: Adults: Women – 1.1 – 27.6 ng/ml; Men – 0.5 – 13.8 ng/ml.
Increased leptin values:
- Obesity, non-insulin-dependent diabetes mellitus;
- Enhanced nutrition.
Decreased leptin values:
- Starvation;
- Weight loss; (body weight);
- Obesity associated with genetic leptin deficiency.
C-Peptide
Biologically inactive marker of carbohydrate metabolism, an indicator of endogenous insulin secretion.
C-peptide is a stable fragment of endogenously produced proinsulin, “cut off” from it during the formation of insulin. The level of C-peptide corresponds to the level of insulin produced in the body.
In the proinsulin molecule between the alpha and beta chains there is a fragment consisting of 31 amino acid residues. This is the so-called connecting peptide or C-peptide. During the synthesis of the insulin molecule in the beta cells of the pancreas, this protein is excised by peptidases and, together with insulin, enters the bloodstream. Until the C-peptide is removed, insulin is not active. This allows the pancreas to store insulin in the form of a pro-hormone. Unlike insulin, C-peptide is biologically inactive. C-peptide and insulin are secreted in equimolar quantities, so determining the level of C-peptide allows assessing insulin secretion.
It should be noted that although the amount of C-peptide and insulin molecules formed during secretion into the blood is the same, the molar concentration of C-peptide in the blood is approximately 5 times higher than the molar concentration of insulin, which is apparently due to different rates of elimination of these substances from the bloodstream . Measuring C-peptide has several advantages over measuring insulin: The half-life of C-peptide in the circulation is longer than that of insulin, so C-peptide levels are a more stable indicator than insulin concentrations. In immunological analysis, C-peptide does not cross-talk with insulin, so measurement of C-peptide makes it possible to assess insulin secretion even while taking exogenous insulin, as well as in the presence of autoantibodies to insulin, which is important when examining patients with insulin-dependent diabetes mellitus.
The level of C-peptide changes in accordance with fluctuations in the level of insulin produced endogenously. The ratio of these indicators may change against the background of liver and kidney diseases, since insulin is metabolized primarily by the liver, and the metabolism and excretion of C-peptide is carried out by the kidneys. In this regard, the determination of this indicator may be useful for the correct interpretation of changes in insulin levels in the blood in cases of liver dysfunction.
Indications for the purpose of analysis:
- Differential diagnosis of diabetes types 1 and 2;
- Prediction of the course of diabetes mellitus;
- Infertility, polycystic ovary syndrome;
- Differential diagnosis of hypoglycemic conditions;
- Suspicion of artificial hypoglycemia;
- Assessment of residual beta cell function in diabetics during insulin therapy;
- Detection and control of remission (juvenile diabetes);
- Diagnosis of insulinoma;
- Assessment of possible fetal pathology in pregnant women with diabetes;
- Assessment of insulin secretion in liver diseases;
- Control after removal of the pancreas.
Preparation for the study: on an empty stomach.
- Material for research: serum.
- Determination method: solid-phase chemiluminescent immunoassay.
- Units of measurement and conversion factors: Units of measurement in the BioTest laboratory - pmol/l
- Alternative units of measurement are ng/ml; Unit conversion: ng/ml x 331 ==> pmol/l
Reference values: 298-1324 pmol/l
Increased C-peptide levels:
- Beta cell hypertrophy;
- Insulinoma;
- Antibodies to insulin;
- Non-insulin-dependent diabetes mellitus (IDDM type II);
- Hypoglycemia when taking oral hypoglycemic drugs (sulfonylurea derivatives);
- Somatotropinoma;
- APUDhome;
- Kidney failure; 9. Eating; 10. Taking medications containing estrogens, progesterone, glucocorticoids, chloroquine, danazol, ethinyl estradiol, oral contraceptives.
Decrease in C-peptide levels:
- Insulin-dependent diabetes mellitus (IDDM type I);
- Insulin therapy (normal reaction of the pancreas in response to the administration of exogenous insulin);
- Alcoholic hypoglycemia;
- State of stress;
Antibodies to insulin receptors (for insulin-resistant type II diabetes mellitus).
Glycated hemoglobin (HbA1c)
A combination of hemoglobin with glucose, which allows one to assess the level of glycemia 1-3 months prior to the study.
It is formed as a result of the slow non-enzymatic addition of glucose to hemoglobin A contained in red blood cells. Glycated (the term “glycosylated” is also used) hemoglobin is present in the blood of healthy people.
The rate of this reaction and the amount of glycated hemoglobin formed depend on the average level of glucose in the blood over the life of red blood cells. As a result of the reaction, several variants of glycated hemoglobins are formed: HbA1a, HbA1b, HbA1c. The latter form predominates quantitatively and gives a closer correlation with the severity of diabetes mellitus.
Glycated hemoglobin reflects hyperglycemia that occurred during the life of red blood cells (up to 120 days). Red blood cells circulating in the blood have different ages. Usually they focus on an average period of 60 days. The level of glycated hemoglobin is an indicator of compensation of carbohydrate metabolism during this period. Normalization of the level of glycated hemoglobin in the blood occurs 4-6 weeks after reaching normal glucose levels. In patients with diabetes mellitus, the level of this compound can be increased by 2-3 times.
In accordance with WHO recommendations, this test is considered optimal and necessary for the control of diabetes mellitus. Patients with diabetes are recommended to test their glycated hemoglobin levels at least once a quarter.
Values may vary between laboratories depending on the analytical method used, so monitoring over time is best done in the same laboratory or at least using the same method. When monitoring diabetes treatment, it is recommended to maintain glycated hemoglobin levels below 7% and review therapy when glycated hemoglobin levels exceed 8% (these values apply only to certified methods for determining glycated hemoglobin with reference limits of 4-6%).
Clinical studies using certified methods show that a 1% increase in glycated hemoglobin is associated with an average increase in plasma glucose levels of approximately 2 mmol/L. Glycated hemoglobin is used as an indicator of the risk of developing diabetes complications. It has been proven that a decrease in glycated hemoglobin values by 1/10 is associated with an approximately 45% reduction in the risk of progression of diabetic retinopathy.
Test results may be falsely affected by any condition that affects the average lifespan of red blood cells. Bleeding or hemolysis causes a false decrease in the result; blood transfusions naturally distort the result; in iron deficiency anemia, a false increase in the result of determining glycated hemoglobin is observed.
Indications for the purpose of analysis
Long-term monitoring of the course and control over the treatment of patients with diabetes mellitus to determine the degree of compensation of the disease.
Preparing for the study
It is advisable to take blood samples on an empty stomach. The study is not advisable to conduct after bleeding or blood transfusions.
- Material for research: whole blood with anticoagulant (EDTA).
- Determination method: borate method.
- Execution time: 1 working day.
- Units of measurement and conversion factors: units of measurement in the BioTest laboratory are % of the total amount of hemoglobin.
- Reference values: 4.5-6.5% of the total hemoglobin content.
Increased HBA1c values:
- Diabetes mellitus and other conditions with impaired glucose tolerance.
- Iron deficiency.
- Splenectomy. A false increase may be due to a high concentration of fetal hemoglobin (HbF).
Decrease in HBA1c values:
- Hypoglycemia.
- Hemolytic anemia.
- Bleeding.
- Blood transfusion.
Normal blood protein levels
Insulin production is controlled by blood glucose levels. The normal sugar level for humans is up to 5.4-5.6 mmol/l. If the result is 5.6-6.6 mmol/l, doctors recommend a special diet with a reduced amount of carbohydrates (especially simple ones - sugar, bread, sweet fruits, etc.).
If the sugar level exceeds 6.7 mmol/l with the following test techniques, it is necessary to conduct additional diagnostics and prescribe adequate antidiabetic or other therapy.
If sugar levels are high, the patient is given a glucose tolerance test. The normal result is 7.7 mmol/l and below; an intermediate value, indicating metabolic disorders, is 7.8-11.1 mmol/l. A result above these indicators indicates diabetes. Too low values may indicate malnutrition or pathology. In children, a low glucose concentration is a normal variant due to the underdevelopment of the central nervous system and rapid metabolism.
Blood for testing glucose levels is taken on an empty stomach or at least an hour and a half after the last meal. Violation of this rule makes the result useless for diagnosis.
Insulin levels are rarely examined directly; this analysis is an additional diagnostic method. The normal concentration of the hormone is 3-28 µU/ml. Fetal development provokes an increase in the level of the hormone in the blood due to the relationship with growth hormone, so in pregnant women the result may be slightly higher (on average from 6 µU/ml).

Changes in insulin production - causes, symptoms and consequences
The pancreas is the second largest gland, its weight is 60-100 g, length 15-22 cm.
The endocrine activity of the pancreas is carried out by the islets of Langerhans, which consist of different types of cells. Approximately 60% of the pancreatic islets are β cells. They produce the hormone insulin, which affects all types of metabolism, but primarily reduces the level of glucose in the blood.
Table. Pancreatic hormones
Insulin (polypeptide) is the first protein produced synthetically outside the body in 1921 by Baylis and Bunty.
Insulin dramatically increases the permeability of the muscle and fat cell membrane to glucose. As a result, the rate of glucose transfer into these cells increases approximately 20 times compared to the transfer of glucose into cells in the absence of insulin. In muscle cells, insulin promotes the synthesis of glycogen from glucose, and in fat cells - fat. Under the influence of insulin, the permeability of PєР»РµС‚очной мембраны also increases for amino acids, from which proteins are synthesized in cells.
Rice. The main hormones that affect blood glucose levels
The second pancreatic hormone, glucagon, is secreted by islet a-cells (approximately 20%). Glucagon is a polypeptide in chemical nature, and an insulin antagonist in physiological effects. Glucagon enhances the breakdown of glycogen in the liver and increases plasma glucose levels. Glucagon promotes the mobilization of fat from fat depots. A number of hormones act like glucagon: growth hormone, glucocorticoids, adrenaline, thyroxine.
Table. Main effects of insulin and glucagon
| Type of exchange | Insulin | Glucagon |
| Carbohydrate | Increases the permeability of cell membranes to glucose and its utilization (glycolysis) Stimulates glycogen synthesis Inhibits gluconeogenesis Reduces blood glucose levels | Stimulates glycogenolysis and gluconeogenesis Has a counter-insular effect Increases blood glucose levels |
| Protein | Stimulates anabolism | Stimulates catabolism |
| Fatty | Inhibits lipolysis The number of ketone bodies in the blood decreases | Stimulates lipolysis The amount of ketone bodies in the blood increases |
The third pancreatic hormone, somatostatin, is secreted by 5 cells (approximately 1-2%). Somatostatin inhibits the release of glucagon and the absorption of glucose in the intestine.
Insulin production by the pancreas decreases for a variety of reasons. Of course, it stops due to a malfunction of the organ. The pancreas stops working for a reason, there is a certain root cause. The main one is a bad habit, when a person often overeats, eats food with a high calorie content, and the menu contains foods with a large amount of refined carbohydrates.
Why doesn't the pancreas produce insulin? These can be infectious and chronic diseases, which lead to weakening of the body and lower immunity. The amount of hormone is adversely affected by:
- stress;
- neuroses;
- neurological diseases.
stressful state
There may be a lack of hormone in the bloodstream, but glucose saturation will not increase. This indicates problems with the endocrine structure of the pancreas, which requires consultation with an endocrinologist.
The process of hormone production is disrupted in the presence of certain diseases of the pancreas. In particular, pancreatitis leads to changes in organ tissue. As a result of inflammation, the cells responsible for the production of enzymes and hormones die and are replaced by connective tissue.

If you notice symptoms of changes in your blood insulin levels, be sure to visit your doctor.
As a result, not only exocrine insufficiency occurs (problems with the production of food enzymes). The pancreas is unable to produce insulin in the required quantity.
However, not all patients develop pathology in exactly this sequence. It happens that patients who have already been diagnosed with type 2 diabetes begin to suffer from pancreatitis.
Increased production can be provoked by various factors:
- irregular and unbalanced diet, rich in simple carbohydrates;
- increased physical and mental stress;
- obesity;
- deficiency of vitamin E and chromium.
The level of the hormone can rise due to diseases of the pancreas (we are talking about a violation of the endocrine function of the organ), liver and tumors in the abdominal cavity, as well as during pregnancy. Low indicators can indicate either banal physical exhaustion (extreme fatigue) or the onset of diabetes.
Behind the lack of insulin is the death of the beta cells that synthesize it due to attacks by one’s own immune system. With a lack of pancreatic hormone insulin, cells are unable to absorb glucose, and blood sugar levels continue to remain much higher than acceptable limits.
Types of industrial hormone
Types of insulin are classified according to several criteria: degree of purification, type of animal, duration of action, etc.
Human insulin and its genetically engineered analogues are more suitable for use in replacement therapy than drugs of animal origin.

Depending on the duration of exposure, the following types of insulin are distinguished:
- Fast-acting. Effect begins within 5 minutes after administration. The peak effect occurs after 60-90 minutes. As a rule, it is administered along with a “long-lasting” hormone directly during meals. Drugs of this type are “Insulin Humalog”, “Novo-Rapid”, etc.
- Short. The first effect of this type of insulin occurs after half an hour. It is administered before meals. The short ones include the drugs “Monodar Humodar”, “Insulin Actrapid”.
- Medium duration. Typically used in combination with “fast” types of hormone. On its own it is able to control blood glucose concentrations for up to half a day. Preparations of this type are “Protafan” (human insulin), “Insulin Novomix”, etc.
- Long lasting hormone. It works throughout the day, but the effect occurs the longest time after administration, so it must be combined with “fast” types of the hormone. Long-term hormones include Monodar Long, Insulin Lantus, etc.
Main causes of insulin deficiency
A normal pancreas produces about 200 units of insulin per day. If its functioning is impaired, hormone synthesis can significantly decrease or stop completely. Glucose supplied with food will accumulate in the blood without being converted into glycogen, a reserve source of energy deposited in the liver and muscles. And this is a direct path to the development of diabetes.
If type I diabetes (insulin-dependent) is caused by congenital pathologies of the pancreas or autoimmune disorders, then several factors contribute to the acquisition of insulin deficiency.
- Unbalanced diet: hormone synthesis is disrupted when there is a lack of protein in the diet and when there is a deficiency of zinc, manganese and iron in the food consumed.
- Vascular atherosclerosis, in which blood circulation in the pancreas and its normal functioning deteriorate.
- Acute and chronic inflammation of the pancreas (pancreatitis).
- Disturbances in the formation of enzymes.
- Abuse of foods containing large amounts of simple carbohydrates (sweets, premium flour products).
All factors that can lead to insufficient insulin production are in one way or another related to poor nutrition. To avoid problems with the pancreas and help its normal functioning, you must follow several rules.
Foods that promote insulin production
Regular inclusion of foods that are healthy for the pancreas in your diet can normalize insulin production and become a good means of preventing diabetes. The consumption of certain products also helps to cleanse the organ of waste and toxins, which is of great importance for its full functioning.
Food products should not be considered as an alternative to medications prescribed by a doctor for the production of insulin: they do not replace drug treatment, but help maintain the functioning of the body.
Apples
Apples contain a large amount of vitamins, minerals, pectin and organic acids. The substances contained in the fruit take part in the synthesis of insulin, normalize digestion and dissolve accumulated waste deposits in the body. Experts advise taking sweet green varieties of apples.
To stimulate the pancreas, apple juice is useful, which you can drink up to three liters a day.
For people with insulin deficiency and obesity, treatment with apple cider vinegar is recommended. Thanks to fruit acids, drinking vinegar reduces cravings for sweets and breaks down fat cells, removing them from the body. Take 2 tbsp. vinegar dissolved in a glass of water 3 times a day with meals for two weeks.
Cranberry
Contains many vitamins and mineral salts. Leader in the amount of manganese among plant foods. Eating fresh or frozen berries and cranberry juice has a beneficial effect on the pancreas, improves blood circulation, normalizing its activity. It is recommended to eat 0.5 cups of berries daily or drink up to 1 liter of cranberry juice.
To prepare fruit juice with maximum preservation of all its beneficial properties, you need to mash the berries and fill them with boiled water cooled to 500 C (a glass of cranberries per 1 liter of water). Leave for 3-4 hours. Instead of sugar, you can add a little honey.
Nuts
Nuts are rich in omega-3 polyunsaturated fatty acids, which prevent vascular atherosclerosis. Together with a large amount of magnesium, manganese, protein and fiber, nuts are indispensable in the diet of patients with insulin deficiency and diabetes.
For a healing effect, it is enough to eat a handful of almonds, peanuts or walnuts daily.
Celery
The substances contained in celery help cleanse the body, prevent atherosclerosis and normalize the activity of the pancreas. If you have insulin deficiency, celery juice is useful - you need to take half a glass of it in the morning on an empty stomach. It has a beneficial effect on blood vessels, improves digestion, and activates the activity of the pancreas.
Sea kale
Seaweed is useful for insufficient insulin production. Cobalt, manganese and zinc contained in their composition prevent disturbances in the functioning of the pancreas and promote hormone synthesis.
Kelp is added to salads, cereals, vegetable dishes, or crushed dried seaweed is used instead of salt.
Oats contain valuable lipotropic components and enzymes that help improve digestion. The grain crop has excellent absorbent and detoxifying properties. Due to the cleansing effect on the body, consuming oatmeal or infusion improves the functioning of the pancreas. For medicinal purposes, only unpeeled oats are used (instant oats are practically devoid of beneficial properties).
To help the pancreas work, natural health experts advise taking oat milk.
It is prepared according to the following recipe:
- Wash 100 g of oats with running water and pour 1.5 liters of water into a saucepan.
- Place on the stove, bring to a boil and simmer for an hour over low heat.
- Grind the softened oats directly in the pan using a blender.
- Cook for another 20 minutes.
- Place the broth on a fine sieve, draining the liquid (this is medicinal oat milk).
You need to take half a glass of the decoction three times a day before meals. Store in the refrigerator for no more than two days.
How is the gland hormone formed and how does it work?
So which pancreatic cells produce insulin? Hormone synthesis is carried out by beta cells. They are also called pancreatic islets or islets of Langerhans.
The mechanism of hormone formation in the body is relatively simple. It begins to be actively produced when the amount of carbohydrates in biological fluid increases. Any food entering the stomach triggers the process of synthesis of a hormonal substance. Food can be protein, vegetable, fatty – not just carbohydrates. When a person has eaten heavily, the concentration of the hormone increases. Against the backdrop of hunger, it falls.